Azathioprine Dose Calculator
Dose Calculator
How This Works
This calculator determines safe azathioprine dosing based on TPMT enzyme activity and NUDT15 variants. For patients with low enzyme activity or NUDT15 variants, lower doses are required to prevent life-threatening bone marrow suppression. Always consult your doctor before starting or adjusting medication.
Recommended Dose:
0 mg/dayWhen you’re prescribed azathioprine for Crohn’s disease, lupus, or after a transplant, you’re not just taking a pill-you’re trusting your body’s chemistry to handle it safely. But what if your body can’t process it the way most people can? That’s where TPMT testing comes in. It’s not a routine blood test. It’s a genetic check that can stop a rare but deadly side effect before it starts.
Why Azathioprine Can Be Dangerous
Azathioprine has been used for over 60 years to calm down overactive immune systems. It’s cheap-often under $50 a month-and effective for long-term control of autoimmune conditions. But for some people, it turns dangerous. The drug breaks down into active compounds that attack rapidly dividing cells, like those in bone marrow. That’s why it works: it slows down the immune system. But if your body makes too much of those active compounds, your blood cell counts can crash.Severe myelosuppression isn’t just a bump in the road. It means your white blood cells, red blood cells, and platelets drop to dangerously low levels. You become vulnerable to infections, fatigue, bleeding, and hospitalization. In the worst cases, it’s fatal.
About 15 to 28% of people on azathioprine experience side effects. Nausea is common. But the real threat? A hidden genetic flaw that no doctor can spot just by looking at you.
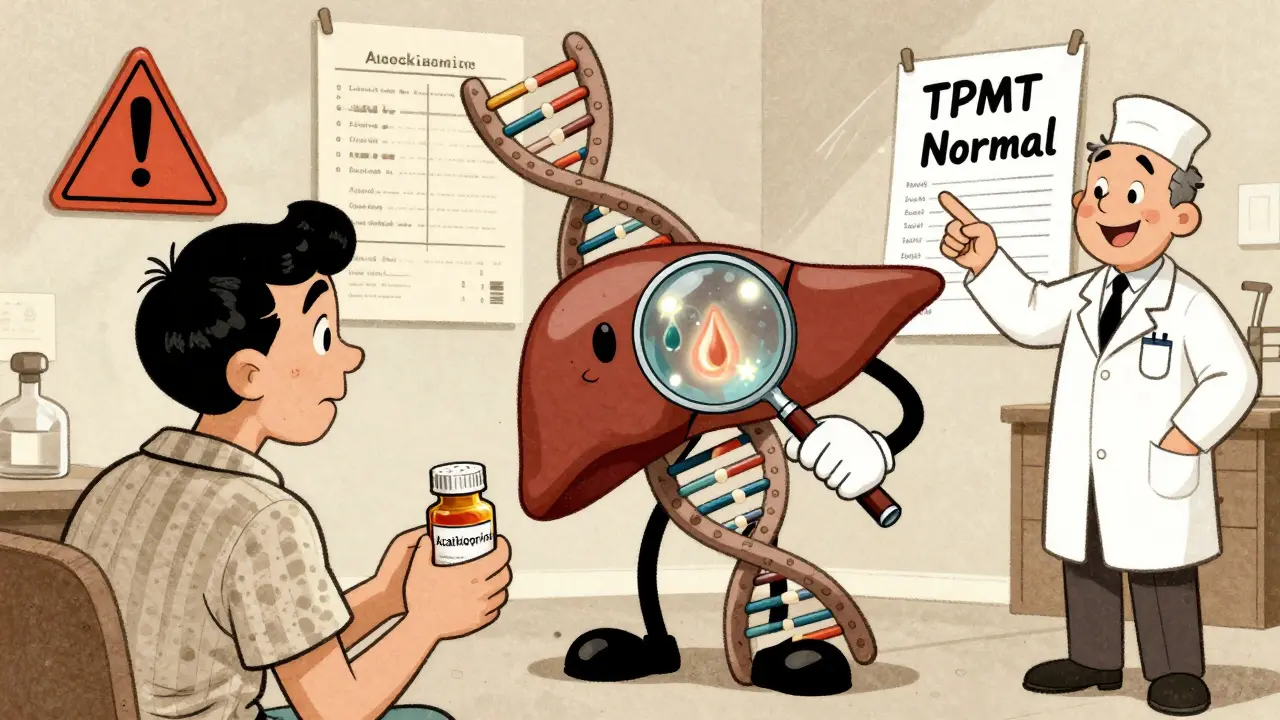
What Is TPMT and Why Does It Matter?
TPMT stands for thiopurine methyltransferase. It’s an enzyme your liver makes to break down azathioprine and keep it from building up. Think of it like a safety valve. Most people have normal levels-enough to handle the standard dose. But about 1 in 300 people inherit two faulty copies of the TPMT gene. They have almost no enzyme activity. For them, even a tiny dose of azathioprine can be toxic.Another 1 in 10 people have one working copy and one faulty copy. Their enzyme activity is reduced. They can still take azathioprine, but they need a much lower dose. Without knowing this, they’re walking into a minefield.
Before TPMT testing became common, doctors had to guess. They’d start at 2 mg per kg of body weight and hope for the best. Blood counts were checked every few weeks. By the time a drop in white cells showed up, damage was already done. Some patients lost their lives to this delay.
How TPMT Testing Works
There are two ways to test for TPMT status: genotyping and phenotyping.Genotyping looks at your DNA. It checks for specific gene variants-like *2, *3A, *3B, and *3C-that tell you if you’re at risk. It’s accurate, fast, and not affected by recent blood transfusions. Results come back in a few days.
Phenotyping measures enzyme activity directly in your red blood cells. It’s useful, but if you’ve had a transfusion recently, the results are unreliable. Your donor’s blood cells will skew the numbers. That’s why genotyping is now the preferred method.
The American Gastroenterological Association (AGA) and the European Crohn’s and Colitis Organisation (ECCO) both recommend testing before starting azathioprine. The CPIC (Clinical Pharmacogenetics Implementation Consortium) has clear guidelines: if you’re homozygous deficient (no enzyme), don’t use azathioprine. Use methotrexate or a biologic instead. If you’re heterozygous (low enzyme), start at 30-70% of the normal dose and check your blood counts weekly for the first month.
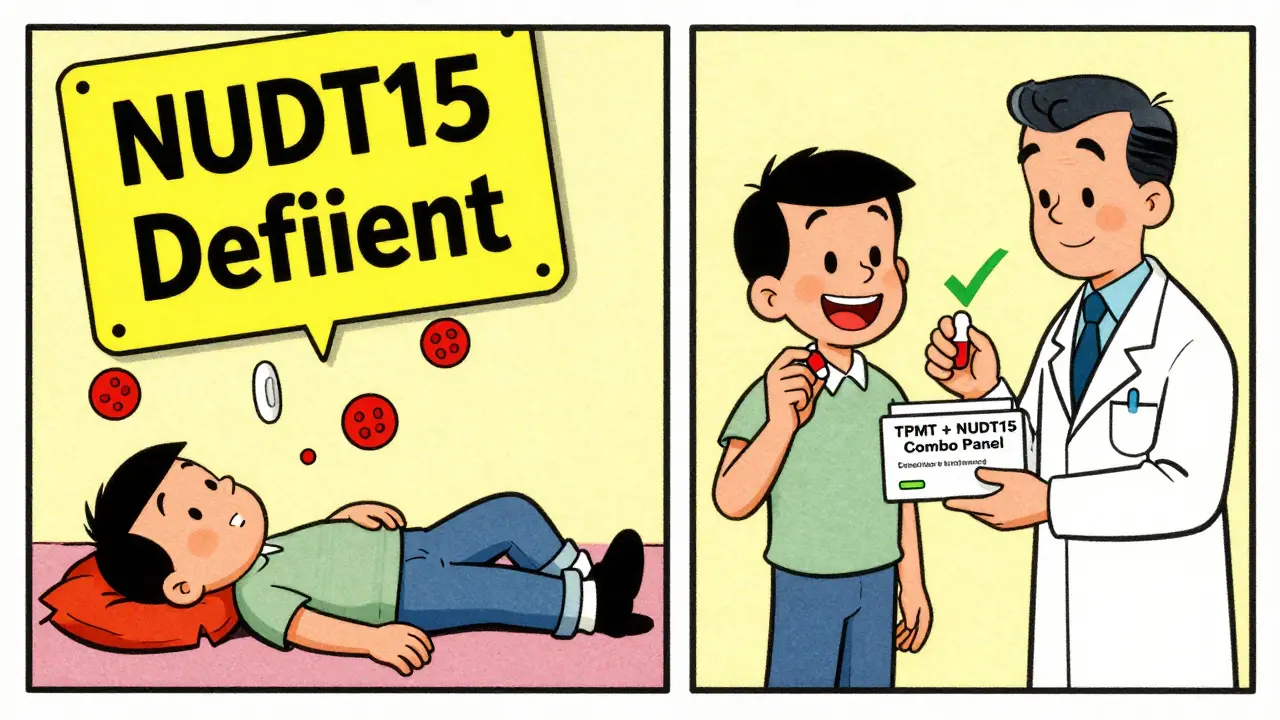
The NUDT15 Factor
TPMT isn’t the whole story. In Asian populations-people of Chinese, Korean, Thai, or Filipino descent-another gene, NUDT15, plays a bigger role. Up to 20% of these individuals carry variants that make them extremely sensitive to azathioprine. Their risk of severe bone marrow suppression is just as high as those with TPMT deficiency.The FDA updated azathioprine’s label in 2019 to include NUDT15. The CPIC followed in 2022 with updated dosing rules. Now, the best practice isn’t just TPMT testing-it’s testing for both genes together. Many labs now offer combined panels. If you’re of Asian heritage, this isn’t optional. It’s essential.
What the Studies Say
A 2011 randomized trial with 333 patients found something surprising: TPMT testing didn’t cut overall side effects. The group that got tested had 29% adverse reactions; the group that didn’t had 28%. That sounds like no difference. But look closer.The test caught the one patient who was homozygous deficient. That person had severe neutropenia. Without testing, they might have died. The other side effects-nausea, liver issues, pancreatitis-weren’t linked to TPMT at all. That’s the key: TPMT testing prevents the rare, catastrophic events. It doesn’t stop the common ones.
Another study in JAMA Dermatology found that only 1 out of 13 patients who had to stop azathioprine due to toxicity had low TPMT activity. That means most side effects come from other causes: drug interactions, liver problems, or unknown factors.
So TPMT testing isn’t a magic shield. But it’s the only shield you have against the one thing that can kill you.
What You Can’t Rely On
Some patients assume that if their TPMT test is normal, they’re safe. That’s not true. Hepatotoxicity affects 7.4% of users. It has nothing to do with TPMT. Photosensitivity? That’s another risk. You need sunscreen. Nausea? It’s common, but often fades with time. And if you’re taking allopurinol-for gout-that’s a red flag. Allopurinol blocks the same enzyme pathway as azathioprine. Even with normal TPMT, the combo can cause life-threatening toxicity.The NCBI and CPIC are clear: TPMT and NUDT15 testing don’t replace blood tests. They complement them. You still need weekly CBCs for the first month, then monthly. Liver enzymes too. No genetic test can predict every problem.

Cost, Access, and Real-World Use
TPMT testing costs $200-$400 in the U.S. Most private insurers cover it. Medicaid coverage varies. In the UK, NHS hospitals often do it routinely for IBD patients. In community clinics or rural areas, it’s still not standard.Why? Because some doctors don’t know the guidelines. Others think it’s too expensive. But consider this: one hospital stay for pancytopenia can cost $20,000. The test pays for itself.
Adoption rates vary. In U.S. academic centers, 50-60% of patients get tested. In Europe, it’s closer to 80%. In non-gastroenterology practices-like rheumatology or dermatology-it’s often skipped. That’s a problem. Azathioprine isn’t just for IBD. It’s used in lupus, vasculitis, and severe eczema. Every prescriber needs to know.
What to Do Next
If you’re about to start azathioprine:- Ask your doctor if TPMT and NUDT15 testing is available.
- If you’re of Asian descent, insist on both tests.
- Don’t start the drug until you have the results.
- If you’re homozygous deficient, switch to methotrexate or a biologic.
- If you’re heterozygous, expect a lower starting dose-maybe 50 mg instead of 100 mg.
- Get weekly blood tests for the first month. Report fatigue, fever, or bruising immediately.
- Tell every doctor you see that you’re on azathioprine. Especially if you’re prescribed allopurinol, sulfasalazine, or ACE inhibitors.
The Bottom Line
Azathioprine is a powerful tool. But it’s not safe for everyone. TPMT and NUDT15 testing don’t guarantee you won’t have side effects. But they give you the only real chance to avoid the one that could kill you. For less than the cost of a few months’ worth of medication, you get a clear roadmap for safety.Don’t wait for symptoms to appear. Ask for the test before you take the first pill. Your bone marrow will thank you.
Is TPMT testing required before taking azathioprine?
No, it’s not legally required, but major medical guidelines-including those from the American Gastroenterological Association and the Clinical Pharmacogenetics Implementation Consortium-strongly recommend it. Many hospitals and specialists do it routinely. Skipping it puts you at risk for severe, avoidable toxicity.
Can I still take azathioprine if I have low TPMT activity?
If you have intermediate (heterozygous) TPMT activity, yes-but at a reduced dose, usually 30-70% of the standard amount. If you have severe deficiency (homozygous), azathioprine is not safe. Your doctor will switch you to methotrexate, mycophenolate, or a biologic like infliximab.
Does TPMT testing work for everyone?
No. TPMT testing only explains part of the risk. About 70% of severe side effects come from other causes: drug interactions (like with allopurinol), liver issues, or other genes like NUDT15. That’s why blood tests (CBC, liver enzymes) are still essential-even if your genetic test is normal.
How long does TPMT testing take?
Results usually come back in 3 to 7 days. Some labs offer faster turnaround. If you’re in a hurry, ask if your provider can order a genotyping test-those are faster than enzyme activity tests. Don’t start azathioprine until you have the results.
Is TPMT testing covered by insurance?
Most private insurers in the U.S. cover it. Medicare and Medicaid coverage varies by state. In the UK, the NHS typically covers it for IBD patients. Check with your provider. The cost is often less than $400, and avoiding one hospitalization can save thousands.
What if I’ve already been on azathioprine for months without problems?
If you’ve been stable for over six months with normal blood counts, the risk of sudden severe myelosuppression drops significantly. But if you’ve never been tested, it’s still worth asking your doctor about it-especially if you develop new symptoms like unexplained fatigue or bruising. You may still benefit from knowing your status for future treatments.
Can I get TPMT testing done without a doctor’s order?
Some direct-to-consumer labs offer pharmacogenomic testing, but they’re not always reliable for clinical decisions. TPMT testing should be ordered by your prescriber so results are interpreted in context with your medical history and other medications. Never rely on a home test alone.