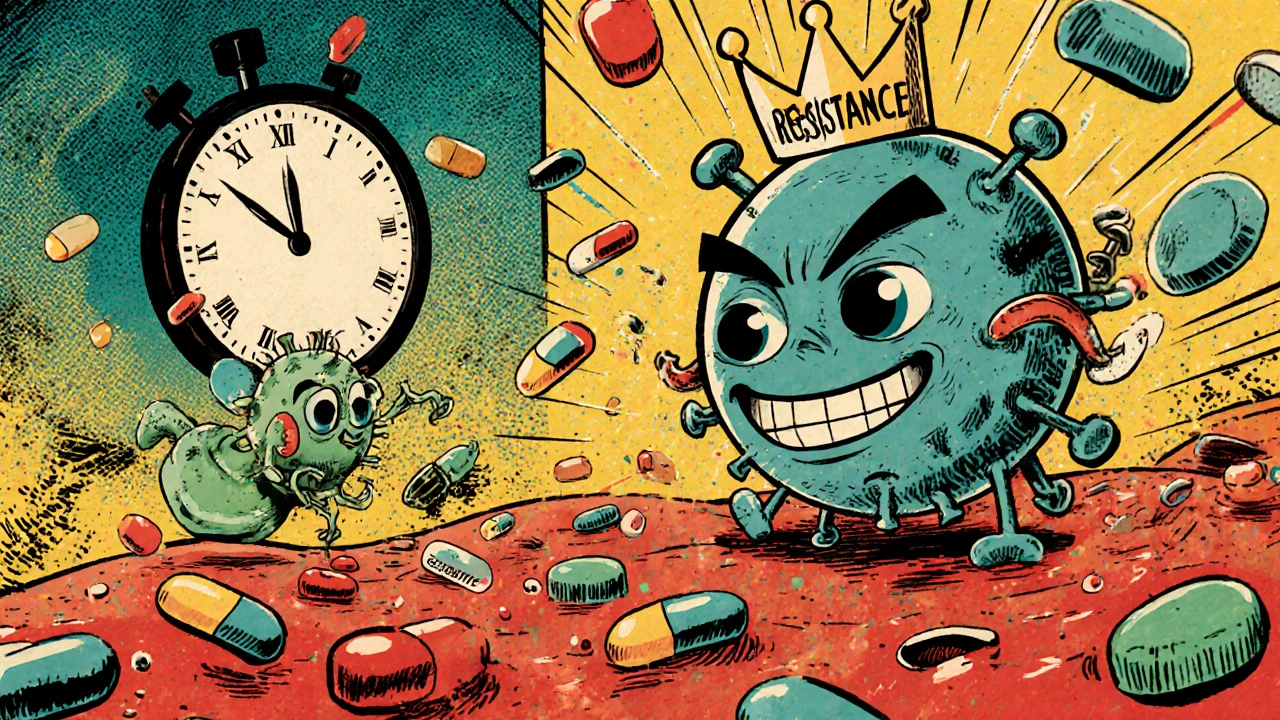
When you take an antiviral, you’re not just fighting a virus-you’re in a high-stakes race against evolution. Viruses don’t sit still. They mutate. And if you miss a dose, skip a day, or stop early, you might just give them the edge they need to survive-and become resistant. This isn’t science fiction. It’s happening right now, in real people, with real drugs.
How Antiviral Resistance Actually Happens
Antiviral resistance isn’t magic. It’s biology. Every time a virus replicates, it makes copies of itself. But it’s sloppy. Tiny errors creep in-mutations. Most of these changes do nothing. Some hurt the virus. But occasionally, one lets the virus laugh off the drug you’re taking.
This isn’t rare. In the 1980s, HIV patients on early monotherapy with AZT started seeing their viral loads bounce back. Why? The virus mutated. By 1989, resistance was common. Today, we see the same pattern with hepatitis B, herpes, and even flu. The key? Low genetic barrier drugs. These are the ones that need just one or two mutations to become useless. Lamivudine for hepatitis B? Up to 70% of people develop resistance after five years. That’s why doctors rarely use it alone anymore.
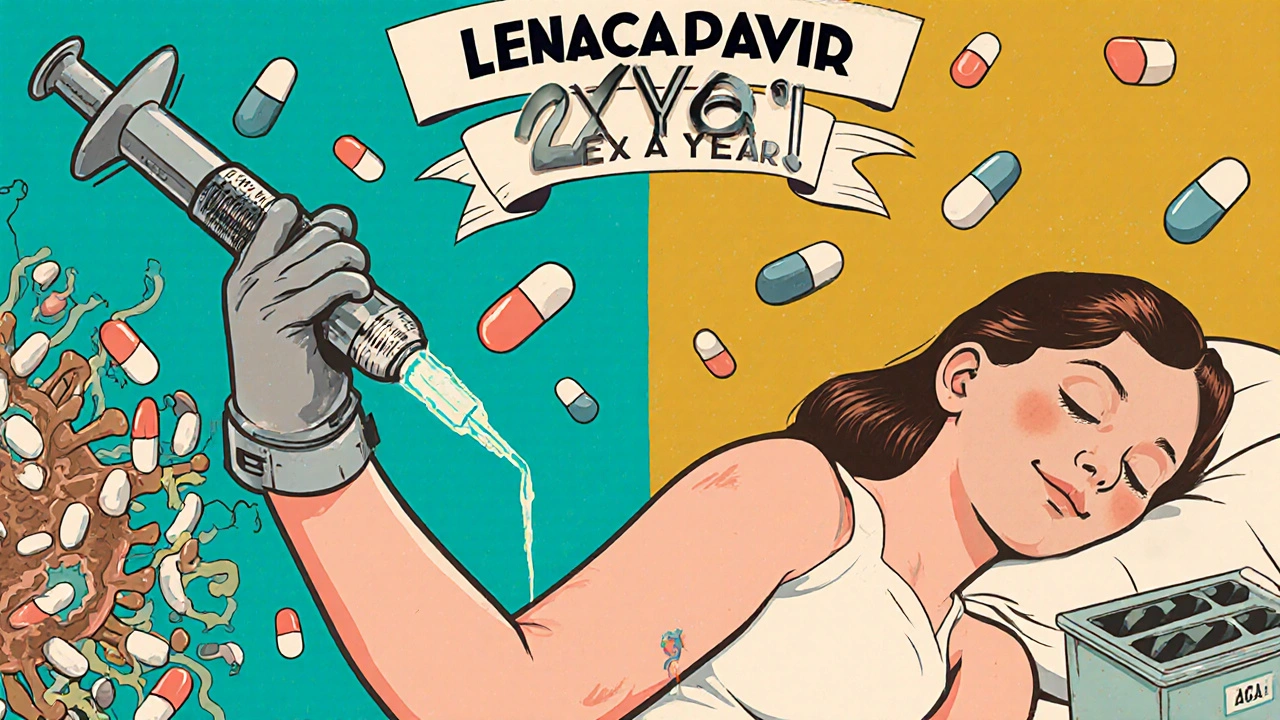
Compare that to modern HIV drugs like dolutegravir or lenacapavir. These have a high genetic barrier. The virus needs to change in three or four places at once to escape. That’s almost impossible without help-like missed doses or bad adherence. That’s why combination therapy is the gold standard now. One pill, multiple drugs, same goal: crush the virus before it can adapt.
Common Side Effects You Should Know
Not all side effects are scary. Some are just annoying. Others? They can make you quit.
For HIV patients on modern regimens, nausea and headaches are common in the first few weeks. Fatigue shows up in about 1 in 4 people. These usually fade. But for some, the long-term stuff matters more: weight gain, trouble sleeping, or mood changes. It’s not the drug itself-it’s how your body reacts to it over time.
Hepatitis C treatments with DAAs? Most people tolerate them well. But 23% report fatigue. 18% get headaches. That’s it. Compared to the old interferon days-where patients had flu-like symptoms for months-this is a win.
Herpes meds like valacyclovir? Usually gentle. But some people get dizziness or nausea. If you’re on foscarnet or cidofovir for resistant HSV? Those are tougher. Kidney stress, electrolyte imbalances, and IV infusions make them last resorts. You don’t take them unless you have to.
Bottom line: Side effects aren’t the same for everyone. But they’re predictable enough to plan for. Talk to your pharmacist. Ask: ‘What’s most likely to happen? What should I call my doctor about?’
Why Adherence Isn’t Just Important-It’s Life-or-Death
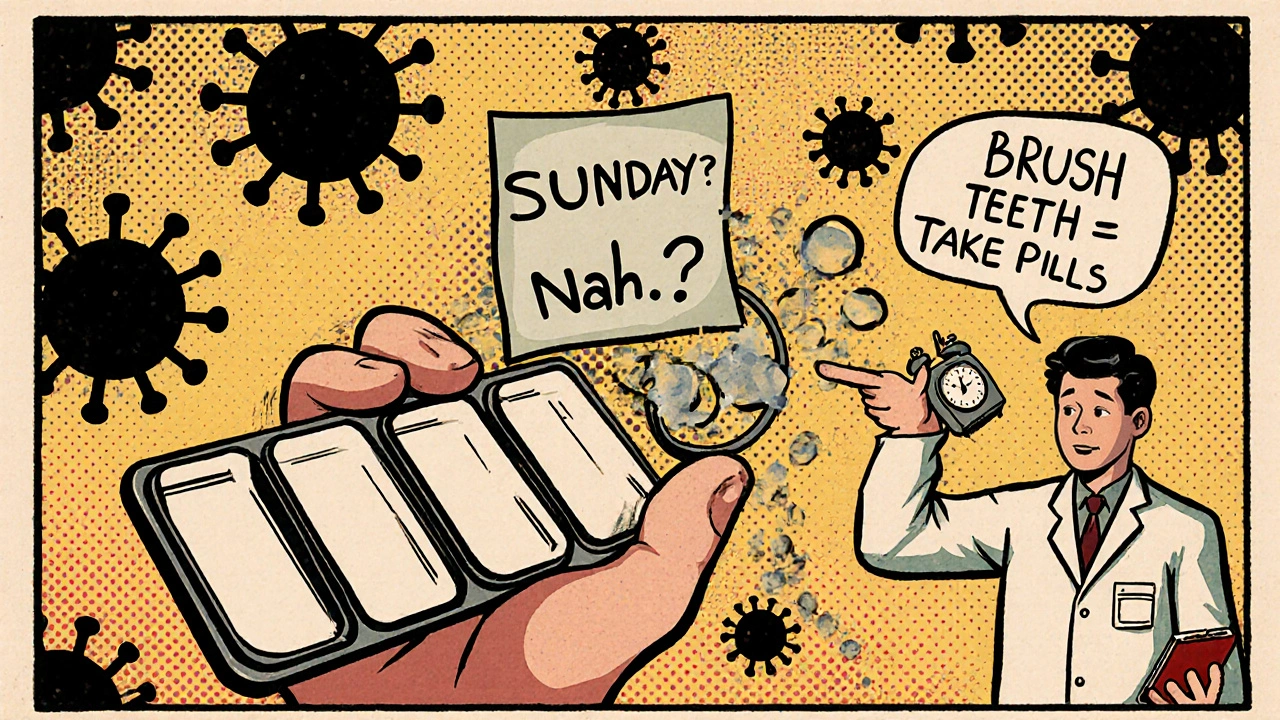
Let’s say you take your antiviral every day except Sunday. Sounds harmless, right? Wrong.
Viruses replicate fast. In one day, an HIV-infected person can produce billions of new virus particles. Miss a dose, and drug levels drop. The virus gets a breathing space. It mutates. That tiny gap? That’s where resistance starts.
Studies show that if you miss more than 5% of your doses over time, resistance risk jumps dramatically. For HIV, missing 10% of doses over a year can double your chance of treatment failure. For hepatitis B, skipping doses on lamivudine? You’re practically inviting resistance.
Why do people miss doses? Three big reasons:
- Complex schedules (three pills a day? Hard to remember)
- Side effects (feeling awful makes you want to stop)
- Travel or disruption (business trips, holidays, sleepovers)
The good news? Tools exist. Pill organizers? Used by 63% of people who stay on track. Phone alarms? Used by 57%. Apps that send reminders? They cut missed doses by nearly half. One study found patients who got weekly check-ins from a pharmacist had 28% fewer resistance cases.
Modern HIV pills? Single-tablet regimens. One pill, once a day. No more counting pills. No more timing meals. That’s why adherence jumped from 60% to over 90% in just five years.
What to Do If Resistance Shows Up
Resistance testing isn’t optional anymore. It’s standard.
If your viral load stops dropping-or starts rising-your doctor should order a resistance test. This isn’t a fancy lab trick. It’s a genetic scan of your virus. It tells you exactly which mutations are present. Then, your treatment plan changes.
For HIV, if you have the M184V mutation (common after missing doses on lamivudine or emtricitabine), you’ll likely switch to dolutegravir or bictegravir. These still work. For hepatitis B, if lamivudine failed, you move to tenofovir or entecavir. For herpes, if acyclovir doesn’t work, foscarnet or cidofovir step in-though those come with more risks.
The big shift? Resistance testing is now recommended before starting treatment for chronic infections like HIV and HBV. Why? Because some people already carry resistant strains. You don’t want to start with a drug that’s already broken.
How to Stay on Track-Real Strategies That Work
Here’s what actually helps people stick with their meds-not just theory, but real-world fixes:
- Use a pillbox with days of the week. Fill it every Sunday. See it. Know you’ve taken it.
- Set two alarms. One in the morning, one at night. Even if you’re not home, the phone buzzes. You remember.
- Link it to something you already do. Brush your teeth? Take your pill right after. Shower? Do it before. Habit stacking works.
- Ask for a 90-day supply. Fewer refills. Fewer chances to run out.
- Call your pharmacist. Not your doctor. Your pharmacist. They’re trained in adherence. They’ll help you sort out interactions, side effects, or confusing instructions.
- Don’t wait for a crisis. If you miss a dose, don’t panic. Just take it as soon as you remember. Then go back on schedule. Never double up unless your doctor says so.
For travelers: Pack extra. Keep meds in your carry-on. Know the time zone change. Set your phone to your home time until you’re settled.
What’s Changing Now-and What’s Coming
The game is shifting. In 2023, the FDA approved lenacapavir, a new HIV drug that blocks the virus’s shell. It’s given as a twice-yearly injection. No daily pills. No resistance seen in 96% of patients after two years.
CRISPR gene therapy? Still experimental. But early trials show it can cut HIV reservoirs by 60%-without triggering resistance. That’s huge.
For hepatitis C, cure rates are now over 95%. Most people are done in 8 to 12 weeks. No more interferon. No more 48-week treatments. That’s why adherence is no longer the biggest problem-it’s access. Only 12% of people with hepatitis B even get treated. Why? Cost. Fear of resistance. Lack of awareness.
Doctors now know: the best antiviral is the one you take. Not the fanciest. Not the newest. The one you can stick with.
Final Thought: You’re Not Just Taking a Pill
You’re part of a larger battle. Every time you take your antiviral, you’re not just protecting yourself. You’re helping stop the spread of resistant strains. That matters for your kids. Your partner. Your community.
Resistance isn’t inevitable. It’s preventable. And it starts with you-showing up, day after day, even when it’s hard.
Can antivirals stop working completely?
Yes, but only if the virus mutates and you keep exposing it to the same drug. This usually happens with missed doses or monotherapy. Modern combination treatments make complete failure rare. If resistance does develop, doctors switch to drugs that still work, based on lab testing.
Are side effects worse with older antivirals?
Absolutely. Older drugs like interferon for hepatitis C caused severe flu-like symptoms, depression, and fatigue for up to two years. Today’s antivirals are far gentler. Most side effects are mild and temporary-headache, nausea, or tiredness-that fade within weeks.
What happens if I miss one dose?
Don’t panic. Take the missed dose as soon as you remember, unless it’s almost time for the next one. Never double up. One missed dose rarely causes resistance-but repeated misses do. Keep your schedule tight. Use alarms or pill organizers to stay on track.
Is resistance permanent?
The mutation stays in your virus forever. But that doesn’t mean you’re stuck. Doctors can switch you to a different drug class that still works. Your body clears the old virus. The resistant strain may fade over time without drug pressure, but it can come back if you reuse the same medication.
Can I stop taking antivirals once I feel better?
No. For chronic infections like HIV or hepatitis B, stopping means the virus rebounds-and likely comes back stronger. Even if you feel fine, the virus is still there. Treatment isn’t about symptoms. It’s about suppression. Always follow your doctor’s plan.
Do antivirals cause long-term damage?
Some older drugs had risks like kidney or bone damage. Modern antivirals are much safer. Long-term studies show minimal impact on organs when taken as directed. Regular blood tests monitor for any changes. The bigger risk? Not taking them.
How do I know if my antiviral is still working?
Your doctor checks your viral load every 3 to 6 months. If it’s undetectable, the drug is working. If it rises, resistance may be developing. Don’t wait for symptoms. Lab tests are the only reliable way to know.
If you’re on antivirals, you’re doing something powerful. Stay consistent. Use the tools. Talk to your team. The virus is smart-but you’re smarter when you’re informed.







Man, this post hit different. Viruses don't care about your Monday blues or your alarm clock dying. They just replicate. And every missed pill? That's a tiny victory for evolution. I used to think resistance was some sci-fi villain thing-until my cousin's HIV regimen failed because he skipped doses during a road trip. Now I see it: we're not just patients. We're soldiers in a silent war against time and mutation. And yeah, the pills suck sometimes-but they're the only thing standing between us and chaos.
Stop treating adherence like a chore. Treat it like your life depends on it-because it does.
The scientific accuracy of this article is commendable. The distinction between low and high genetic barrier antivirals is particularly well-articulated. It is imperative that public health messaging reflects this nuance, as misconceptions regarding medication adherence remain pervasive even among educated populations. The data cited regarding resistance rates with lamivudine and the efficacy of combination therapy are consistent with current clinical guidelines. Further dissemination of such information could significantly reduce preventable treatment failures.
Bro... we're all just meat suits trying not to die. 🤷♂️
Viruses? They don't even know what a pill is. They just wanna live. And honestly? Maybe they're right. Why should we get to live forever while they get wiped out? I mean... who gave us the right?
But also... yeah, take your meds. I guess.
This is the kind of shallow, feel-good pamphlet journalism that gives medicine a bad name. You treat patients like children who need sticky notes and phone alarms. The real issue? Pharma pushed single-pill regimens because they're profitable-not because they're magically superior. And don't get me started on lenacapavir. A twice-yearly injection? That's not innovation-that's corporate control disguised as convenience. You think people are failing because they forget? No. They're failing because the system doesn't care about them.
Adherence isn't the problem. Capitalism is.
WHAT THE F*** ARE YOU TALKING ABOUT?!
Im not some lazy american who needs a phone alarm to take a pill! We used to fight wars with no meds and still won! Why do we need fancy drugs now?!
My uncle in Vietnam took penicillin from a jar and lived! Why cant people just be strong?!
Also i think this is all a globalist plot to make us dependent on big pharma! THEY CONTROL THE VIRUSES! I KNOW IT!
Also i misspelled some stuff cause im mad and im not a robot and i dont care what you think<3
ok but like… i took my HIV meds for 3 years straight and then missed a week during my mom’s funeral and now i’m terrified every time i sneeze. i know logically it’s not that big a deal but emotionally?? i feel like i betrayed everyone. the guilt is real. why do we make people feel like monsters for being human?
also i just took a pill and now i’m crying. thanks for that, post.
Excellent breakdown. I especially appreciate the emphasis on pharmacist involvement-so many people overlook that resource. I've seen patients who were overwhelmed by complex regimens turn their lives around with simple pill organizers and weekly check-ins. Also, the point about linking medication to daily habits? Genius. I started taking mine after brushing my teeth, and now I don't even think about it. Habit stacking is underrated.
One thing I'd add: if you're traveling, keep your meds in their original bottles with the prescription label. Customs can be a nightmare otherwise. Been there.
Thank you for writing this. I’ve been on antivirals for six years. Some days are harder than others. I don’t always talk about it. But reading this reminded me I’m not alone. I use the pillbox. I set two alarms. Sometimes I still forget. But now I don’t beat myself up. I just take it when I remember. And I keep going.
You don’t need to be perfect. You just need to show up.
Brothers and sisters this is not just about medicine this is about discipline this is about dignity
Every pill you take is a vote for your future
Viruses do not care about your schedule your pain your trauma
But you? You can choose to be stronger
Use the pillbox
Set the alarm
Call the pharmacist
This is not weakness this is wisdom
And if you do this every day for a year
You are not just surviving
You are winning
Respect the process
Respect yourself
This is one of the most clearly written public health pieces I’ve read in years. The distinction between monotherapy and combination regimens is critical for lay audiences to understand. The historical context of AZT resistance in the 80s provides necessary grounding. I especially appreciate the emphasis on accessibility as the new barrier-not adherence alone. In many low-resource settings, even the simplest regimen is out of reach. We must address cost and infrastructure before blaming patients for non-adherence.
Well done.
Oh please. You’re telling people to take their pills like they’re toddlers who need a sticker chart? What about the fact that these drugs are often toxic? What about the fact that we’re told to take them for life, even if we feel fine? Who even decided that suppression is the goal? What if the virus isn’t the enemy? What if our immune system is just… tired?
And why are we always the ones being told to change? Not the pharmaceutical companies. Not the doctors who push pills like candy. No. It’s always the patient. Always.
Wake up. This isn’t medicine. It’s control dressed in science.
Okay so imagine this: you’re a virus. You’ve been living in this human for years. They take a pill. You die. Again. And again. And again. But then… one day… they sleep in. They forget. They’re at a party. They’re grieving. They’re high. And suddenly-you’re free.
You multiply. You mutate. You laugh. You become a legend.
And now? You’re not just a virus.
You’re a rebel.
And the human? They’re just a footnote in your epic.
…
So yeah. Take your damn pills.
Or don’t.
But know this: when you do, you’re not just saving yourself.
You’re killing a god.
Look, I respect the science. But let’s be real. We’re being sold a fantasy. Resistance? It’s not your fault. It’s the system. You think people miss doses because they’re lazy? No. They’re working two jobs. They don’t have insurance. They’re scared of side effects because no one explained them properly. And now we’re blaming them for the failures of a broken healthcare system?
My cousin took her meds every day for five years. Then her Medicaid got cut. She stopped. Now she’s on a new regimen. Did she fail? Or did the system fail her?
We need to fix the system. Not the patients.
Wow. Just… wow. This post is so… so… *nice*. So soothing. So… comforting. Like a warm blanket made of corporate brochures. You know what’s really dangerous? Not taking your meds. But you know what’s even more dangerous? Believing that if you just take your pills, everything will be fine. That’s not medicine. That’s a cult. You’re being trained to obey. To trust the pill. To never question. To never feel. To never be human.
What if resistance isn’t the enemy? What if compliance is?