Medication Monitoring & Safety Tracker
Track Your Monitoring Schedule
Monitoring Schedule
Next Blood Test Due
Monitoring Risk Level
Time Since Start
Highest Risk Period
Compliance Status
Critical Symptoms to Watch For
If you experience ANY of these symptoms, seek emergency medical care immediately:
- Fever above 38.3°C (101°F)
- Sore throat that won't go away
- Mouth ulcers or sores
- Chills
- Unexplained fatigue
- General weakness
What to Do Next
If you have symptoms:
- Go to ER immediately
- Call your doctor (but don't wait for them to call you)
- Be specific: Say, "I'm on [your medication] and I'm worried about agranulocytosis. I have fever and sore throat."
- Never stop your medication without consulting your doctor first
When you take a medication for a chronic condition, you expect relief-not a life-threatening drop in your white blood cells. But for some people, common drugs can trigger agranulocytosis, a condition where the body stops producing enough neutrophils, the immune cells that fight off bacteria and fungi. Without them, even a minor sore throat can turn into sepsis within hours. This isn’t rare. Up to 70% of all agranulocytosis cases are caused by medications, and without quick action, death rates can hit 20%. The good news? With the right monitoring, that risk drops below 5%.
What Exactly Is Agranulocytosis?
Agranulocytosis isn’t just low white blood cells-it’s a crash. Normal neutrophil counts range from 1,500 to 7,000 per microliter of blood. Agranulocytosis kicks in when that number plunges below 100. At that level, your body can’t defend itself. You won’t get a big red bump or pus-filled wound. Instead, you might just feel tired, have a low-grade fever, or notice a sore throat that won’t go away. These aren’t signs you’d normally panic over. That’s why so many cases are missed.
The bone marrow, where blood cells are made, either stops producing neutrophils entirely or gets attacked by the immune system because of a drug. Some drugs trigger an allergic-like reaction where antibodies latch onto neutrophils and destroy them. Others poison the stem cells that turn into white blood cells. Either way, the result is the same: no shield against infection.
Which Medications Carry the Highest Risk?
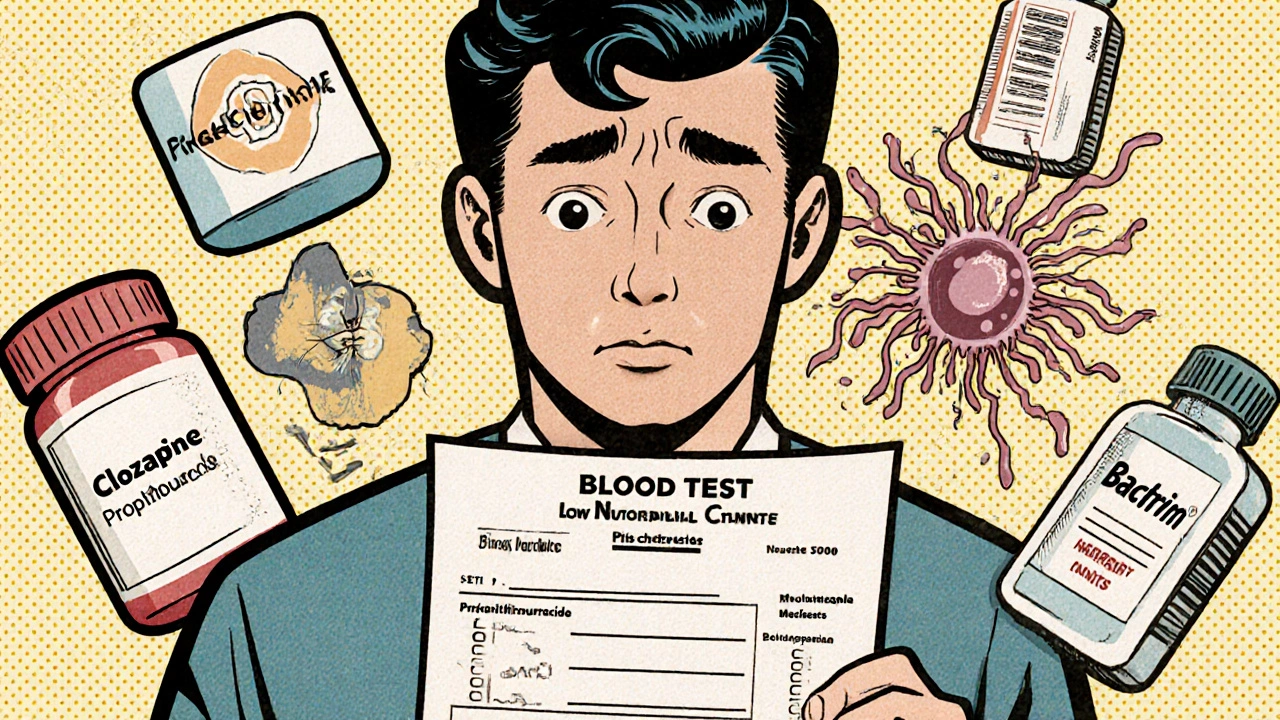
More than 200 drugs have been linked to agranulocytosis, but only a handful carry real, measurable danger. The biggest offender is clozapine, an antipsychotic used for treatment-resistant schizophrenia. About 0.8% of people taking it develop agranulocytosis-even with monitoring. That might sound small, but for someone with severe mental illness, the benefits often outweigh the risks. That’s why the FDA requires weekly blood tests for the first six months.
Antithyroid drugs like propylthiouracil and methimazole are next on the list. Propylthiouracil carries a risk of 0.36 cases per 1,000 patient-years. That means if 1,000 people take it for a year, about 4 will develop agranulocytosis. Methimazole is safer, but still risky enough that doctors check blood counts monthly during the first few months.
Antibiotics aren’t always innocent. Trimethoprim-sulfamethoxazole (Bactrim, Septra) raises your risk 16 times compared to other antibiotics. Even common painkillers like dipyrone (not sold in the U.S. but used in Europe and Latin America) have caused fatal cases. Ibuprofen and acetaminophen? Almost no link.
It’s not just the drug-it’s how long you’ve been on it. Most cases happen between 1 and 3 months after starting, but some appear after years. That’s why stopping a drug after a few weeks doesn’t mean you’re safe.
Why Infection Happens So Fast
Neutrophils are your first responders. They swarm into infected tissue within minutes. When they’re gone, bacteria multiply unchecked. A simple mouth ulcer can become a spreading infection. A cough might turn into pneumonia. A fever above 38.3°C (101°F) in someone with ANC under 500 is a medical emergency.
Unlike other infections, you won’t see swelling or pus. There’s no classic redness or warmth. That’s why patients often go to their doctor thinking they have a virus-and get sent home with advice to rest. By the time they return, they’re septic. A 2022 study in Clinical Infectious Diseases showed that giving broad-spectrum antibiotics like piperacillin-tazobactam within one hour of fever onset cuts death rates from 21% to under 6%.
The biggest danger? Delay. The Aplastic Anemia & MDS International Foundation found that 86% of patients waited more than 48 hours for a diagnosis. In rural areas, where labs take two days to return results, that delay can be fatal.

How Monitoring Saves Lives
The only way to catch agranulocytosis before it’s too late is through regular blood tests. For clozapine, the rules are strict: weekly CBCs for the first six months, then every two weeks for the next six, then monthly. If the ANC drops below 1,000, the drug is stopped immediately. That’s not just caution-it’s science. Studies show that acting at 1,000 instead of 500 catches 78% more cases before infection sets in.
But monitoring isn’t foolproof. A 2020 study found that over 30% of clozapine prescribers didn’t follow the weekly testing rule. Patients forget. Clinicians get busy. Labs get backed up. That’s why new tools are emerging. The Hemocue WBC DIFF device, approved by the FDA in 2022, gives a full neutrophil count in five minutes at the point of care. In one trial, using it improved patient adherence by over 30%.
For other high-risk drugs like propylthiouracil, monthly blood tests are standard. But in low-resource areas, even that’s a challenge. The WHO reports that only 32% of low- and middle-income countries have formal monitoring systems for these drugs.
What You Should Do If You’re on a High-Risk Drug
If you’re taking clozapine, propylthiouracil, or trimethoprim-sulfamethoxazole, here’s what you need to do:
- Know your drug’s risk level. Ask your doctor if it’s classified as Tier 1 (high risk) under European Medicines Agency guidelines.
- Get blood tests on schedule. Don’t skip them. Even if you feel fine.
- Watch for symptoms: fever, sore throat, mouth ulcers, chills, or unexplained fatigue.
- If you develop a fever above 38.3°C, go to the ER immediately. Say: “I’m on [drug name] and I’m worried about agranulocytosis.”
- Keep a list of all your medications and share it with every provider you see.
Don’t stop your medication on your own. Stopping suddenly can be dangerous-especially with antipsychotics or thyroid drugs. Talk to your doctor first.
New Tools and Future Changes
Science is catching up. In early 2023, the FDA approved the first genetic test for clozapine: the HLA-DQB1*05:02 assay. If you carry this gene variant, your risk of agranulocytosis is 14 times higher. Testing for it before starting clozapine could prevent cases entirely. Some clinics in the U.S. and Europe are already offering it.
Electronic health records are getting smarter too. A 2022 study showed AI systems that flag missed blood tests or rising infection risk reduced diagnostic delays by 47%. These systems are now being rolled out in major hospitals.
By 2028, experts predict that 40% of high-risk medications will require genetic screening before use. That’s a huge shift-from reactive monitoring to proactive prevention.
What Happens After Diagnosis?
If agranulocytosis is caught early, recovery is usually quick. Once the drug is stopped, neutrophils typically bounce back in 1 to 3 weeks. But if infection sets in, treatment becomes complex. You’ll need hospitalization, IV antibiotics, and sometimes granulocyte colony-stimulating factors (G-CSF) to speed up white blood cell production.
Long-term, most people can go back on the same drug-but only if they’re rechallenged under strict supervision. Only a few do, because the risk is too high. For others, switching to a safer alternative is the only option.
Why This Matters Beyond the Individual
Agranulocytosis isn’t just a patient problem. It’s a system failure. In the U.S., pharmaceutical companies have paid out over $187 million in lawsuits related to drug-induced cases. The FDA has issued 27 safety alerts in the last 12 years. Yet, rural and underserved communities still face 2.3 times higher death rates because they can’t get timely blood tests.
Monitoring isn’t optional. It’s the difference between life and death. For every person who dies from a preventable infection, there’s a missed blood test, a delayed call, a lack of education. Better systems, better tools, and better awareness can change that.
Can agranulocytosis be reversed?
Yes, if caught early. Stopping the medication that caused it usually allows the bone marrow to recover within 1 to 3 weeks. Neutrophil counts typically return to normal without lasting damage. However, if a severe infection develops before treatment, recovery can take longer and may require hospitalization, IV antibiotics, or growth factor injections.
How often should I get blood tests if I’m on clozapine?
Under FDA guidelines, you need weekly blood tests for the first 6 months, then every 2 weeks for the next 6 months, and then monthly after that. If your absolute neutrophil count (ANC) drops below 1,000/μL, your doctor must stop the drug immediately. Missing a test puts you at serious risk.
What symptoms should I watch for?
Fever above 38.3°C (101°F), sore throat, mouth ulcers, chills, fatigue, or unexplained weakness. These are often mistaken for the flu or a cold. If you’re on a high-risk medication and have any of these, seek medical help immediately-don’t wait.
Is agranulocytosis the same as neutropenia?
No. Neutropenia means a low neutrophil count (below 1,500/μL). Agranulocytosis is a severe form-below 100/μL. It’s rare but life-threatening. While neutropenia can be managed with observation, agranulocytosis requires immediate action to prevent fatal infection.
Can I take over-the-counter painkillers if I’m at risk?
Ibuprofen and acetaminophen are generally safe and not linked to agranulocytosis. Avoid dipyrone (available outside the U.S.) and other NSAIDs unless approved by your doctor. Always check with your prescriber before starting any new medication, even if it’s sold without a prescription.
Are there alternatives to clozapine if I’m worried about agranulocytosis?
Yes, but clozapine is often the only effective treatment for severe, treatment-resistant schizophrenia. Alternatives like olanzapine, risperidone, or quetiapine may be tried first. If those fail, clozapine remains the gold standard. Genetic testing for HLA-DQB1*05:02 can help determine if you’re at higher risk before starting.








Look, I get it-meds can mess you up. But let’s be real: if you’re on clozapine and you’re not getting weekly blood tests, you’re basically playing Russian roulette with your bone marrow. My cousin did it for two years without a single check. Said he ‘felt fine.’ Ended up in ICU with sepsis from a damn gum abscess. Now he’s on disability and can’t even hold a job. Stop being lazy. Get tested. It’s not hard.
While the clinical data presented here is both comprehensive and well-sourced, I would respectfully suggest that greater emphasis be placed on the socioeconomic disparities in access to monitoring. The fact that only 32% of low- and middle-income countries maintain formal surveillance systems for high-risk medications underscores a global health inequity that extends beyond individual patient responsibility. Pharmacovigilance must be institutionalized, not optional.
I’ve been on propylthiouracil for six years. I’ve had my blood drawn every month like clockwork. I’ve cried in the lab parking lot because I was scared to see the results. But I’m still here. And I’m not just surviving-I’m teaching yoga, hiking with my dog, laughing with my kids. This isn’t just about numbers on a chart. It’s about showing up for your own life-even when it’s terrifying. You’re not weak for needing help. You’re brave for asking for it.
Man, this whole thread is a masterclass in how medicine should work-but doesn’t. I work in a clinic in rural Ohio, and half the folks on clozapine don’t even have a car to get to the lab. We’ve started using the Hemocue device on Tuesdays and Thursdays-five-minute finger prick, instant result. One lady came in crying because she hadn’t been tested in four months. She said, ‘I thought I was fine.’ I said, ‘You’re fine now. But you weren’t yesterday.’ We caught her ANC at 890. She’s alive because we moved the lab to her neighborhood. Stop waiting for perfection. Just start somewhere.
Okay, real talk: if you’re on a high-risk med and you skip a blood test, you’re not just risking your life-you’re risking everyone around you. Sepsis doesn’t care if you’re ‘too busy.’ It doesn’t care if you ‘don’t feel sick.’ It just spreads. And if you end up in the ER, you’re tying up beds, ventilators, nurses who are already burnt out. Be responsible. Not for the system-for yourself. Your life matters. Get. The. Test.
So the FDA says clozapine causes agranulocytosis but they also say its the only thing that works for schizophrenia... so why dont they just ban it? And why arent they testing ALL meds for this? And why do we even have this system? I think the pharmas are hiding something. They make billions off the tests and the hospital stays. And they dont want you to know that a simple vitamin could prevent this. They just want you dependent. The government is in on it too. They dont want you healthy. They want you paying. You think this is medicine? Its a money machine.
Wow. Such a moving, deeply researched piece. Truly. I’m sure the 70% of people who didn’t die from drug-induced agranulocytosis are just thrilled you took the time to write this. I mean, really-who else is going to remind people to get blood tests? The pharmaceutical reps? The insurance companies? The doctors who’ve never heard of HLA-DQB1*05:02? You’re a hero. Truly. I’ll be sure to print this out and tape it to my fridge next to my coupon for 20% off antacids.
Thank you for writing this. I know how scary it is to be told you need to get blood drawn every week. I’ve been there. I’ve sat in that waiting room wondering if today’s the day my numbers crash. But you’re not alone. If you’re reading this and you’re scared-take a breath. You’re doing the right thing. Even if you’re tired. Even if it’s inconvenient. You’re protecting your future self. And that’s worth it.
This is the kind of post that makes me believe in humanity again. You didn’t just list facts-you gave people a lifeline. I’ve got a friend on clozapine who skipped tests for six months. After reading this, he went in. His ANC was at 980. They stopped the drug, gave him G-CSF, and now he’s back to coaching his kid’s soccer team. That’s the power of knowledge. Don’t let fear silence you. Speak up. Get tested. Live.
I’ve been a nurse in the UK for 27 years. I’ve seen this happen-over and over. A young man, 22, on methimazole, ignored the fatigue, the sore throat. Thought it was just stress. Came in with a temp of 40.1°C, septic, no neutrophils. We gave him everything. He didn’t make it. His mum still comes in every year on the anniversary. We keep his file. We don’t forget. This isn’t theoretical. It’s real. And it’s preventable. If you’re on one of these drugs, don’t wait for the fever. Don’t wait for the pain. Get tested. Even if you think you’re fine. You’re not. Not until the blood says so.
One must consider the ontological implications of medicalized survival. The very act of monitoring one's hematopoietic function in response to pharmacological intrusion constitutes a form of biopolitical subjugation. One is not merely managing a disease; one is being disciplined by the pharmaceutical-industrial complex. The HLA-DQB1*05:02 assay does not liberate-it quantifies compliance. The Hemocue device is not innovation; it is the extension of the panopticon into the venous system. To seek safety through testing is to surrender autonomy to an algorithm. Are we patients-or data points?
Wow. So much effort. So many words. And yet... you still didn’t mention that dipyrone is banned in the US because people kept dying from it. Thanks for the recap, I guess.