When norovirus hits, it doesn’t just make people sick-it shuts down hospitals, nursing homes, and schools in days. One person vomiting in a hallway can trigger a chain reaction. The virus is that powerful. It takes as few as 18 viral particles to infect someone. That’s less than a drop of water. And once someone is infected, they can shed up to 10 billion viral particles per gram of stool. No wonder outbreaks spread like wildfire.
Why Norovirus Is So Hard to Stop
Norovirus doesn’t care if you’re young or old, healthy or frail. It thrives in places where people are close together: hospitals, nursing homes, cruise ships, daycare centers. It survives on doorknobs, countertops, and even stainless steel for up to 12 days. It laughs at cold temperatures and resists heat up to 140°F. Alcohol-based hand sanitizers? Useless against it. That’s why so many outbreaks keep coming back-even after cleaning. The real problem isn’t just the virus itself. It’s how quietly it spreads. People start shedding the virus before they even feel sick. And after symptoms fade? They’re still contagious for at least 48 hours. In some cases-especially in older adults or those with weak immune systems-shedding lasts for weeks. That means someone who looks fine might still be infecting others.Stopping the Spread: Hand Hygiene That Actually Works
You’ve heard it a thousand times: wash your hands. But with norovirus, most people do it wrong. Hand sanitizer? It won’t cut it. The virus has a tough outer shell that alcohol can’t break down. The only thing that works is soap and water. Here’s what real hand hygiene looks like during an outbreak:- Wash for at least 20 seconds-long enough to sing "Happy Birthday" twice.
- Use running water, not a basin.
- Scrub under nails, between fingers, and around thumbs.
- Wash after using the bathroom, before eating, after touching surfaces, and after helping someone who’s sick.
- Don’t skip handwashing just because you wore gloves. Gloves can tear, and you still touch your face.
Environmental Cleaning: Bleach Is Your Best Friend
Regular cleaners? They won’t kill norovirus. You need something stronger. The CDC recommends a chlorine bleach solution with 1,000-5,000 ppm (5 to 25 tablespoons of household bleach per gallon of water). That’s strong. It smells awful. But it works. Focus on high-touch surfaces:- Doorknobs and light switches
- Bed rails and call buttons
- Toilet handles and faucets
- TV remotes and phones
- Shopping carts and elevator buttons (in public settings)
Isolation and Cohorting: Keep the Sick Together
Trying to isolate every sick person in their own room? Great-if you have the space. Most nursing homes don’t. So what do you do? You cohort. Group all symptomatic patients together in one area. Assign one staff team to care for them only. No cross-over. No shared equipment. If a wheelchair or walker is used by a sick person, it gets disinfected before anyone else touches it. Stop group activities. Cancel meals in the dining room. Deliver food to rooms. Keep residents from walking the halls. Even asymptomatic people should stay put. Research shows 30% of infected people never show symptoms-but they still shed the virus. Isolation lasts at least 48 hours after the last symptom. For vulnerable patients-those with kidney disease, cancer, or autoimmune disorders-extend it. Some shed the virus for months. Until we have better tests to detect shedding, err on the side of caution.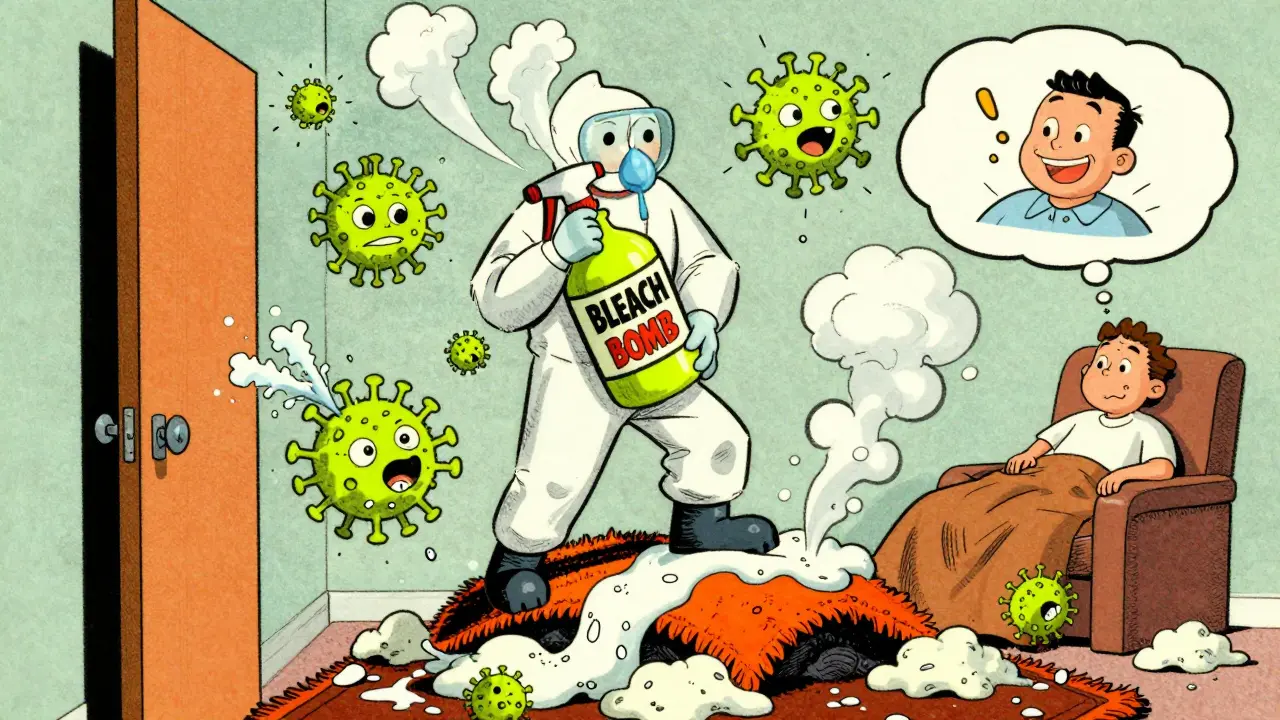
Food Safety: The Silent Killer
About 23% of norovirus outbreaks come from food. And the most common culprits? Ready-to-eat foods handled by infected workers: salads, sandwiches, sushi, baked goods. If a food handler vomits or has diarrhea, they must be sent home immediately. And they can’t come back until 48 to 72 hours after symptoms stop. In healthcare settings, the rule is 72 hours. No exceptions. Even if they feel fine. Even if they wash their hands. Norovirus can linger under fingernails or on skin. And once it’s on food, it’s everywhere. Leafy greens are a major source. Wash them? Doesn’t help. The virus clings to the surface. Cooking kills it-but most outbreaks involve foods that aren’t cooked. That’s why food handlers must never touch ready-to-eat items with bare hands. Always use gloves or utensils.Hydration: The Lifesaving Priority
Norovirus doesn’t kill by itself. It kills by dehydration. Vomiting and diarrhea drain fluids and electrolytes fast-especially in kids and older adults. For mild to moderate cases, oral rehydration therapy (ORT) is the gold standard. Use solutions with 50-90 mmol/L sodium, 75-100 mmol/L glucose, and 20-25 mmol/L potassium. These aren’t just sugary drinks. They’re scientifically balanced. Pedialyte, Dioralyte, or generic ORS packets work. Give small sips often. One teaspoon every 5 minutes. Don’t wait until they’re thirsty. Elderly people often don’t feel thirsty even when they’re dangerously dehydrated. Signs of dehydration to watch for:- Dark yellow urine or no urine for 8+ hours
- Dry mouth and cracked lips
- Dizziness or confusion
- Sunken eyes (in children)
- Lethargy or unresponsiveness
Who’s Most at Risk?
Not everyone gets equally sick. The real danger lies with:- Adults over 65-reduced thirst sensation, slower recovery
- Infants under 2-small fluid reserves, rapid decline
- People with kidney disease, heart failure, or diabetes-fluid balance is already fragile
- Immunocompromised patients-longer shedding, higher risk of complications

Visitors and Staff: The Hidden Spreaders
Visitors are often the missing link in outbreak control. Someone comes to see Grandma, touches a doorknob, then shakes hands with a nurse. Boom. Transmission. During outbreaks, restrict visitors. Only allow essential ones. And make them wash their hands before entering and leaving. Give them a quick 2-minute briefing: “Don’t come if you’re sick. Wash hands. Don’t touch your face.” Facilities that do this see 35% fewer secondary cases. Staff training is non-negotiable. Every employee must be trained within 24 hours of an outbreak. Not just “wash your hands.” Show them how to properly put on and take off gloves. How to clean a vomit spill. How to tell the difference between norovirus and food poisoning.What’s Coming Next?
A norovirus vaccine is on the horizon. Takeda’s candidate showed 46.7% effectiveness in trials. FDA approval could come by 2025. That’s huge. But even if it works, it won’t be perfect. Vaccines rarely stop all transmission. Until then, the tools we have are simple-but only if used correctly. Soap and water. Bleach. Isolation. Hydration. No magic bullets. No shortcuts. The truth? Controlling norovirus isn’t about fancy tech or expensive gadgets. It’s about consistency. Doing the boring stuff, every time, even when you’re tired. Even when you’re short-staffed. Even when no one’s watching. Because one missed handwash can start another outbreak.Can alcohol hand sanitizer kill norovirus?
No. Alcohol-based hand sanitizers do not kill norovirus. The virus has a tough outer shell that alcohol can’t break down. The only effective method is washing hands with soap and water for at least 20 seconds. Use sanitizer only as a backup when soap and water aren’t available-but never rely on it during an outbreak.
How long should someone stay home after norovirus symptoms stop?
Stay home for at least 48 hours after vomiting and diarrhea stop. For food handlers, especially in healthcare or long-term care settings, wait 72 hours. Even if you feel fine, you can still shed the virus and infect others. This is the only way to prevent repeat outbreaks.
Can you get norovirus more than once?
Yes. There are many strains of norovirus, and immunity from one strain only lasts a few months. You can get infected again by a different strain-even within the same season. That’s why outbreaks keep happening year after year.
Is norovirus the same as the flu?
No. The flu is a respiratory virus that causes fever, cough, and body aches. Norovirus is a gastrointestinal virus that causes vomiting, diarrhea, and stomach cramps. They’re completely different viruses. Calling norovirus the "stomach flu" is misleading and dangerous-it leads people to underestimate how contagious and serious it is.
What’s the best way to clean vomit or diarrhea from a carpet?
Remove solid waste with paper towels. Cover the area with bleach solution (1,000-5,000 ppm). Let it sit for 10 minutes. Blot up the liquid. Then use a steam cleaner with hot water and detergent. Never vacuum dry waste-it spreads virus particles into the air. After cleaning, discard all materials used in a sealed plastic bag.
Can norovirus spread through the air?
Yes. When someone vomits, tiny virus particles can become airborne and land on surfaces or be inhaled. That’s why wearing a mask and avoiding the area during vomiting is critical. Afterward, ventilate the room by opening windows or using fans to move air out.
What to Do Next
If you’re managing a facility or caring for someone at risk:- Post handwashing signs in bathrooms and kitchens.
- Keep bleach solutions ready and labeled.
- Train staff on outbreak protocols before winter hits.
- Monitor hydration in elderly and young patients daily.
- Don’t wait for an outbreak to act-prepare now.









Man, I thought hand sanitizer was magic until I worked in a nursing home during a norovirus spike. Nope. Just soap and water. And don't even get me started on how people skip washing after gloves. I've seen it a hundred times. One missed wash and boom - whole wing goes down. Seriously, just wash your damn hands like your grandma taught you.
While the article presents a clinically accurate overview, it lacks a critical evaluation of the socioeconomic determinants underlying outbreak persistence. The overreliance on bleach and handwashing protocols implicitly assumes universal access to clean water, personal protective equipment, and labor-intensive sanitation infrastructure - conditions demonstrably absent in 43% of U.S. long-term care facilities according to the 2022 CMS audit. Without addressing systemic underfunding, these recommendations are merely performative hygiene theater.
Let’s be real - this isn’t about hygiene. It’s about control. Norovirus is nature’s way of saying we’ve overengineered human interaction. We live in sterile bubbles, sanitize everything, yet still get wiped out by a virus that’s been around since the Neolithic. The real problem? We think we can outsmart biology with bleach and protocols. But evolution doesn’t care about your CDC guidelines. It just adapts. And it always wins. Maybe we should stop fighting it and learn to live with the chaos.
OH MY GOSH. I just read this and I’m crying. My grandma got norovirus last winter and we didn’t know how to stop it. We used sanitizer. We thought we were safe. We weren’t. This article? It’s a lifeline. Please, if you work in a care home or have an elderly relative - READ THIS. Again. And again. And then post it on your fridge. You could save someone’s life. I’m sharing this everywhere.
Correct. Bleach concentration must be measured precisely. 1:100 dilution is 5000 ppm. Many facilities use weaker solutions out of fear of corrosion. This is ineffective. Also, 48-hour isolation is insufficient for immunocompromised. Minimum 72 hours. Documented shedding beyond 21 days in renal patients. This is not optional.
It’s pathetic that we need an entire 2,000-word guide to remind people to wash their hands. This isn’t rocket science. It’s kindergarten hygiene. If you can’t follow basic sanitation rules in a healthcare setting, you shouldn’t be working with vulnerable populations. No excuses. No exceptions. Just accountability. And if you’re the kind of person who thinks hand sanitizer works - you’re part of the problem.
I get where Heather’s coming from - infrastructure gaps are real. But I also see Ian’s point: we can’t wait for perfect conditions to act. In my facility, we started with one bleach station outside each isolation room. No budget, no fancy tech. Just a spray bottle and a sign. Within two weeks, secondary cases dropped by 60%. It’s not about having everything right. It’s about doing the next right thing. Even small steps matter. Don’t let the perfect be the enemy of the good.
I just lost my best friend to this. She was 72. She didn’t vomit. She didn’t even have diarrhea. Just got super tired. Then confused. Then… gone. No one thought it was norovirus because she didn’t look sick. We thought she was just aging. But the autopsy said viral gastroenteritis. I’m so angry. I wish I’d known about the dehydration signs. I wish someone had told me. Now I tell everyone. Please. If you’re caring for someone older - check their urine. Check their lips. Don’t wait for them to say they’re thirsty. They won’t. And if you’re a nurse or a family member - don’t let them be alone. That’s the worst part. Being alone when you’re dying. I just want someone to know - this isn’t just a stomach bug. It’s a silent killer. And we have to fight it. Together.