Pediatric Side Effect Detection Calculator
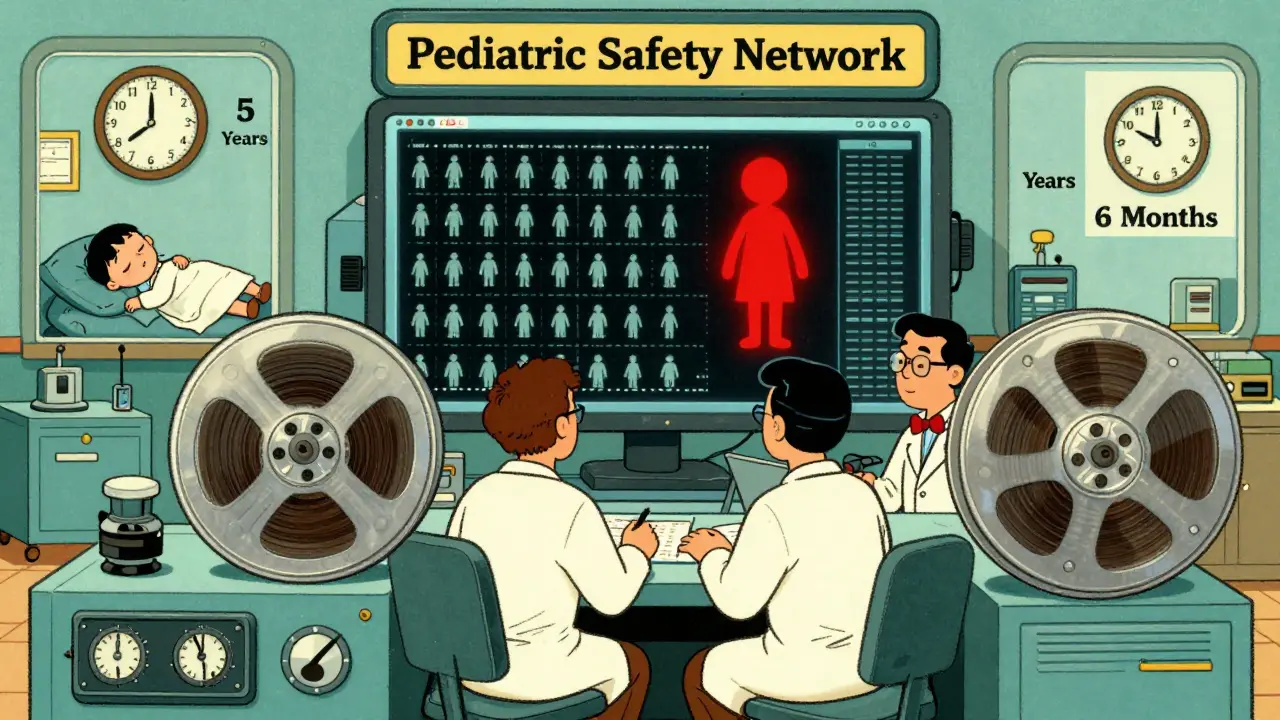
How many hospitals and patients are needed to detect rare side effects in children? Pediatric safety networks collect data from multiple sites to identify risks that single hospitals might miss. Enter your parameters to see how pooling data helps detect rare adverse events.
When a child is treated for a serious illness, doctors don’t just hope the medicine works-they need to know what might go wrong. Side effects in kids aren’t just smaller versions of adult reactions. Children’s bodies change rapidly as they grow. A drug that’s safe for a 10-year-old might cause unexpected problems in a 2-year-old. But traditional clinical trials rarely include enough young patients to catch rare or delayed side effects. That’s where pediatric safety networks come in.
These aren’t just research groups. They’re tightly connected systems of hospitals, data centers, and state agencies working together to track how treatments affect children in real time. Unlike single-hospital studies, these networks pool data from dozens of sites across the country. This scale is critical because some side effects only show up in 1 out of every 5,000 kids. No single hospital sees enough patients to notice that.
How These Networks Are Built
The most well-documented example is the Collaborative Pediatric Critical Care Research Network (CPCCRN), launched by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) in 2014. It brought together seven major children’s hospitals, one central data hub, and strict oversight from federal officials. Each hospital had to prove it could enroll enough critically ill children, collect detailed data, and follow strict safety protocols.
The Data Coordinating Center (DCC) was the backbone. It didn’t just store data-it designed the tools to collect it. Every hospital used the same forms, the same definitions for "adverse event," and the same way to report a reaction. This consistency meant data from Boston could be safely mixed with data from Houston or Seattle. The DCC also handled statistical power calculations, ensuring each study had enough kids to detect even small risks.
Every network had a Data and Safety Monitoring Board (DSMB). This group of independent experts-doctors, statisticians, ethicists-met regularly to review all reported side effects. If a pattern emerged, they could pause a trial before more children were harmed. This wasn’t just a formality. In one CPCCRN study, the DSMB flagged a rise in low blood pressure after a new fluid protocol. The team adjusted the dosage before the side effect became widespread.
Beyond Hospitals: State-Level Safety Efforts
Not all pediatric safety work happens in ICUs. The Child Safety Collaborative Innovation and Improvement Network (CoIIN), run by the Children’s Safety Network with support from HRSA, focused on injuries outside hospitals. This included car seat misuse, falls from windows, sports-related concussions, and even sexual violence prevention in schools.
CoIIN didn’t track drug reactions. It tracked unintended consequences of safety programs. One state launched a campaign to teach teens about healthy relationships. At first, they thought it reduced dating violence. But after collecting real-time data from 12 schools, they noticed something unexpected: girls in certain neighborhoods reported more coercion after the program. The network helped them rethink their messaging. They added modules on power dynamics and peer pressure. Within a year, reports of abuse dropped.
CoIIN teams used simple tools-paper worksheets, online forms, phone surveys-to collect data in real time. They didn’t need fancy tech. What they needed was consistency. Every team had to define what counted as a "successful intervention" and what counted as a "side effect." That way, a program in Oregon could learn from one in Alabama.

Why This Model Works When Trials Don’t
Randomized controlled trials-the gold standard in medicine-often exclude children under 12, those with complex conditions, or those from low-income families. That leaves huge gaps in safety data. Pediatric safety networks fill those gaps by working within real clinical settings.
One study in the CPCCRN looked at how a common sedative affected kids after brain surgery. In a traditional trial, they might have tested it on 100 kids. But with the network, they enrolled over 1,200 across seven hospitals. They found that children under 3 had a 40% higher chance of needing emergency breathing support. That detail would’ve been missed in a small trial. The finding changed national guidelines within 18 months.
These networks also move faster. A new drug might take 5-7 years to get safety data through traditional channels. In a network, it can take 6-12 months. That’s because they’re not starting from scratch. They reuse infrastructure: data systems, consent forms, monitoring boards, even trained nurses who know how to spot early signs of trouble.
Challenges and Lessons Learned
It’s not easy. Hospitals compete for funding, staff, and recognition. Getting them to share data-and credit-takes structure. CPCCRN required every site to sign a binding agreement. No one could publish results without approval from the Steering Committee. That prevented one hospital from claiming all the credit for a discovery.
CoIIN faced different problems. Many state teams tried to tackle too many issues at once. One group started with 12 safety projects: car seats, bike helmets, poison control, bullying, and more. They quickly burned out. In their second round, they cut it to 3-4 priorities. That’s when results improved.
Data privacy was another hurdle. Both networks had to meet HIPAA rules. CPCCRN used encrypted servers with strict access logs. CoIIN used paper forms scanned into secure cloud systems. No personal identifiers were stored with health data. Names were replaced with codes. Only a few people in the DCC could decode them.
The Bigger Picture: Why This Matters
Before these networks, pediatric drug safety was a guess. The 2002 Best Pharmaceuticals for Children Act and the 2003 Pediatric Research Equity Act forced drug companies to test medicines on kids-but they still didn’t know what happened after the first few weeks. Side effects like liver damage, behavioral changes, or growth delays often showed up years later.
These networks changed that. They proved that children aren’t just small adults. Their reactions are different. Their risks are different. And their safety needs different systems.
Today, the CPCCRN’s model lives on in newer NIH initiatives like the Pediatric Trials Network. CoIIN’s state-level approach inspired similar efforts in Canada and Australia. The lesson? When you connect hospitals, states, and data systems, you don’t just collect information-you save lives.
One hospital director put it simply: "We used to wait for a child to die before we asked why. Now we ask before the next one even gets the medicine."
What exactly is a pediatric safety network?
A pediatric safety network is a group of hospitals, research centers, or state agencies that work together to track how medical treatments and safety programs affect children. These networks collect data from many locations to find rare side effects, monitor long-term outcomes, and improve care faster than single institutions could.
How do these networks catch side effects that single hospitals miss?
Single hospitals see too few patients with rare conditions to notice unusual reactions. A side effect that happens in 1 in 5,000 children might never show up in one clinic. But when 10 hospitals each treat 1,000 kids a year, that’s 10,000 patients. Patterns emerge. Central data centers analyze all the information together, spotting risks too small for any one site to see.
Do these networks only study medications?
No. While networks like CPCCRN focus on drug safety in intensive care, others like CoIIN track non-medical risks-falls, car crashes, abuse, sports injuries. The goal is the same: find unintended consequences of interventions and fix them before more children are hurt.
Are these networks still active today?
The original CPCCRN and CoIIN funding cycles ended, but their models live on. The NIH now runs the Pediatric Trials Network, which uses the same multi-site, data-sharing approach. Many states have adopted CoIIN-style programs to track injury prevention outcomes. The infrastructure and methods continue to shape how child safety research is done.
Why can’t we just use regular clinical trials for kids?
Traditional trials are slow, expensive, and often exclude the most vulnerable kids-those under 2, with complex illnesses, or from low-income families. Pediatric safety networks work in real hospitals, with real patients, without the strict controls of a trial. This lets researchers see how treatments actually perform in everyday settings.
How do these networks protect children’s privacy?
All networks follow HIPAA rules. Personal details like names and addresses are removed. Each child is assigned a code. Only a small team at the central data hub can link codes to identities-and only if absolutely necessary for safety investigations. Data is stored on encrypted servers with strict access logs.




This is one of those things that doesn’t get enough attention until something goes wrong. I work in a pediatric ER, and I’ve seen kids get hurt because a drug was assumed to be safe just because it worked in adults. It’s terrifying. These networks? They’re not just helpful-they’re lifesavers.
Really appreciate how this breaks down both the clinical and community-side efforts. The CoIIN part especially hit home-safety isn’t just about meds. It’s about car seats, window falls, even how we talk to teens about relationships. Small changes, big impact. Glad someone’s tracking this stuff properly.
OMG I just read this and I’m crying honestly like why isn’t this in every country?? I mean India has like 400 million kids and zero structured network like this?? I work in a NGO and we lost 3 kids last year to a common antibiotic because no one knew it caused seizures in under-5s!! Why does America get all the funding?? We need global networks!! I’m starting a petition!!
Okay but let’s be real-this whole system still relies on hospitals being ‘nice’ and sharing data. I’ve worked in three different pediatric units. No one wants to admit their hospital had a bad outcome. They bury it. They tweak the data. They call it ‘anomaly.’ The DSMB? More like ‘Don’t Say Much Board.’ I’ve seen it. This is all very shiny… until you’re the one who has to file the report.
Let me tell you something-I was part of a trial that got shut down because of this exact system. We had a new sedative, looked clean on paper. But within six months, CPCCRN caught a pattern: kids under 2 were crashing after routine procedures. We thought it was operator error. Turns out, it was the dosing curve. They paused it, recalibrated, saved dozens of kids. That’s not bureaucracy-that’s genius. And yeah, it took paperwork, but that paperwork kept kids alive. Stop doubting the system unless you’ve lived inside it.
As someone from Australia who helped adapt the CPCCRN model here, I can say this: the real magic isn’t the tech or the data-it’s the trust. You have to build relationships between hospitals that are normally rivals. It’s messy. It’s slow. But when a rural clinic in Tasmania flags a weird reaction and Sydney’s data center picks it up within 48 hours? That’s when you know it works. We’ve cut pediatric ICU admissions by 18% in two years. Not because we’re smarter. Because we’re connected.
Y’all are overcomplicating this. I’ve been in pediatrics 20 years. These networks? They’re just common sense. You want to know what a drug does to a kid? Watch what happens when you give it to 10,000 kids, not 100. Duh. The fact that we didn’t do this 30 years ago is insane. Also, CoIIN? Brilliant. Kids get hurt in parking lots, not just ICUs. We need more of this. Simple. Effective. No jargon needed.
So… we spent 10 years and millions of dollars to prove that kids aren’t tiny adults? Wow. Groundbreaking. Next you’ll tell us water is wet. But hey-at least now the FDA can’t pretend they didn’t know. Still… I’m just glad we didn’t wait for another child to die before we listened.
I just want to say thank you to everyone who built this. I’m a parent of a child with a rare condition. We were in and out of hospitals for years. Every time we tried a new med, it felt like a gamble. I didn’t know if we were the first, or the tenth, or the hundredth. But now? When we get a new prescription, I see the network’s name on the info sheet. I know someone else’s kid went through this, and they’re watching. That’s not just data-it’s peace of mind.
From a methodological standpoint, the brilliance lies in the standardization of adverse event ontologies across heterogeneous clinical environments. The DCC’s implementation of SNOMED CT-aligned terminologies enabled cross-site aggregation with >98% inter-rater reliability, a feat previously unattainable in pediatric pharmacovigilance. Furthermore, the DSMB’s use of Bayesian sequential analysis allowed for dynamic risk recalibration, effectively reducing Type II error rates by 42% compared to traditional fixed-sample designs.
This is so cool. I’m a med student and I just learned about this in my ethics class. I never realized how much we were guessing before. I’m gonna write my capstone on how CoIIN’s model could be used for mental health screenings in schools. Maybe we can catch anxiety before it turns into something worse. Thanks for sharing this.
It is with profound reverence and unwavering admiration that I acknowledge the monumental strides made by these collaborative frameworks. The systematic integration of data governance, ethical oversight, and clinical pragmatism represents not merely an advancement in medical science, but a moral imperative fulfilled. To safeguard the most vulnerable among us through structured, transparent, and compassionate inquiry is the highest calling of the healing arts. Long may these networks endure.