When you're navigating the wide world of fertility treatments, Clomid often pops up as a go-to solution. But hey, it's not the only player in town. There are several alternatives that might just be what you need. You might wonder, what else is out there? Well, brace yourself as we dive into the diverse options that can offer a fresh perspective on fertility treatments.
First up is Lupron, known scientifically as Leuprolide. It's a GnRH agonist that's been making waves in controlled stimulation during IVF protocols. Why do people go for Lupron? Often, it's because it lets them have a better grip on their treatment. Doctors combine it with FSH for this exact reason, making everything a bit more predictable during the IVF journey.
Lupron (Leuprolide)
Lupron doesn’t work alone; it's usually paired with other medications to help fine-tune ovulation control.
Pros
- High protocol success rates
- Reduces OHSS risk
- Established IVF protocol
- Flexible dosing
Cons
- Long protocol duration (3+ weeks)
- May cause menopausal side effects like hot flashes
- Requires precise timing and monitoring
- Lupron (Leuprolide)
- Letrozole
- Gonadotropins
- Metformin
- Tamoxifen
- Femara
- Ovarian Drilling
- Traditional Chinese Medicine
- Conclusion
Lupron (Leuprolide)
Diving into fertility treatments, Lupron is quite a unique option on the table. This medication, known in more technical terms as Leuprolide, is a type of GnRH agonist. What does that mean for folks trying to boost their fertility chances?
Well, GnRH agonists like Lupron work a bit like the director of an intricate play, orchestrating the timing and control in IVF protocols. It's been commonly used to suppress natural ovulation, thus allowing for more controlled ovarian stimulation.
Pros
Why might you consider Lupron? Let's break down the perks:
- High protocol success rates: Folks have seen promising results, which brings hope and confidence to many looking for fertility solutions.
- Reduces OHSS risk: Ovarian hyperstimulation syndrome can be a concern, but Lupron steps in to lower this risk, making the journey a bit smoother.
- Established IVF protocol: It's been around the block, meaning doctors are familiar, and that familiarity translates to trusted results.
- Flexible dosing: Dosing can be tweaked based on personal needs, offering room for customization in treatments.
Cons
Still on the fence? Consider these downside factors:
- Long protocol duration: Buckle up because using Lupron might mean committing to a treatment timeline of over three weeks. That’s a factor to keep in mind for anyone juggling a busy life.
- Potential menopausal side effects: Some folks might experience symptoms like hot flashes, which are manageable but could be uncomfortable.
- Precision is key: The timing and monitoring need to be spot-on, necessitating close coordination with your healthcare provider. This precise timetable might not fit everyone's schedule.
For some real numbers, let's take a quick look at a snapshot of success rates in an IVF setting:
| Factor | Success Rate |
|---|---|
| Using Lupron | Approx. 50-60% |
| Standard Protocol Without Lupron | Approx. 40-50% |
Whether you're just starting this journey or looking for the next step, Lupron offers a path worth considering. Armed with these insights, discussing options with your doctor can guide you to the best choice for your unique circumstances.
Letrozole
Ever wondered why Letrozole is causing a buzz in the fertility world these days? This breast cancer medication turned fertility enhancer is catching attention for all the right reasons. Originally developed to treat estrogen-receptor-positive breast cancer by blocking estrogen production, Letrozole inadvertently found its way into fertility treatments, offering a fresh alternative to Clomid. What's interesting is that it works by encouraging the pituitary gland to release more follicle-stimulating hormone (FSH), aiding the ovaries in producing well-developed eggs.
A significant advantage of Letrozole? It tends to have fewer side effects compared to Clomid. Women often report less thinning of the uterine lining, making implantation more successful. Plus, it's typically linked with a reduced risk of multiple pregnancies, which is always something to consider.
Pros
- Lower risk of multiple pregnancies
- Less impact on estrogen levels than Clomid
- Increased rates of ovulation for women with Polycystic Ovary Syndrome (PCOS)
- Shorter half-life compared to Clomid, reducing systemic side effects
Cons
- Off-label use, meaning it's not FDA-approved specifically for infertility
- Varies in effectiveness based on individual health conditions
- Requires precise administration and monitoring
It's fascinating to note that some studies even suggest that Letrozole may lead to higher pregnancy rates compared to Clomid, especially in women with PCOS. So if you're exploring alternatives to Clomid, Letrozole might deserve your attention due to its promising potential in fertility treatments.
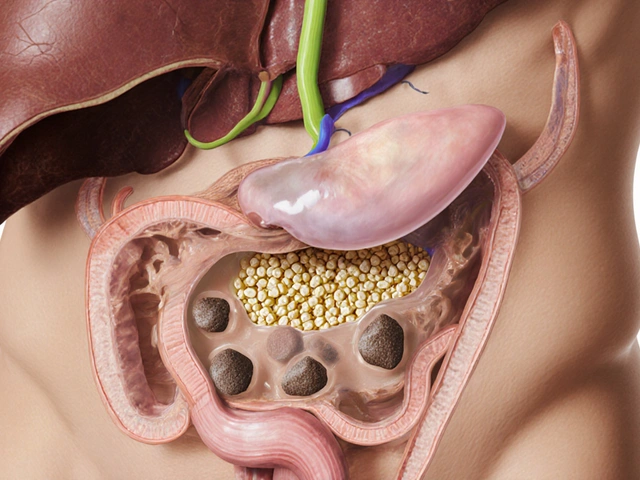
Gonadotropins
Now let’s talk about gonadotropins, another player in the quest for pregnancy. These hormones are no strangers to the fertility game, often used when treatments like Clomid or Letrozole don't quite hit the mark. Think of gonadotropins as a more direct approach, as they stimulate the ovaries to produce more eggs, increasing the chance of conception.
Gonadotropins include FSH (follicle-stimulating hormone) and LH (luteinizing hormone), which are similar to the ones naturally produced by the pituitary gland. They’re usually given through injections, which can sound a bit daunting, but many find that it's a manageable part of the process.
Pros
- Highly effective, especially when other treatments haven't worked
- Encourages the production of multiple eggs, increasing fertility chances
- Can be precisely controlled with dosage adjustments
Cons
- Requires close monitoring to avoid overstimulation
- Higher cost compared to Clomid
- Possible side effects include mood swings and bloating
Despite the higher cost and frequent doctor visits, many couples find gonadotropins to be a game-changer. They are often part of the IVF protocol, playing a crucial role in the successful maturation of multiple eggs. If you’re considering this route, be ready for regular clinic visits to ensure your hormones are playing by the rules.
| Year | Success Rate (%) |
|---|---|
| 2020 | 60 |
| 2021 | 65 |
| 2022 | 68 |
Bottom line: gonadotropins aren't the simplest fertility treatment, but they could be some of the most effective when used appropriately. Keeping open communication with your healthcare provider will be key to ensuring that this treatment is tailored to your needs.
Metformin
When it comes to alternative treatments for fertility, Metformin might just be one you've stumbled across. Traditionally used to manage diabetes, it's made its mark in the fertility world, especially for those dealing with polycystic ovary syndrome (PCOS). But how exactly does it help with fertility?
Well, Metformin improves the way your body handles insulin. For women with PCOS, insulin resistance can mess with hormone levels and make ovulation unpredictable. By tackling insulin resistance, Metformin can help level the playing field, encouraging more regular ovulation cycles. That's a big plus when you're trying to conceive.
Pros
- Makes cycles more regular
- Often improves ovulation
- Generally well-tolerated
- May also help with weight loss and reduce the risk of gestational diabetes
Cons
- Some may experience gastrointestinal side effects
- Not effective for everyone
- It may take a few months to see significant results
Also, since PCOS is so common, it's handy to know that Metformin addresses one of its root problems rather than just treating symptoms. But remember, while it's a hero to some, it's not a universal fix. It works best for specific hormone imbalances, so always chat with your healthcare provider to see if it's the right fit for you.
| Condition | Approx. Success Rate with Metformin |
|---|---|
| PCOS | 30-40% |
| Non-PCOS-related fertility issues | Lower success rate |

Tamoxifen
Stepping into the world of fertility treatments, Tamoxifen is a name you might not immediately associate with boosting fertility. It's mainly known for its role in treating and preventing breast cancer, but it has a more personal side when it comes to helping with ovulation issues.
Tamoxifen operates quite similarly to Clomid—it blocks estrogen receptors in the brain. This trickery convinces the body to crank up its natural production of hormones like FSH (Follicle Stimulating Hormone) and LH (Luteinizing Hormone), which kickstart ovulation. It's often a go-to for women who haven't responded well to Clomid.
"Tamoxifen can be a favorable alternative for women, particularly those with certain types of hormone receptor-positive cancers." — Dr. Anita Mahajan, an esteemed oncologist.
Pros
- Effective for women who are resistant to Clomid
- Potentially fewer side effects related to mood changes compared to other fertility drugs
- Lower risk of ovarian hyperstimulation syndrome (OHSS)
Cons
- Limited to certain fertility profiles
- Not suitable for women actively undergoing certain cancer treatments
- Requires close monitoring, as with all hormone-related treatments
One of the interesting stats about Tamoxifen's role in fertility is its use in cases where Clomid didn't hit the mark. Studies suggest that it provides an ovulation success rate of about 30-40% when Clomid can't pull through.
This medication stands out for its dual role—balancing as both a cancer treatment and a fertility booster. It's crucial for patients to discuss the Clomid alternatives with their healthcare provider to tailor the treatment to their unique medical history and fertility goals.
Femara
Looking for a Clomid alternative that's been picking up popularity? Say hello to Femara, also known as Letrozole. Originally intended for breast cancer treatment, this little pill has shown promise in the fertility realm by helping induce ovulation.
Femara works by blocking estrogen production, which signals the pituitary gland to crank up the production of Follicle Stimulating Hormone (FSH). This, in turn, stimulates the ovaries to produce eggs—a vital step for couples aiming for conception.
Pros
- Effective for women who are Clomid-resistant
- Lower risk of multiple births compared to Clomid
- Less thinning of the uterine lining
- Often better tolerated with fewer side effects
Femara has an edge over Clomid when it comes to reducing the chance of twins or more babies at once, which is often a concern in fertility treatments. Most women also appreciate the fewer side effects that it brings to the table, like avoiding the dreaded hot flashes or mood swings.
Cons
- Not FDA-approved specifically for fertility treatment
- Potential side effects include fatigue, dizziness, and headaches
- Less information on long-term effects than for other drugs
- May not be suitable for everyone, and dosage needs to be carefully managed
No drug is perfect though, and Femara is not FDA-approved just for fertility—not yet, anyway. Some women experience fatigue or headaches, and if you decide to try it, your doc will need to keep a close eye on the dosage and effects.
Overall, Femara can be a great option if Clomid isn't cutting it for you. Always consult with your healthcare provider for personalized advice tailored to your specific situation.
Ovarian Drilling
Ovarian drilling might sound a bit extreme, but it's actually a well-known surgical procedure used as an alternative to Clomid for women with polycystic ovary syndrome (PCOS). Curious about how it works? It's pretty straightforward. The process involves making tiny holes in the ovary using a laser or thin needle, often with the help of laparoscopy. This can restore regular ovulation by reducing male hormone levels and helping the body respond better to its own hormones.
Thinking about the key advantages? Well, one biggie is that it can lead to spontaneous ovulation without additional medication. That's a win if you're trying to avoid the roller coaster of hormonal treatments. The effects can last for up to a year, sometimes longer, providing a window for conception.
Pros
- Might help restore natural ovulation
- Reduces the need for ovulation-stimulating drugs
- Can improve insulin sensitivity
Cons
- Requires surgery, which comes with typical surgical risks
- Not a guaranteed fix for all cases of PCOS
- Effects can wear off over time
Now, let's not ignore the numbers. According to a study published in the Journal of Clinical Endocrinology & Metabolism, around 80% of women experienced resumed regular menstrual cycles post-surgery. That's pretty encouraging if you've been stuck in the frustrating cycle of irregular periods!
So, why consider ovarian drilling over medication like Clomid? It's often suggested for women who haven’t had success with medication or those looking to minimize medication use, yet still hold a chance at achieving natural fertility. Of course, discussing this option with your healthcare provider is vital. They'll help decide if it's the right path for your fertility journey.
Traditional Chinese Medicine
When thinking about fertility treatments, Western medicine isn't the only game in town. Traditional Chinese Medicine (TCM) offers a different approach, focusing on balancing the body's energy, or Qi, to enhance fertility.
In TCM, fertility issues are often seen as disruptions in energy flow. Acupuncture and herbal treatments are commonly used to restore this balance. The idea might sound abstract, but there's evidence backing it up. TCM treatments can increase blood flow to the reproductive organs, regulate menstrual cycles, and improve overall health.
Key Techniques
- Acupuncture: Tiny needles are inserted into specific points on the body. It's believed to boost circulation and release endorphins, helping with stress, which can be a big deal when you're trying to conceive.
- Chinese Herbal Medicine: Custom herbal blends are tailored to individual needs. Ingredients like ginseng, ginger, and licorice root are often included for their reputed effects on fertility.
"The integration of TCM in fertility treatments can offer a holistic approach that restores balance to the body," says Dr. Mei Tao, a respected TCM practitioner.
Pros
- Non-invasive treatment options
- Few side effects compared to pharmaceuticals
- Can be combined with Western treatments for enhanced efficacy
Cons
- Results can take time and vary among individuals
- Requires a trained practitioner for effective treatment
- Limited scientific research compared to conventional methods
A study published in the 'Journal of Integrative Medicine' notes that couples using TCM alongside IVF saw improved pregnancy rates.
Conclusion
When it comes to fertility treatments, there’s no one-size-fits-all. Isn’t it fascinating how many Clomid alternatives we have to choose from? Each treatment option offers its unique set of benefits and challenges, tailored to different needs and goals. This variety ensures that everyone can find a path that aligns with their personal and medical circumstances.
To make things clearer, let’s look at a handy table to summarize the notable points:
| Alternative | Pros | Cons |
|---|---|---|
| Lupron (Leuprolide) | High success, reduces OHSS risk | Long duration, menopausal effects |
| Letrozole | Lower side effects | Requires monitoring |
| Gonadotropins | High effectiveness | Expensive, risk of multiple births |
| Metformin | Improves insulin resistance | Gastrointestinal side effects |
| Tamoxifen | Alternative for Clomid-resistant patients | Possible blood clot risk |
| Femara | Lowered OHSS risk | May lower estrogen |
| Ovarian Drilling | Permanent solution | Invasive procedure |
| Traditional Chinese Medicine | Holistic approach | Lack of scientific validation |
Each option shines in its own way, and this flexibility is a godsend amidst the hopes and hurdles of fertility journeys. The choice of treatment really boils down to individual medical history, preferences, and consultations with healthcare providers. Exploring these alternatives gives you a better shot at finding the right fertility path, whether you're all about natural approaches or prefer established medical protocols.
Remember, the journey to starting or growing a family is personal, and having more choices means you're better equipped to find what fits best for you. It's about being informed, staying hopeful, and finding what works for you and your unique story. IVF options are varied, allowing for a highly personalized treatment plan that can be pivotal in achieving your dreams.









Clomid’s not the only game in town, and the landscape of fertility meds is way broader than most people think. Each alternative-whether it’s Lupron, Letrozole, or even a surgical option like ovarian drilling-carries its own set of pros and cons that line up differently with individual health profiles. I’d say the biggest thing is matching the drug’s mechanism to the specific issue you’re facing, like insulin resistance or anovulation. Bottom line: have a solid chat with your reproductive endocrinologist to map out which route makes sense for you.
Life is a cascade of hormones, and choosing a drug is like picking a pen for a poem you haven’t yet written.
I hear you, Joseph-hormones do feel like an abstract script sometimes. That said, the good news is there’s solid data behind many of these alternatives, not just philosophical musings. Letrozole, for example, tends to have a cleaner side‑effect profile for many women with PCOS, which can make the journey a bit less stressful. Metformin tackles the root insulin issue, so it’s a more systemic fix rather than just nudging the ovaries. And yes, grammar matters too; “Clomiphene” is the correct spelling, not “Clomid,” even though the latter is marketable shorthand. Keep the optimism alive; the right combo is out there for you.
Alright, strap in, because the world of Clomid alternatives is nothing short of a roller‑coaster ride through a pharmaceutical theme park.
First, we got Lupron, the GnRH agonist that loves to play puppet master with your pituitary, extending protocols to three weeks or more-perfect if you enjoy scheduling chaos.
Then there’s Letrozole, the breast‑cancer drug turned fertility hero, quietly boosting FSH without the dreaded uterine‑lining thinning, which is a sigh of relief for many.
Gonadotropins? Oh, they’re the heavyweight champs, delivering multiple eggs but costing a small fortune and demanding 24‑hour monitoring.
Metformin steps in for the insulin‑resistant crowd, slowly nudging regular ovulation and sometimes even helping with weight-though the GI side‑effects can be a drama on their own.
Tamoxifen, that old oncology staple, masquerades as an ovulation trigger when Clomid fails you, yet it’s not for everyone, especially those with clot‑risk concerns.
Femara (yes, that’s Letrozole’s fancy alias) offers a lower multiple‑birth risk, but beware of fatigue and headaches that can linger like unwanted party guests.
Ovarian drilling sounds like a sci‑fi plot twist, but it actually makes tiny perforations to reboot ovulation-surgery included, so bring your consent forms.
Traditional Chinese Medicine adds a holistic layer, with acupuncture and herbs that claim to balance Qi, although the evidence is still a patchwork quilt of small studies.
Each of these options carries a unique blend of efficacy, side‑effects, cost, and lifestyle impact, meaning the “best” choice is as personal as your favorite pizza topping.
Don’t forget that monitoring is crucial-whether you’re on Lupron’s long protocol or the rapid‑fire Gonadotropins, your doctor’s office will become your second home.
And while the jargon can feel overwhelming-FSH, LH, GnRH, OHSS-just remember: they’re just letters describing real physiological pathways you’re trying to fine‑tune.
Bottom line, the fertility journey isn’t a one‑size‑fits‑all; it’s a nuanced dance between biology, medication, and personal preference.
So pick your partner wisely, keep communication open with your care team, and never underestimate the power of a supportive community to keep you motivated.
Good luck out there, and may your egg‑hunting adventures end in a happy “conception” finale!
From a strategic standpoint, the decision matrix for Clomid alternatives reads like a high‑level boardroom discussion-risk assessment, cost‑benefit analysis, and protocol scalability are all on the table. Lupron offers robust OHSS mitigation but demands an extended timeline, which can clash with personal schedules. Letrozole shines in PCOS cohorts, delivering comparable pregnancy rates with fewer multiple gestations, a point worth noting for clinicians managing twin‑risk budgets. Gonadotropins deliver peak efficacy at a premium price point, making them the go‑to for IVF power‑lifting cycles. Metformin provides a metabolic advantage for insulin‑resistant patients, though its delayed onset requires patience. Tamoxifen and Femara serve niche Clomid‑resistant populations, each with distinct side‑effect spectrums that must be weighed. Surgical ovarian drilling offers a drug‑free ovulation trigger, but the invasive nature limits its appeal. Finally, integrate Traditional Chinese Medicine judiciously as an adjunct therapy, acknowledging the limited yet promising data on synergistic outcomes. Align these variables with patient goals, and you’ll navigate the fertility maze with a clearer, data‑driven compass.