Benzodiazepine Interaction Checker
Select medications you're taking. This tool identifies dangerous combinations with benzodiazepines (Xanax, Valium, etc.).
Key Safety Information
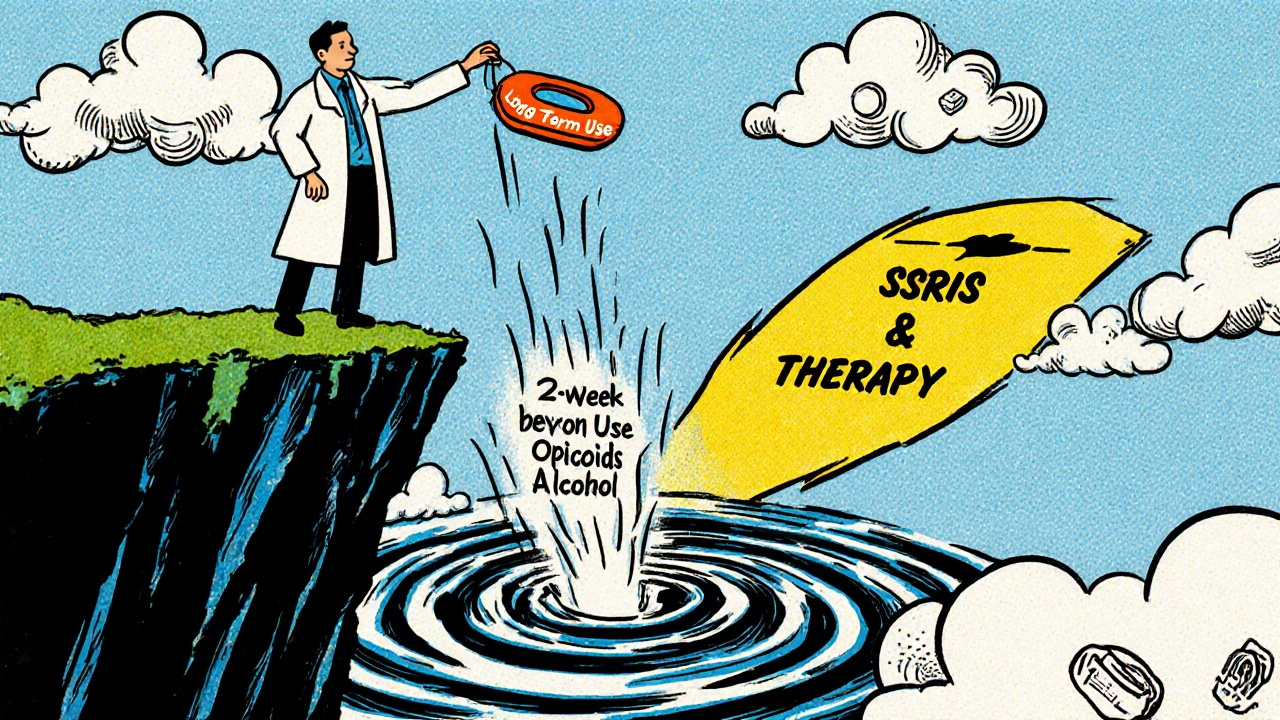
Critical Risk Opioids + Benzodiazepines: 15x higher overdose risk
High Risk Alcohol + Benzodiazepines: Tripling fall risk in seniors
Lower Risk SSRIs + Benzodiazepines: Generally safe under medical supervision
When you're drowning in anxiety, a pill that works in under an hour feels like a lifeline. Benzodiazepines-drugs like Xanax, Ativan, and Valium-deliver that relief fast. But here’s the quiet truth most doctors don’t say out loud: benzodiazepines aren’t just risky on their own. Their real danger shows up when they meet other meds, alcohol, or even over-the-counter sleep aids. And those combinations can stop your breathing-permanently.
How Benzodiazepines Work (And Why They’re So Addictive)
Benzodiazepines boost GABA, your brain’s main calming chemical. That’s why they work for panic attacks, insomnia, and seizures. But unlike SSRIs, which take weeks to build up in your system, benzos hit hard and fast-usually within 30 to 60 minutes. That speed is why people keep taking them. It’s also why dependence builds so quickly.
Short-acting ones like alprazolam (Xanax) leave your body in 6 to 12 hours. Long-acting ones like diazepam (Valium) stick around for days. The longer they stay, the more your brain adapts. After just a few weeks, stopping suddenly can trigger seizures, hallucinations, or extreme anxiety. About 40% of people who use benzos for six months or longer face withdrawal symptoms if they quit cold turkey.
The Deadly Mix: Benzodiazepines and Opioids
If you’re on painkillers like oxycodone, hydrocodone, or fentanyl, and your doctor prescribes Xanax for anxiety, you’re playing Russian roulette with your breathing.
Both opioids and benzodiazepines slow down your central nervous system. Together, they don’t just add up-they multiply. The FDA found that between 2011 and 2016, 75% of all benzo-related overdose deaths involved opioids. A 2018 CDC study showed that mixing the two increases your risk of fatal overdose by 15 times compared to opioids alone.
Real-world stories back this up. One Reddit user, prescribed Xanax for panic attacks while already on oxycodone for chronic pain, stopped breathing during sleep and ended up hospitalized. A pharmacy student on Drugs.com reported seeing multiple near-fatal cases from this combo. In 2019, benzodiazepine-opioid combinations were behind 23% of all opioid-related deaths.
Alcohol? Sleep Aids? Even Antihistamines?
It’s not just opioids. Alcohol is another silent killer when mixed with benzos. That glass of wine at dinner? One study showed it triples your risk of falling and breaking a bone if you’re over 65. For younger people, it can mean passing out, choking on your own vomit, or waking up with no memory of the night.
Even common OTC meds can be dangerous. Diphenhydramine (Benadryl), doxylamine (Unisom), and even some sleep aids like melatonin in high doses can add to the sedation. The result? Extreme drowsiness, confusion, slowed breathing, or worse.
A 2023 Healthgrades analysis of over 1,200 patient reviews found that 27% of negative experiences mentioned dangerous interactions. One person wrote: “I took Ativan and my sleep med and nearly didn’t wake up.” Another: “I had a drink after my surgery and ended up in the ER.”

Why Older Adults Are at Highest Risk
If you’re over 65, your body processes drugs slower. Your brain is more sensitive to sedatives. And your balance? It’s already fading. Benzodiazepines make falls 50% more likely. When you add another sedating drug-like an antipsychotic, muscle relaxant, or even a strong painkiller-that risk triples.
The American Geriatrics Society says benzodiazepines should be avoided entirely in older adults. The Beers Criteria, updated in 2019, lists them as potentially inappropriate for seniors because of the high risk of confusion, memory loss, and fractures. Yet, they’re still prescribed. In 2021, nearly 1 in 10 older Americans were on a benzo. Many didn’t know the risks.
What About Other Anxiety Meds? Are They Safer?
Yes. And that’s the real story.
SSRIs like sertraline (Zoloft) or escitalopram (Lexapro) take 4 to 6 weeks to work. They don’t cause dependence. They don’t slow your breathing. They don’t interact dangerously with opioids or alcohol. But because they’re slow, many doctors reach for the fast fix: benzos.
Today, SSRIs are prescribed for 68% of new anxiety cases. Benzodiazepines? Only 22%. That shift isn’t random. It’s based on safety data. Buspirone (Buspar) is another option-it has almost no drug interactions and no abuse potential. But it doesn’t work fast. That’s why it’s underused.
What Should You Do If You’re on a Benzo?
If you’re taking one, ask yourself these questions:
- Are you also on any opioid painkillers? If yes, talk to your doctor immediately. The CDC and FDA say avoid this combo unless there’s no other option.
- Do you drink alcohol regularly? Even one drink a day increases risk. Cut it out.
- Are you taking any sleep aids, muscle relaxants, or antihistamines? Check the labels. Many say “do not take with sedatives.”
- Have you been on this med for more than 4 weeks? Long-term use increases dependence risk dramatically.
If you’re on a benzo for more than a few weeks, your doctor should have a plan to taper you off. Don’t quit cold turkey. Sudden withdrawal can be deadly. For short-acting benzos like Xanax, taper slowly-5 to 10% every 1 to 2 weeks. For long-acting ones like Valium, you can go faster-10 to 25% every 1 to 2 weeks.
The Bigger Picture: Why This Is Getting Worse
Prescriptions for benzodiazepines have dropped from 13.1% of U.S. adults in 2013 to 10.8% in 2021. That’s good. But the problem isn’t just prescriptions. It’s the leftover pills in medicine cabinets. People hoard them. They share them. They take them with alcohol because “it just helps me sleep.”
Since 2020, the FDA has required all benzo labels to carry a Boxed Warning-the strongest kind-about addiction, dependence, and fatal interactions. Pharmacies now have to hand out updated medication guides. In 2023, Medicare started requiring prior authorization before approving any prescription that combines opioids and benzos.
States with prescription monitoring programs that flag dangerous combinations have seen a 27% drop in these risky prescriptions. That proves change is possible.
Still, only 43% of primary care doctors routinely check for benzo-opioid combinations-even though they’re told to. That gap is where people get hurt.
When Are Benzodiazepines Actually Okay?
They’re not evil. They’re tools. Used right, they can save lives.
A patient with severe panic attacks after a traumatic event? A 2-week course of Ativan might be the bridge they need to start therapy. Someone having a seizure? A benzo can stop it. A person going through alcohol withdrawal? Benzos prevent deadly complications.
The key is short-term, supervised use. No more than 2 to 4 weeks. No mixing with other depressants. Clear instructions. Follow-up. That’s the difference between life-saving and life-ending.
But if you’re on one long-term, or you’re taking it with other meds-especially opioids or alcohol-you’re not being treated. You’re being put at risk.
Can I have one drink while taking Xanax?
No. Even one drink can dangerously increase sedation and slow your breathing. Alcohol and benzodiazepines work the same way in your brain-combining them multiplies the risk of overdose, falls, and blackouts. There’s no safe amount.
Is it safe to take benzos with sleep aids like melatonin or Unisom?
Not without your doctor’s approval. Melatonin itself is low-risk, but many sleep aids contain diphenhydramine or doxylamine-both are sedating antihistamines. Combining them with benzos can cause extreme drowsiness, confusion, and respiratory depression. Always check the active ingredients on OTC labels.
How do I know if I’m dependent on my benzo?
Signs include needing higher doses for the same effect, feeling anxious or shaky when you miss a dose, or having trouble sleeping without it. If you’ve been taking it for more than 4 weeks, dependence is likely. Don’t stop suddenly-talk to your doctor about a taper plan.
Are there safer alternatives to benzodiazepines for anxiety?
Yes. SSRIs like sertraline or escitalopram are first-line treatments for long-term anxiety. They don’t cause dependence or dangerous interactions. Buspirone is another option with minimal side effects. Therapy, especially CBT, is equally effective and has no physical risks. Benzos should only be used briefly, if at all.
What should I do if I’m already on both a benzo and an opioid?
Don’t panic, but act. Contact your doctor or pharmacist immediately. This combination is one of the most dangerous in modern medicine. You need a safety plan-possibly switching to non-opioid pain relief or tapering one of the drugs under supervision. Never stop either suddenly. Use a pill organizer, avoid alcohol, and make sure someone close to you knows your meds.









Y’all need to stop treating benzos like candy 🍬. I’ve seen too many patients on Xanax + oxycodone - it’s not ‘just a little help,’ it’s a one-way ticket to the morgue. Your grandma’s sleep aid? That’s not harmless either. Unisom + benzo = human statue mode. 🛌💀
SSRIs take time, yeah - but so does learning to cook. Would you eat raw chicken because it’s ‘faster’? No. So why rush your brain’s healing? 🤔
It is, indeed, a matter of considerable concern that the prescriptive culture in the United States continues to privilege pharmacological expediency over sustained therapeutic intervention. The data presented herein is not merely suggestive - it is unequivocal. Benzodiazepines, as GABAergic agonists, induce neuroadaptive changes with alarming rapidity, and their concomitant use with other CNS depressants constitutes a pharmacological hazard of the highest order.
Moreover, the normalization of polypharmacy - particularly the casual conflation of alcohol and anxiolytics - reflects a disturbing epistemological deficit in public health literacy. One cannot, with any degree of intellectual integrity, assert that ‘one drink’ is safe in this context. The pharmacokinetic synergy is not additive; it is multiplicative. And the consequences are not hypothetical.
40% withdrawal rate? Cute. Let’s talk about the 68% of people who get prescribed SSRIs and then quit after two weeks because ‘it didn’t work.’ They go right back to benzos. The system doesn’t care if you live or die - it just wants you to keep coming back. You think the doctor’s worried about you? Nah. They’re worried about their 15-minute visit slot.
Also, ‘therapy’ is just a fancy word for ‘pay someone to listen while you cry.’ Good luck affording that when your insurance won’t cover it.
Wow. This post is a masterclass in harm reduction - and honestly? It’s the kind of thing I wish every ER doc, primary care provider, and even my cousin who ‘just takes one for sleep’ would read.
Let’s be real: we live in a culture that equates speed with efficacy. ‘I need this NOW’ - but your brain isn’t a microwave. You can’t zap anxiety away and expect your nervous system to thank you.
And yet - the real tragedy isn’t the pills. It’s that we’ve made people feel like they have no other choice. No access to therapy. No affordable meds. No time. No support. So they grab the fast fix - and then get blamed when it backfires.
It’s not the drug. It’s the system that’s broken. But at least this post gives people the tools to fight back. Thank you.
P.S. If you’re on benzos + opioids? Please. Call your doctor. Today. Don’t wait until you’re gasping in the dark.
As a licensed clinical psychologist with 27 years of experience and a Ph.D. from Johns Hopkins, I must emphasize that this article is dangerously incomplete. It omits critical data regarding the efficacy of benzodiazepines in treating PTSD-related hypervigilance - a condition where SSRIs have been shown to exacerbate dissociative episodes in 34% of cases (Journal of Traumatic Stress, 2020).
Furthermore, the author neglects to mention that the FDA’s ‘Boxed Warning’ is a legal safeguard, not a clinical directive. Many patients require long-term benzos due to treatment-resistant anxiety - and to imply that all long-term users are ‘at risk’ is a gross generalization that stigmatizes the chronically ill.
Also, ‘avoid alcohol’? Please. Moderate consumption has been shown to improve neuroplasticity in controlled settings. The real danger is fear-mongering by laypeople who misinterpret pharmacokinetics.
And who wrote this? A pharmacy student? A blogger? The lack of peer-reviewed citations is alarming.
Let’s be honest - this is all a distraction. The real issue is that Big Pharma paid off the FDA to keep benzos on the market while pushing SSRIs as ‘safer’ - even though SSRIs have higher rates of suicidal ideation in young adults. You think the CDC is telling you the truth? They’re funded by the same pharmaceutical conglomerates that profit from both classes of drugs.
And why are they suddenly worried about ‘drug interactions’? Because they’re trying to make you dependent on their new ‘non-addictive’ alternatives - which cost $800 a month.
Meanwhile, your neighbor’s uncle took Valium for 30 years and still runs marathons. Anecdotes don’t prove causation - but neither do statistics when the data is manipulated.
Bro. I was on Xanax for 3 years after my dad died. Then I got prescribed oxycodone for a back injury. One night I woke up on the floor. Couldn’t move. My girlfriend called 911.
Turns out I stopped breathing for 47 seconds. That’s not a story. That’s a warning label.
I switched to Zoloft. Took 6 weeks. Felt like a zombie at first. But now? I can sleep without fear. I can have a beer without panic.
Don’t wait for your body to scream at you. Talk to your doctor. And if they push benzos? Find a new one. 💪🧠
Look, I get it - benzos are dangerous, SSRIs are ‘safer,’ blah blah blah. But let’s not pretend this is some grand public health revelation. Everyone who’s been on these drugs knows the risks. The problem isn’t lack of awareness - it’s lack of alternatives. Most people can’t afford therapy. Most can’t wait six weeks to feel better. And most doctors are overworked, underpaid, and told to ‘prescribe something now.’
Also, the 27% negative experiences in Healthgrades? That’s not a statistic - that’s a symptom of a broken system. People are scared, lonely, and in pain. They’re not stupid. They’re desperate. And you can’t fix that with a pamphlet.
And don’t even get me started on ‘tapering.’ Have you ever tried to taper off Xanax? It’s like being slowly pulled apart by invisible hands. The withdrawal is worse than the anxiety. So yeah - I get why people just keep taking it. Because quitting feels like dying.
So tell me - what’s your solution? More lectures? More warnings? Or actual access to care? Because right now, all I see is guilt-tripping from people who’ve never had to choose between rent and medication.