Black Cohosh Medication Interaction Checker
Check Your Medication Interactions
Black cohosh may interact with common medications and increase risk of liver damage. Select any medications you take to see potential interactions.
Results
Select medications to see potential interactions with black cohosh.
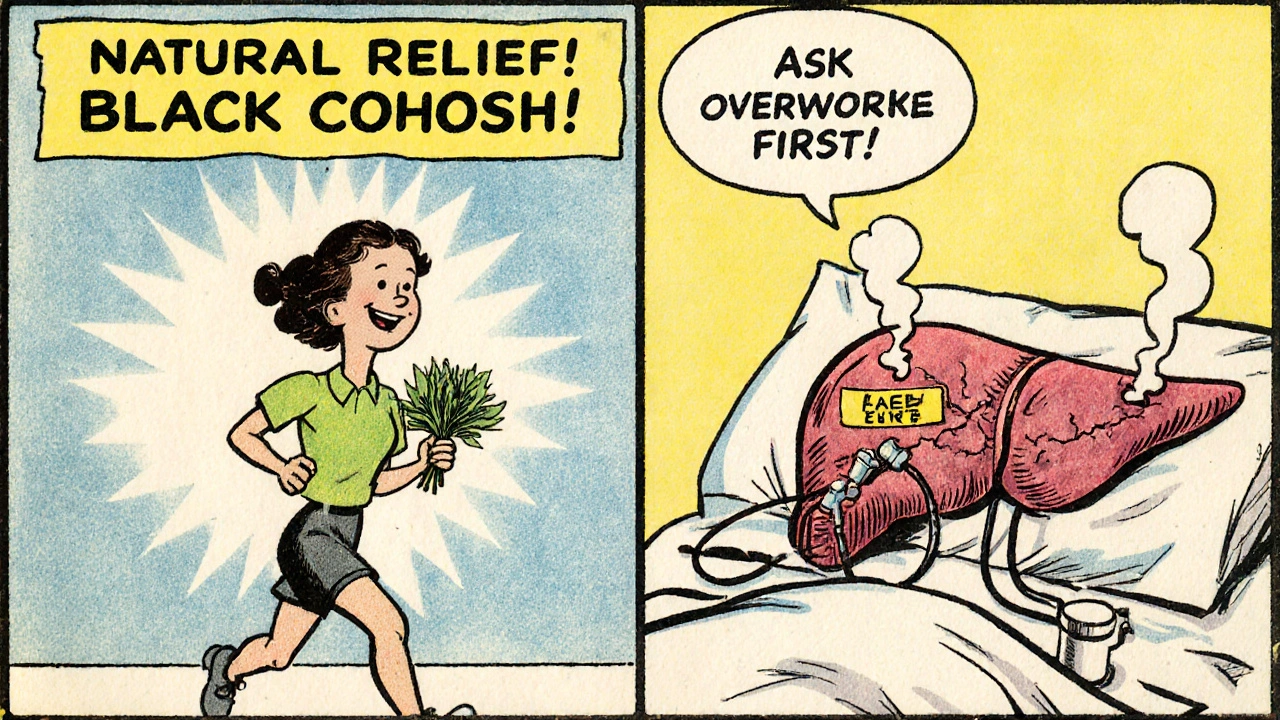
Black cohosh has been a go-to herbal remedy for women managing menopause symptoms for decades. It’s marketed as a natural alternative to hormone therapy, promising relief from hot flashes, night sweats, and mood swings without the risks of estrogen. But behind the glowing Amazon reviews and quiet endorsements from wellness influencers lies a quiet but serious risk: liver damage. And it doesn’t just happen out of nowhere-it often shows up when black cohosh is mixed with common medications you might not even think twice about.
What Black Cohosh Actually Does (and Doesn’t Do)
Black cohosh comes from the roots and rhizomes of a North American plant, Cimicifuga racemosa. It’s been used since the 1800s, and by the 1990s, it became a household name in the U.S. as women looked for ways to avoid traditional hormone replacement therapy. Products like Remifemin are among the most studied, with typical doses ranging from 20 to 40 mg twice daily. The active compounds-triterpene glycosides like actein and cimicifugoside-are thought to influence serotonin and opioid pathways in the brain, not estrogen receptors. That’s why many women with a history of breast cancer were told it was safe.
But here’s the catch: clinical trials on its effectiveness are mixed. Some show modest improvement in hot flashes; others show no difference from placebo. The benefit isn’t strong, and the risks? They’re real.
Liver Damage Isn’t Rare-It’s Documented
Since 2003, more than 50 cases of liver injury linked to black cohosh have been reported to the U.S. LiverTox database. These aren’t minor spikes in liver enzymes. These are cases of acute hepatitis, cholestasis, autoimmune-like liver injury, and even liver failure requiring transplants.
In one documented case, a 51-year-old woman developed ALT levels of 722 U/L (normal is under 56) and bilirubin of 15.8 mg/dL after three months of black cohosh use. She needed hospitalization. Another woman, 54, developed acute liver failure after combining black cohosh with acetaminophen-both within recommended doses-and required a transplant.
The pattern? Most injuries show up after 2 to 6 months of use. Symptoms include yellowing skin or eyes (jaundice), dark urine, extreme fatigue, nausea, and pain under the right ribs. Many people ignore these signs, thinking it’s just the flu or stress. By the time they get tested, the damage is advanced.
Why It Harms the Liver (And Why It’s Hard to Predict)
No one knows exactly how black cohosh causes liver injury. It’s not a simple poison. It doesn’t affect everyone. That’s what makes it so dangerous.
Researchers believe it’s either:
- A direct toxic effect from certain compounds in the extract
- An idiosyncratic reaction-your body’s unique immune or metabolic response
- An interaction with other drugs that overwhelms your liver’s ability to process them
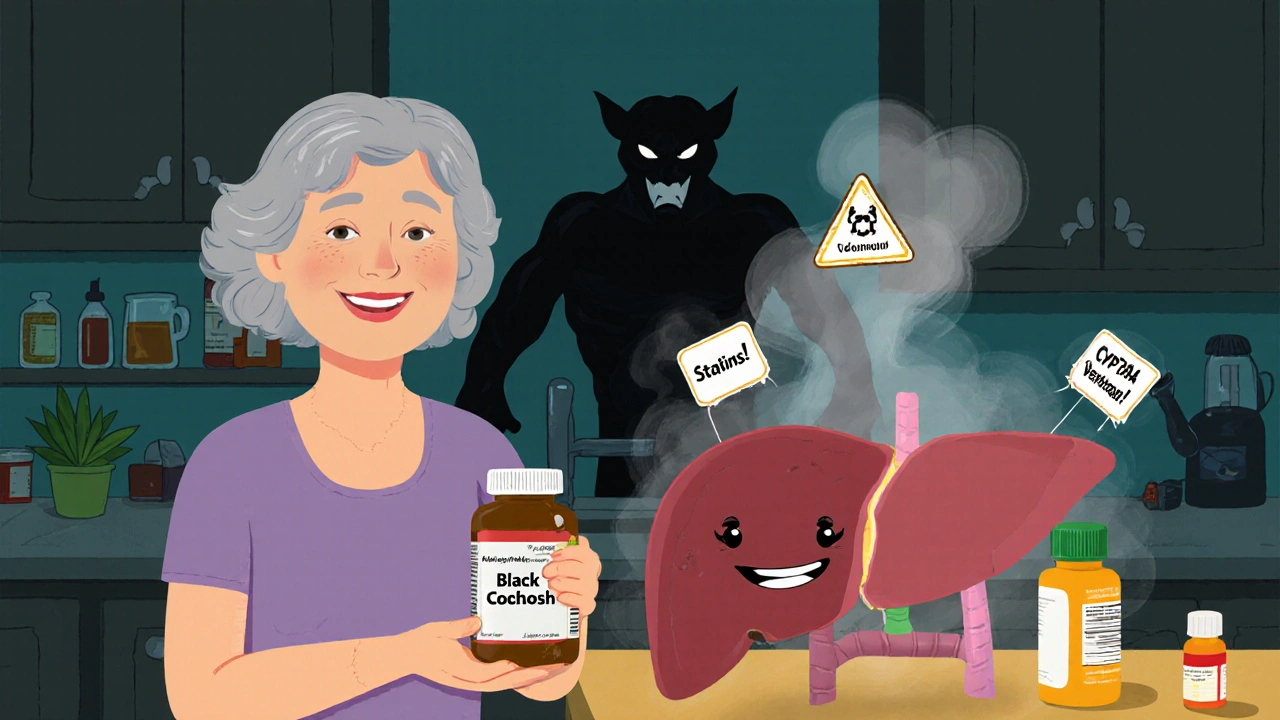
Black cohosh is broken down by liver enzymes called CYP3A4 and CYP2D6. That’s the same system that handles dozens of common medications. When you take black cohosh with something else that uses these enzymes, your liver gets overloaded. The result? Toxic buildup. Liver cells die. Inflammation follows.
Medications That Turn Black Cohosh Into a Risk
This is where most people get caught off guard. You’re not taking black cohosh alone. You’re taking it with other things-and those combinations can be deadly.
Acetaminophen (Tylenol): This is the most dangerous combo. Even at normal doses, combining acetaminophen with black cohosh has led to liver failure. Both are processed by the same liver pathways. Together, they create a perfect storm.
Statins (like atorvastatin, simvastatin): Used to lower cholesterol, statins already carry a small risk of liver enzyme elevation. Add black cohosh, and that risk jumps. A 2023 study showed a 3.2-fold increase in liver injury when both were taken together.
Methotrexate: Used for autoimmune diseases and some cancers, methotrexate is hard on the liver. Black cohosh doesn’t make it safer-it makes it worse.
Antibiotics like clarithromycin: These are strong CYP3A4 inhibitors. They slow down how fast your liver breaks down black cohosh, causing it to build up to toxic levels.
Birth control pills and hormone therapies: Even though black cohosh isn’t estrogenic, mixing it with hormonal meds adds metabolic stress to the liver. No one’s studied this well, but the risk is high enough that experts recommend avoiding it.
Who Should Never Take It
If you have any of these conditions, don’t take black cohosh-not even once.
- Pre-existing liver disease (fatty liver, hepatitis, cirrhosis)
- History of liver injury from any supplement or medication
- Taking any of the medications listed above
- Alcohol use disorder or regular heavy drinking
- Autoimmune conditions like lupus or rheumatoid arthritis
The American College of Obstetricians and Gynecologists updated its guidelines in January 2024 to explicitly warn against black cohosh use in patients with liver conditions or those on hepatotoxic drugs. That covers about 38% of the menopausal population.
What About ‘Liver-Safe’ Formulas?
Some brands-Gaia Herbs, Nature’s Way-now market "liver-safe" black cohosh extracts. They claim to remove the toxic compounds using special processing. Sounds promising, right?
Here’s the truth: there’s zero clinical evidence to back it up. In June 2023, the American Gastroenterological Association issued a clear statement: "No clinical data supports improved safety for these modified formulations."
Just because a label says "liver-safe" doesn’t mean it is. The FDA doesn’t regulate supplements for safety before they hit the shelf. These claims are marketing, not medicine.
What to Do If You’re Already Taking It
If you’ve been taking black cohosh for months and feel fine, don’t panic-but don’t ignore the risk either.
Here’s what to do:
- Stop taking it immediately if you notice yellowing skin, dark urine, unexplained fatigue, or abdominal pain.
- Get a liver function test (LFT). ALT, AST, bilirubin, and alkaline phosphatase levels will tell you if your liver is stressed.
- Don’t restart it-even if you felt better. The damage can be silent until it’s too late.
- Talk to your doctor about alternatives. SSRIs like paroxetine or escitalopram have been shown to reduce hot flashes as effectively as black cohosh-with far less risk.
Most primary care doctors don’t routinely check liver enzymes for supplement users. A 2022 study found only 22% of doctors monitored LFTs for patients on herbal products. Don’t wait for them to ask. Take charge.
Real People, Real Consequences
On Reddit’s r/Supplements, a user wrote: "Took black cohosh for 3 months. Normal liver tests at first. Then ALT jumped to 485. No symptoms until I was hospitalized. They said it was likely the supplement. I’m done with herbs."
On Drugs.com, 32% of 138 reviews mention liver-related symptoms: "yellow eyes," "constant tiredness," "pain under my ribs."
And yet, Amazon ratings for black cohosh hover at 4.1 out of 5. Why? Because the people who feel better don’t leave reviews. The people who get hurt? They’re too sick to post.
What’s the Bottom Line?
Black cohosh isn’t worth the risk. The benefits are weak. The dangers are real, unpredictable, and potentially fatal. It’s not just about the supplement itself-it’s about what you’re taking with it. Acetaminophen. Statins. Antibiotics. Even daily vitamins can add up.
There are safer, proven options for managing menopause symptoms: SSRIs, gabapentin, cognitive behavioral therapy, lifestyle changes. They work. They’re studied. They don’t attack your liver.
If you’re considering black cohosh-or already taking it-talk to your doctor. Get your liver checked. And if you’re not sure whether your meds are safe with it? Don’t guess. Ask.
The supplement industry thrives on the idea that "natural" equals "safe." But your liver doesn’t care if it’s from a plant or a lab. It only cares if it can handle the load.








Man, I took this stuff for six months because my wife swore by it. Felt great at first. Then one day I just felt like a wet sock someone left in the gym bag. Turns out my ALT was through the roof. Docs said it was the cohosh + my daily Tylenol for headaches. Never again. Don't be that guy.
One must interrogate the epistemological foundations of the supplement industrial complex. The conflation of "natural" with "benign" is a semantic fallacy rooted in romanticized vitalism-a pre-Enlightenment episteme that persists in neoliberal wellness culture. The liver, as a metabolic organ, operates according to pharmacokinetic law, not folkloric virtue. To presume botanical origin confers safety is to mistake taxonomy for toxicology.
Moreover, the regulatory arbitrage enabling such products to bypass FDA premarket scrutiny constitutes a structural failure of bioethical governance. The absence of mandatory post-marketing surveillance for phytochemicals is not an oversight-it is policy.
Oh here we go again. Another "natural is dangerous" think piece. Did you know aspirin comes from willow bark? And digitalis from foxglove? Plants kill people every day. But somehow, if it’s in a bottle with a hippie on the label, it’s a death trap? LOL. I’ve been taking black cohosh since 2018. Liver enzymes? Perfect. My doctor says so. You’re just scared of plants because you’re a pharma shill.
Y’ALL. I just got my LFTs back. ALT: 890. Bilirubin: 18. I thought I had the flu. Turns out? Black cohosh. And I was taking it with my statin. I’m on the transplant list now. I’m 49. I have two kids. I didn’t even know this was a thing. Please. Please. Read this. Don’t be me.
Thank you for writing this. I’ve been so scared to say anything because everyone says "just take the herb, it’s natural." But I’ve seen too many friends get sick. I’m switching to gabapentin now. My hot flashes are still bad-but at least I’m alive to complain about them.
Just wanted to add-I’m a pharmacist. We don’t always ask about supplements. But we should. If you’re on anything liver-metabolized-antibiotics, pain meds, cholesterol drugs, even some antidepressants-ask your pharmacist about interactions. It’s not their job to guess. It’s yours to speak up.
Black cohosh is a distraction. The real issue? The FDA is controlled by Big Pharma. They want you to take SSRIs because they own the patents. The liver damage? A cover-up. Look at the studies-they’re all funded by pharmaceutical conglomerates. They scare you off herbs so you stay on their $200/month pills. Natural medicine is the only truth. The liver heals itself if you stop the poison… the pharmaceutical poison.
Wait, so if a plant causes liver damage, but a synthetic drug causes the same damage, the plant is evil but the drug is medicine? That’s not logic-that’s hypocrisy. You’re not protecting people. You’re protecting corporate profits. I’ve seen more people die from SSRIs than black cohosh. Where’s the outcry? Where’s the FDA warning? Oh right-because the FDA takes money from the same people who make Lexapro. Wake up.
It is a matter of profound regret that the populace continues to indulge in unregulated botanicals with the same abandon as one would consume illicit narcotics. The hepatic toxicity profile of Cimicifuga racemosa, while statistically infrequent, is not negligible. One must acknowledge the absence of standardized dosing, the variability of phytochemical content across cultivars, and the complete lack of pharmacovigilance infrastructure. This is not medicine. This is alchemy with a barcode.
Canada banned this in 2021. Why are you still selling it? 😡