Understanding Panic Disorder: The Basics
Before diving into the science behind panic disorder, it's essential to first understand what panic disorder is. Panic disorder is characterized by recurrent, unexpected panic attacks, which are sudden episodes of intense fear or discomfort that peak within minutes. These panic attacks can be accompanied by physical symptoms such as rapid heart rate, shortness of breath, chest pain, and dizziness. They can also involve feelings of impending doom, fear of losing control, or fear of dying.
Panic disorder can significantly impact a person's life, interfering with their daily activities, relationships, and overall quality of life. While panic disorder can be a debilitating condition, it's important to remember that it's treatable and many people find relief through therapy, medication, or a combination of both. Now that we have a basic understanding of panic disorder, let's explore the science behind what's happening in the brain during a panic attack.
The Role of the Amygdala in Panic Disorder
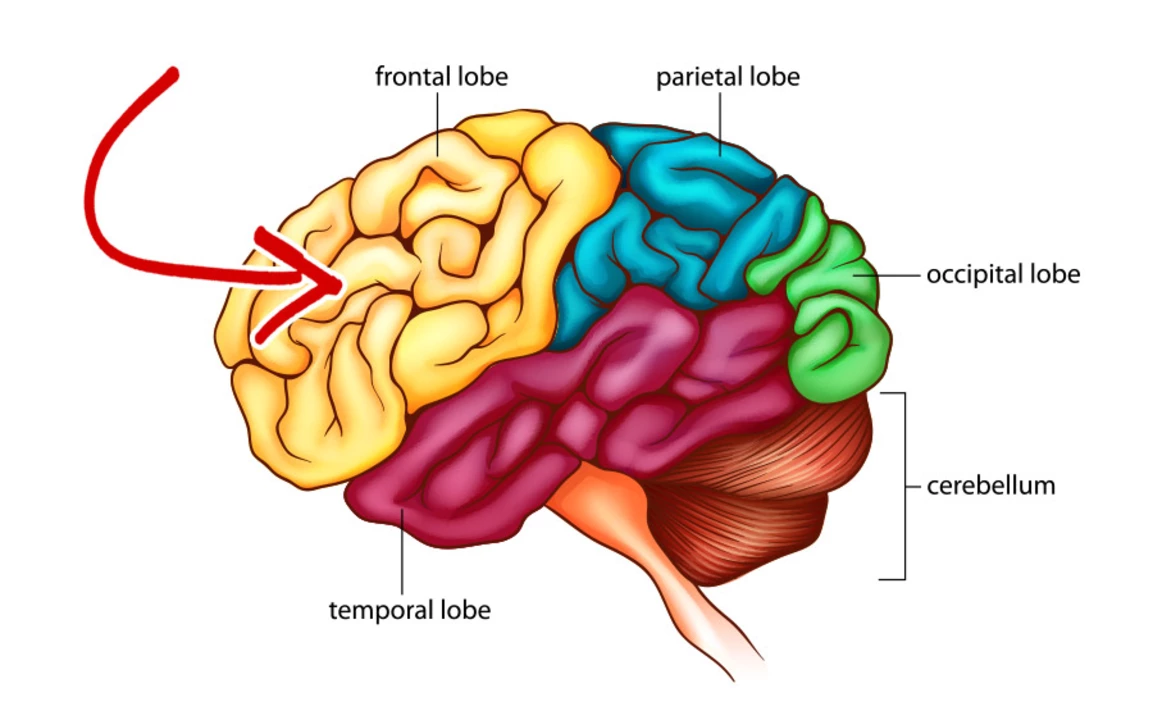
The amygdala is a small, almond-shaped structure located deep within the brain that plays a crucial role in processing emotions, particularly fear-related ones. Research has shown that the amygdala is hyperactive in individuals with panic disorder, making them more sensitive to potential threats and more likely to experience panic attacks.
During a panic attack, the amygdala sends signals to other parts of the brain responsible for the "fight or flight" response, triggering a cascade of physical and emotional symptoms. This heightened sensitivity to fear and anxiety may be due to genetic factors, learned behaviors, or a combination of both. Understanding the role of the amygdala in panic disorder helps to shed light on why some people are more susceptible to panic attacks than others.
Neurotransmitter Imbalances and Panic Disorder
Neurotransmitters are chemical messengers in the brain that play a vital role in regulating mood, behavior, and overall brain function. Imbalances in neurotransmitter levels have been implicated in various mental health disorders, including panic disorder. Two neurotransmitters, in particular, have been linked to panic disorder: serotonin and norepinephrine.
Serotonin is often referred to as the "feel-good" neurotransmitter because it helps to regulate mood, sleep, and appetite. Low levels of serotonin have been associated with depression and anxiety disorders, including panic disorder. Norepinephrine is involved in the body's stress response, and dysregulation of this neurotransmitter has been implicated in panic disorder as well. Medications that target these neurotransmitters, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), are often prescribed to treat panic disorder and help to restore balance in the brain.
Hyperventilation and the Vicious Cycle of Panic
During a panic attack, individuals often experience hyperventilation, which is rapid and shallow breathing. This type of breathing can lead to an imbalance of oxygen and carbon dioxide in the body, causing symptoms such as dizziness, lightheadedness, and shortness of breath. These physical sensations can then exacerbate the feelings of panic and anxiety, creating a vicious cycle of panic.
One of the most effective ways to break this cycle is through deep, slow breathing exercises. By consciously focusing on their breath and slowing it down, individuals can help to restore balance in their body and interrupt the cycle of panic. This is a key component of many cognitive-behavioral therapy (CBT) techniques for treating panic disorder, which we'll discuss further in the next section.
Cognitive-Behavioral Therapy and Panic Disorder
Cognitive-behavioral therapy (CBT) is a widely used and evidence-based treatment for panic disorder. CBT focuses on identifying and challenging negative thought patterns and behaviors that contribute to panic attacks. By addressing these underlying factors, individuals can learn to manage their panic disorder more effectively.
CBT techniques for panic disorder often include deep breathing exercises, progressive muscle relaxation, and exposure therapy, which involves gradually confronting feared situations or sensations in a controlled environment. Through these techniques, individuals can learn to better understand their panic symptoms, build coping skills, and ultimately reduce the frequency and severity of their panic attacks.
Medications for Panic Disorder: How They Work
Medications can also be an effective treatment for panic disorder, particularly when combined with therapy. As mentioned earlier, selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are commonly prescribed for panic disorder. These medications work by increasing the availability of serotonin and/or norepinephrine in the brain, helping to restore balance and improve mood and anxiety symptoms.
In addition to these medications, benzodiazepines may be prescribed for short-term relief of panic symptoms. These medications work by enhancing the effects of a neurotransmitter called gamma-aminobutyric acid (GABA), which helps to reduce anxiety and promote relaxation. However, benzodiazepines should be used with caution due to their potential for dependence and withdrawal symptoms. It's important to work closely with a healthcare provider to find the right medication and treatment approach for each individual's unique needs.







The cascade of neurochemical fireworks in a panic attack feels like a storm raging inside a tiny glass jar; the amygdala blares the alarm, serotonin whispers doubts, and norepinephrine drags you into a frantic dance. You can picture the hyperactive amygdala as a faulty fire alarm that refuses to quiet down even when the kitchen is cool. Then the breath shortens, CO₂ levels dip, and the brain misreads the lack of carbon dioxide as suffocation. The result is that the body launches a full‑blown fight‑or‑flight response, heart pounding like a drum in a marching band. Meanwhile, the prefrontal cortex, which should be the rational commander, gets drowned out by the noise. This neuro‑imbalance explains why you might feel an urge to flee even when there's no danger. The literature points to serotonin deficits, which is why SSRIs often help smooth the turbulence. Norepinephrine spikes amplify the heart rate, making the chest feel like a hammer. Add to that the tendency to hyperventilate, and you get dizziness that fuels the fear loop. Breaking the cycle with controlled breathing is like turning down the volume on that alarm – the brain finally hears the silence. Cognitive‑behavioral therapy teaches you to rewrite the script, challenging the catastrophic thoughts that the amygdala fuels. Exposure exercises act as rehearsals, letting the nervous system learn that the feared scenario isn’t actually lethal. Medication can act as a temporary crutch, stabilizing neurotransmitter levels while therapy does the heavy lifting. It’s a delicate ballet between chemistry and cognition, and both sides need to be in sync for lasting relief. Remember, the brain is plastic; with consistent practice, those stormy patterns can be rewired into calmer seas.
Wow, that breakdown really shows how interconnected everything is; keep focusing on those breathing exercises and CBT techniques, they’ll make a huge difference.
the amygdala basically acts like an over‑eager watchdog that barks at every little thing and never learns to chill out.
Exactly, it's like the watchdog is set on high alert, constantly scanning for threats, which can lead to that exhausting cycle of fear, anxiety, and physical symptoms, especially when the brain's chemistry is out of balance, and that's why therapies that target both mind and body work so well, because they help reset that overactive alarm system.
Breathing slowly can actually calm the nervous system.
In many cultures we teach kids simple breath control from a young age, like counting breaths or humming, which can be a natural guard against panic, so adding a bit of that tradition into daily routine might help ease the amygdala's over‑reaction.
Indeed, incorporating traditional breathing practices can complement modern therapies and provide a holistic approach to managing panic symptoms.
Man, when the brain lights up like a fireworks show during a panic attack, it's like the entire universe decides to explode inside your chest!
The dramatic description is entertaining, but it oversimplifies the nuanced neurobiology and may mislead readers about the actual mechanisms involved.