When you pick up a prescription and see a pill that looks nothing like the one you’ve taken before, it’s natural to wonder: are generic drugs copies? Are they just cheap imitations? Or do they actually work the same way? The answer isn’t as simple as yes or no - but the science is clear.
They’re not copies. They’re equivalents.
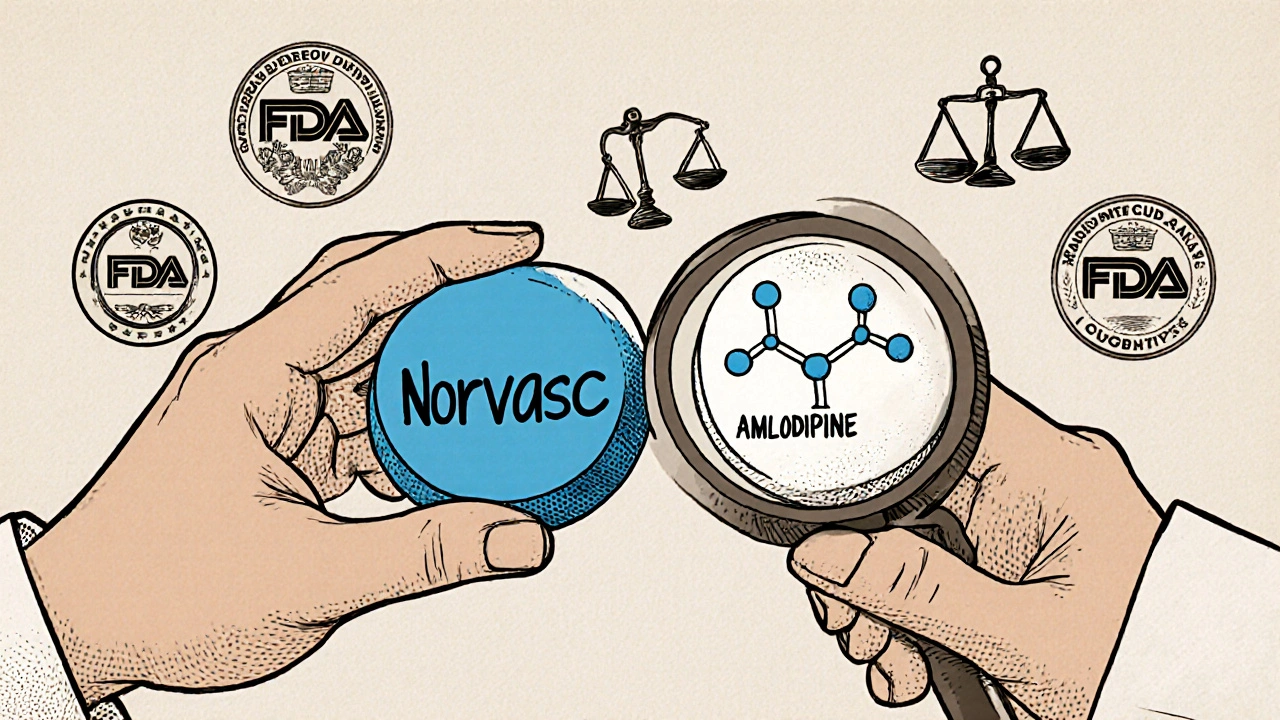
Generic drugs aren’t knockoffs. They’re not made in back-alley labs with unknown ingredients. They’re approved by the U.S. Food and Drug Administration (FDA) as exact therapeutic matches to brand-name drugs. The FDA requires that generic versions contain the same active ingredient, in the same strength, and delivered the same way - whether it’s a pill, injection, or cream. That means if your brand-name drug has 10 milligrams of atorvastatin, the generic has exactly 10 milligrams of atorvastatin. No more, no less.The difference isn’t in what works. It’s in what doesn’t. Generics don’t include the same fillers, dyes, or flavors. That’s why your generic pill might be white and round instead of blue and oval. Those inactive ingredients - called excipients - don’t affect how the drug treats your condition. But they do affect how it looks and sometimes how it tastes. And yes, a few people report feeling different when switching, but that’s usually because of those fillers, not the medicine itself.
How do we know they work the same?
The FDA doesn’t just take a manufacturer’s word for it. Every generic drug must pass a test called bioequivalence. That means scientists measure how quickly and how much of the active ingredient enters your bloodstream compared to the brand-name version. The rule? The generic’s absorption must be within 80% to 125% of the brand’s. That’s not a guess. It’s a strict scientific standard.For example, if the brand-name drug releases its medicine into your blood over 6 hours, the generic must do the same - within a tiny margin of error. Studies show that 96% of non-critical medications switch seamlessly from brand to generic without any change in results. That includes common drugs like lisinopril for high blood pressure, omeprazole for heartburn, and simvastatin for cholesterol. Millions of people take generics every day without knowing the difference.
What about the expensive ones?
The biggest savings come from generics. In 2023, the average brand-name prescription cost $61.85. The generic? $4.27. That’s an 85% drop. The Congressional Budget Office found that generics saved U.S. patients over $313 billion in one year alone. Without them, many people would skip doses or stop taking their meds altogether. A Harvard study showed that 25% of patients on brand-name drugs didn’t fill their prescriptions because of cost. Only 8% of those on generics did the same.It’s not just about saving money. It’s about staying healthy. When a diabetic can afford their metformin, when a heart patient takes their beta-blocker daily, when someone with asthma gets their inhaler - those are real outcomes. Generics make that possible.
Are there exceptions?
Yes. And this is where the myth gets tangled. Some drugs have what’s called a narrow therapeutic index (NTI). That means even a tiny change in blood levels can cause serious problems - too little and the drug doesn’t work; too much and it becomes toxic. These include warfarin (a blood thinner), levothyroxine (for thyroid disease), and certain seizure medications like phenytoin.For these, the FDA and doctors recommend caution. Some patients do better staying on the same brand. But that doesn’t mean generics are unsafe. It means these drugs need closer monitoring. A 2022 study by Cedars-Sinai found that most issues with NTI drugs weren’t caused by the generic itself, but by switching back and forth between different generic brands. Stability matters more than brand.
Even here, data shows 92% of substitutions work fine with proper oversight. The Epilepsy Foundation reported that 17% of patients had breakthrough seizures after switching - but follow-up analysis by the FDA found most cases were linked to missed doses, stress, or illness, not the drug’s effectiveness.
Why do people still doubt them?
A lot of it comes down to appearance and marketing. Brand-name drugs spend billions on ads. They look polished. They have names you recognize. Generics? They’re plain. No commercials. No logos. Just a name like “amlodipine” instead of “Norvasc.” That makes people think they’re inferior. But here’s the truth: the FDA tested over 2,000 generic drugs and found they contained 99.2% of the labeled active ingredient on average. That’s better than many brand-name versions.Another myth: generics are made overseas and are lower quality. In reality, 40% of generic drugs sold in the U.S. are made in American factories. The rest come from countries with FDA-approved facilities - the same ones that make brand-name drugs. The FDA inspects all of them, regularly and without warning.
What do pharmacists see?
Pharmacists are on the front lines. They fill prescriptions, answer questions, and watch for reactions. Most say patients don’t notice a difference - unless they’re told to expect one.One pharmacist in Bristol told me about a patient who refused her generic blood pressure pill because it was “too small.” She’d been on the brand for years. When they switched her back, she said, “I feel like I’m taking something stronger.” She wasn’t. The dose was identical. But her brain had been conditioned to believe the bigger, branded pill meant better results.
Pharmacists spend an average of 3.2 minutes per prescription explaining this. Many patients still walk out confused. A Brown University survey found that 43% of people believe generics contain only 20-80% of the active ingredient. That’s not true. It’s almost always 99%.
What’s changing now?
The system is getting faster. In 2018, the FDA had over 4,200 generic applications waiting. Thanks to new funding and streamlined processes under GDUFA IV, they’re aiming to cut approval time to just 10 months by 2027. That means more generics hitting the market sooner - and lower prices.Complex drugs like inhalers, injectables, and topical creams are next in line. These are harder to copy because the delivery system matters as much as the ingredient. But progress is happening. The FDA’s 2023 plan targets 95% approval rates for priority generics by 2025.
And Medicare Part D - the prescription program for seniors - now automatically switches to generics unless a doctor says otherwise. That’s expected to save $156 billion over ten years. For older adults on fixed incomes, that’s life-changing.
Should you take them?
For 95% of medications, the answer is yes - and here’s why:- You get the same active ingredient
- You get the same effectiveness
- You pay a fraction of the price
- You’re not risking your health
Only in rare cases - like NTI drugs - should you consider sticking with a brand. Even then, it’s not about the generic being bad. It’s about consistency. Once you find a generic that works, stick with it. Don’t switch between different generic brands unless your doctor says so.
If you’re unsure, ask your pharmacist. They can tell you if your drug is a simple generic or one that needs extra care. They can also check if your insurance covers the brand at the same price - sometimes it does, especially if the generic just came out.
Don’t let the look fool you. A white pill isn’t weaker. A small tablet isn’t less effective. And a lower price doesn’t mean lower quality. It just means the patent ran out - and now you get to benefit from it.
Are generic drugs just as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict safety, strength, quality, and purity standards as brand-name drugs. Every generic is tested and inspected before it reaches shelves. Between 2018 and 2022, the FDA reviewed over 1,800 reports of possible issues with generics - and only 5.5 cases per year were confirmed as actual failures. That’s less than 0.3%.
Why do generic pills look different?
U.S. trademark laws require generics to look different from brand-name versions. That means different colors, shapes, or markings. But the active ingredient - the part that treats your condition - is identical. The differences are only in inactive ingredients like fillers or dyes, which don’t affect how the drug works.
Can I trust generics made outside the U.S.?
Yes. The FDA inspects all manufacturing facilities - whether they’re in the U.S., India, China, or elsewhere - before approving a generic drug. Over 40% of generic pills sold in the U.S. are made in American factories. The rest come from international sites that meet the same standards as U.S. plants. The FDA conducts thousands of inspections each year.
Do generics take longer to work?
No. Generic drugs must prove bioequivalence - meaning they enter your bloodstream at the same rate and to the same extent as the brand-name version. Studies show the absorption time is virtually identical. If you feel a delay, it’s likely psychological or due to changes in inactive ingredients affecting how quickly the pill dissolves in your stomach.
Should I always choose the generic?
For most drugs, yes. Generics are equally effective and save you money. But for a small group of drugs with a narrow therapeutic index - like warfarin, levothyroxine, or certain seizure meds - your doctor may recommend sticking with one version (brand or generic) to avoid fluctuations. Always talk to your doctor or pharmacist before switching.
Why do some people say generics don’t work for them?
Sometimes, it’s the inactive ingredients causing minor side effects - like stomach upset or a different taste. Other times, people notice a change because they expect one. Studies show 82% of users report identical effectiveness. If you feel worse after switching, talk to your pharmacist. It might be a different generic brand, or you might need to go back to your original version - but it’s rarely because the generic is inferior.





Man, I remember when I first switched to generics in Dublin after my insurance dropped the brand-name stuff. Thought I was gonna keel over from some weird side effect. Turns out my brain was just screaming because the pill was a different color. Same active ingredient, same results. People freak out over aesthetics like it’s a fashion show. The FDA doesn’t play games. If it’s approved, it works. End of story.
It’s wild how much we trust logos and packaging more than science. A white pill doesn’t feel as ‘legit’ as a blue one with a fancy logo, even though both have the same chemistry inside. We’re wired to equate appearance with quality. But medicine isn’t perfume. It doesn’t need a scent or a glitter finish to save your life.
Let me tell you what really happened to my cousin. She was on levothyroxine for 12 years. Switched to generic because her deductible was insane. Two weeks later she started having panic attacks, hair falling out, heart palpitations. She swore the generic was poison. Went back to brand. Instant relief. Now she’s convinced the pharmaceutical industry is hiding something. And honestly? I don’t blame her. The system is broken when a person’s thyroid health hinges on which white pill they get. It’s not paranoia. It’s survival.
in india generics are the only option. no one can afford brand. but i have seen people switch between different generic brands and get sick. not because the drug is bad but because the fillers change. one brand uses lactose, another uses corn starch. people with sensitivities don’t know. no one tells them. the system assumes everyone is the same. but bodies are not factories.
40 percent made in usa sure but the rest are inspected once every 5 years and most factories are in india and china where corruption is normal. the FDA is a joke. they approve based on paperwork not reality. i know people who got sick from generics. no one listens.
Generics are the unsung heroes of public health. If you’re on a fixed income and your meds cost $4 instead of $60 you’re not just saving money-you’re staying alive. No drama. No fluff. Just science and access. Stop letting marketing fool you.
ok but like… why do they make the generic pills so tiny?? like i get it they dont need the fancy dye but why make em the size of a poppy seed?? i took my blood pressure med and thought i swallowed a bug. then i checked the bottle and it was the same dose. just… smaller. my brain hates it. i feel like its not working. its not the chemistry its the vibes.
Look, I get why people are nervous. I used to be one of them. But I’ve worked in community health for over a decade. I’ve seen patients who couldn’t afford their meds stop taking them entirely. Then they end up in the ER with a stroke or heart attack. Generics keep people out of hospitals. They’re not perfect, but they’re the most equitable solution we’ve got. The real villain isn’t the white pill-it’s a system that lets drug companies charge $200 for a pill that costs $2 to make.
It is deeply concerning that the public continues to harbor such irrational fears regarding pharmacological equivalence. The FDA’s bioequivalence thresholds are grounded in rigorous statistical methodology, and the data demonstrating therapeutic interchangeability is overwhelming. To suggest that a pill’s color or size correlates with efficacy is not merely misguided-it is antithetical to the principles of evidence-based medicine. One must ask: if the active ingredient is identical, the pharmacokinetics are equivalent, and the manufacturing facilities are subject to the same inspection protocols, then on what empirical basis does one reject the generic? The answer, regrettably, lies not in science, but in psychological conditioning and corporate propaganda.
My mom’s on warfarin. They switched her to generic. She didn’t feel different. But her INR went nuts. They had to tweak the dose twice. Now she’s back on brand. Not because generics are bad. But because for some drugs, consistency matters more than cost. If your doc says stick with one version-do it. Don’t switch between generics. That’s where the real risk is.