Pediatric Antihistamine Dosing Calculator
Calculate the correct dose based on your child's weight and the antihistamine type. Always use a proper dosing syringe or cup - never a kitchen spoon.
Recommended Dose
Safe for childEnter child's weight to see the recommended dose.
How to Use This Calculator
1. Always use the oral syringe or dosing cup that came with the medication 2. Check the concentration on the bottle (e.g., 12.5 mg per 5 mL) 3. Never use a kitchen spoon - they vary widely in size 4. For first-generation antihistamines like Benadryl, use weight-based dosing 5. Second-generation antihistamines (Zyrtec, Claritin) are safer for children
Every year, thousands of children end up in emergency rooms because someone gave them the wrong amount of antihistamine. It’s not because parents are careless-it’s because the system is confusing. One teaspoon of Children’s Benadryl isn’t the same as one teaspoon of Zyrtec. And if you use a kitchen spoon? You might be giving your child three times too much. These aren’t hypothetical risks. In 2022, over 21,000 children under six were reported to poison control centers for antihistamine exposure. Most of these cases were preventable.
Why Dosing Errors Happen
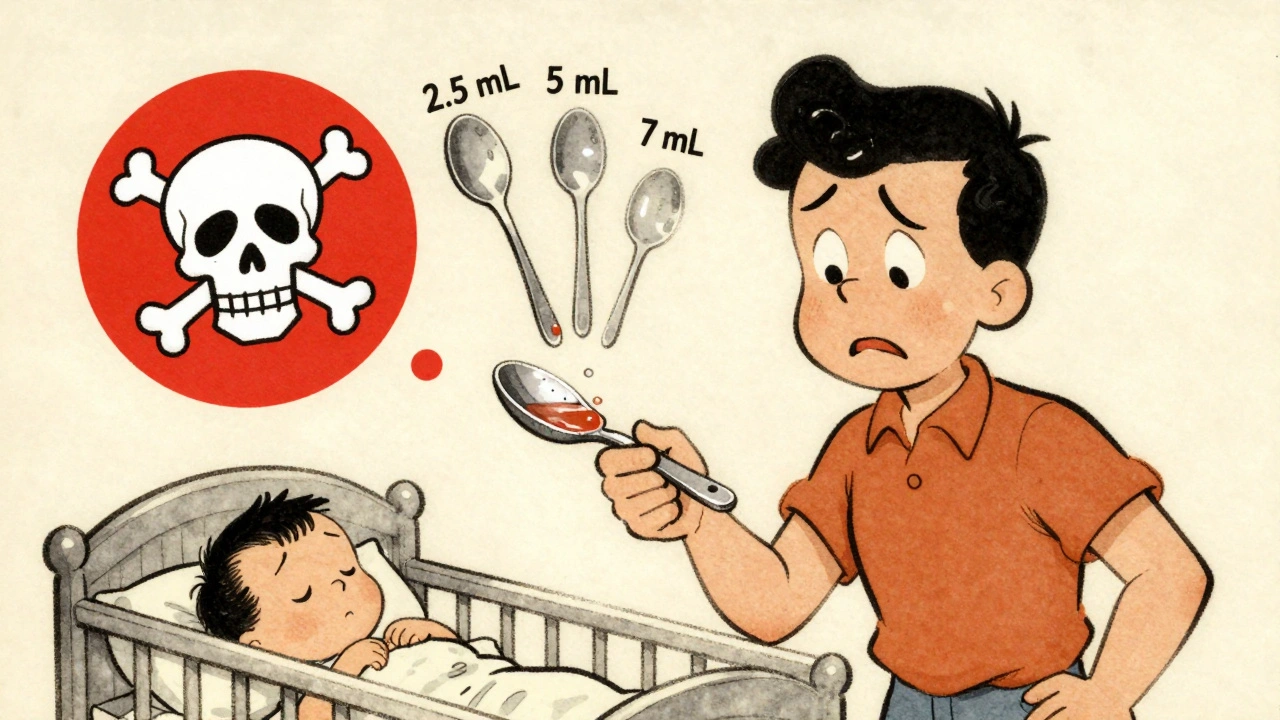
The biggest problem? Measurement. Parents aren’t trained pharmacists. They’re tired, stressed, and trying to help their sick child. They reach for a spoon because it’s right there. But a kitchen teaspoon can hold anywhere from 2.5 to 7.5 milliliters. That’s a 300% difference in dose. A 2015 study in the Annals of Internal Medicine showed this simple mistake leads to dangerous overdoses more often than you’d think. Then there’s the confusion between formulations. Children’s diphenhydramine (Benadryl) liquid is 12.5 mg per 5 mL. That’s 2.5 mg per mL. But adult Benadryl tablets are 25 mg or 50 mg. A grandparent might grab the adult bottle, thinking it’s the same. One case documented by the FDA involved a 23-month-old who got 50 mg-four times the correct dose-after a grandparent confused adult and children’s bottles. The child spent two days in the hospital with respiratory distress. Another issue: dosing by age instead of weight. Charts often list “1-2 years: 5 mg.” But a 1-year-old weighing 20 pounds needs a different dose than a 1-year-old weighing 30 pounds. Weight matters. The American Academy of Pediatrics says weight-based dosing is the only safe way to calculate antihistamine amounts.First-Generation vs. Second-Generation Antihistamines
Not all antihistamines are created equal. First-generation drugs like diphenhydramine (Benadryl) cross the blood-brain barrier easily. That’s why they make adults drowsy-and why they can cause seizures, hallucinations, or breathing problems in kids. Their therapeutic index is narrow: the difference between a helpful dose and a toxic one is just about 2 to 1. That’s like walking a tightrope. Second-generation antihistamines like cetirizine (Zyrtec) and loratadine (Claritin) don’t cross the brain barrier as easily. They’re safer. Their therapeutic index is around 10 to 1. That means you’d need to give a child five times the right dose before hitting danger. That’s why they’re now the go-to choice for pediatric allergies. Yet diphenhydramine is still widely used. Why? It’s cheap. It’s available everywhere. And many parents still think it’s the best for colds or sleep. But the American College of Allergy, Asthma, and Immunology found that 78% of ER visits for antihistamine reactions involve kids under six-and 67% of pediatricians say parents use it unnecessarily for colds, not allergies. The FDA and AAP now strongly advise against using diphenhydramine in children under two.The Measurement Trap
Even if you get the right dose, you still need the right tool. The FDA has required all pediatric liquid medications to come with an oral syringe or dosing cup marked in milliliters since 2011. But a 2018 study in Pediatrics found that 42% of caregivers still use kitchen spoons, shot glasses, or droppers not meant for medicine. Here’s what you need to know:- 1 teaspoon = 5 mL
- 1 tablespoon = 15 mL
- Never use a kitchen spoon
- Always use the syringe or cup that came with the bottle
- Check the concentration: is it 12.5 mg/5 mL? 5 mg/5 mL? 10 mg/5 mL?

How to Get It Right
You don’t need to be a doctor to give your child antihistamine safely. Here’s how:- Use weight, not age. Find your child’s weight on the dosing chart. If you don’t know it, weigh them on a bathroom scale: hold them, step on, then subtract your weight.
- Use the syringe that came with the bottle. If it’s missing, ask your pharmacy for a new one. They’re free.
- Double-check the concentration. Look at the label. Is it 12.5 mg per 5 mL? 5 mg per 5 mL? Write it down.
- Never use adult medicine for kids. Even if you cut a tablet in half, the fillers and coatings aren’t designed for children.
- Ask your pharmacist to show you. Say: “Can you demonstrate how to measure this?” Most will happily do it.
What to Do If You’re Not Sure
If you’re confused, don’t guess. Don’t give half a teaspoon and hope it’s enough. Don’t give another dose because your child spit it out. Instead:- Call Poison Control at 1-800-222-1222. They’re available 24/7.
- Text your pharmacy. Many have live chat.
- Wait. If your child isn’t in distress, wait until morning to confirm with your pediatrician.

Why This Matters Long-Term
The good news? Things are getting better. Since 2019, pediatric antihistamine overdoses have dropped 19% year over year. Hospitals now use electronic systems that flag weight-based dosing errors before they happen. The FDA is testing QR codes on bottles that link to instructional videos. Pilot programs at Boston Children’s Hospital cut dosing errors by 53%. But progress depends on parents. You’re the last line of defense. When a grandparent hands your child a spoonful of Benadryl because “it worked for me,” you need to know why that’s dangerous. When a friend says “my kid takes Zyrtec every night for sleep,” you need to know that’s not approved-and it’s risky. Second-generation antihistamines are safer, simpler, and more effective for daily use. Diphenhydramine should be reserved for emergencies-like a sudden allergic reaction with swelling or trouble breathing-and even then, only if you’re certain of the dose.Final Checklist
Before giving any antihistamine to your child, ask yourself:- Is this the right drug? (Avoid diphenhydramine for routine use under age 2)
- Is this the right dose? (Based on weight, not age)
- Is this the right tool? (Oral syringe, not spoon)
- Is this the right concentration? (Check the label: mg per mL)
- Am I sure? (If not, call Poison Control)
Can I give my 1-year-old Benadryl for a cold?
No. The FDA and American Academy of Pediatrics strongly advise against using first-generation antihistamines like diphenhydramine (Benadryl) in children under 2 for colds or sleep. These drugs don’t treat cold symptoms effectively and carry a high risk of serious side effects like seizures, breathing problems, and extreme drowsiness. For colds, focus on fluids, rest, and saline drops. Use antihistamines only for confirmed allergies, and only with second-generation options like loratadine or cetirizine if recommended by a doctor.
Is it safe to use a kitchen spoon to measure children’s antihistamine?
No. Kitchen spoons vary in size from 2.5 mL to 7.5 mL. That means you could be giving your child up to three times too much or too little. Even a small difference can be dangerous with medications like diphenhydramine, which has a narrow safety margin. Always use the oral syringe or dosing cup that comes with the medicine. If you lost it, ask your pharmacy for a free replacement.
What’s the difference between Children’s Zyrtec and Children’s Benadryl?
Children’s Zyrtec (cetirizine) is 1 mg per mL, and it’s a second-generation antihistamine-less likely to cause drowsiness or serious side effects. Children’s Benadryl (diphenhydramine) is 2.5 mg per mL and is a first-generation drug that crosses into the brain, causing sedation and increasing the risk of overdose. A 5 mL dose of Zyrtec is 5 mg. A 5 mL dose of Benadryl is 12.5 mg. Giving the same volume of both is a 2.5x overdose of diphenhydramine. Never substitute one for the other without checking the label and dose.
My child spit out the medicine. Should I give another dose?
Don’t give another dose unless you’re certain your child spit out almost all of it. If they swallowed even a small amount, giving more could lead to overdose. Instead, wait and contact your pediatrician or Poison Control. Re-dosing is one of the most common causes of accidental overdose in children. If your child consistently spits out medicine, ask your pharmacist about flavored versions or techniques to help them swallow safely.
Are chewable antihistamines safe for toddlers?
Chewable tablets pose a choking hazard for children under 4. The FDA’s MAUDE database shows that 12% of pediatric medication errors involve choking on chewable tablets. For kids under 4, always use liquid formulations with a dosing syringe. If your child is 4 or older and can safely chew, make sure they’re supervised and understand how to chew and swallow properly. Never let them run around with a tablet in their mouth.









Let me get this straight - you’re telling me parents are still using kitchen spoons in 2024? Bro. We have smartphones that can identify birds by their song, but you can’t grab a $2 syringe from the pharmacy? This isn’t negligence, it’s a public health farce. And don’t even get me started on grandmas handing out Benadryl like it’s candy. I’ve seen it. My cousin’s kid ended up in the ER because ‘it worked for me in the 80s.’
Oh wow another article about how dumb people are. Shocking. The real issue isn’t dosing - it’s that we’ve outsourced basic responsibility to pharmaceutical companies and the state. You don’t need a syringe. You need a brain. If you can’t read a label or measure 5 mL, maybe you shouldn’t be medicating children. This isn’t rocket science. It’s reading. And yet we treat it like quantum physics. Pathetic.
I’ve been a pediatric nurse for 18 years and I still get parents asking if Zyrtec and Benadryl are interchangeable. I don’t judge - I just show them the label, hand them a syringe, and say ‘this is your new best friend.’ The system is broken, but most people aren’t trying to hurt their kids. They’re just overwhelmed. A little patience, a free syringe, and a 30-second chat can save a life. No heroics needed. Just human connection.
The fundamental epistemological flaw in contemporary pediatric pharmacology lies not in the pharmacokinetics of antihistamines, but in the ontological dislocation of parental agency from scientific literacy. The commodification of health information has resulted in a hermeneutic vacuum wherein laypersons rely on heuristic substitution rather than evidence-based decision-making. The syringe is not a tool - it is a symbol of institutional trust, and its absence reflects a deeper societal failure.
I gave my 14-month-old half a teaspoon of Benadryl last week because she was sneezing and I thought it would help. I’ve been crying ever since. I’m not a bad mom. I’m just tired. I didn’t know the concentration was different. I thought all kids’ medicine was the same. Now I’m scared to give her anything. What if I did permanent damage? I can’t sleep. I keep checking her breathing. I don’t know what to do. Please tell me she’s okay.
How tragic. In India, we have no such luxury. We use whatever is available. If the bottle has no syringe? We use a clean teaspoon. If the label is in English and we can’t read it? We ask the neighbor. This isn’t ignorance - it’s survival. You Americans have the luxury of overthinking dosing. We have the burden of under-resourcing. Don’t lecture us about syringes when your hospitals charge $500 for a child’s visit.
Let’s be clear: the 21,000 pediatric antihistamine exposures are not accidents. They are the predictable outcome of a culture that has abandoned personal responsibility in favor of institutionalized ignorance. Parents are not victims. They are participants in a systemic collapse of basic competence. The solution is not more syringes. It is mandatory parental education. Or better yet - ban non-prescription pediatric antihistamines entirely. Let doctors decide. They’re trained. You’re not.
Bro, I’m from India and I’ve given my son Zyrtec for 2 years. No syringe. Just the cap. I shake it, fill it to the brim, and give it. He’s fine. You think I don’t care? I care too much. But what else can I do? The pharmacy doesn’t give syringes. The bottle doesn’t come with one. You think I’m playing Russian roulette? I’m trying. And if I mess up, I’ll go to the hospital. That’s all I can do. Stop acting like you’re better than me.
My daughter used to spit out everything so I asked the pharmacist for a flavored version. They gave me one with cherry and a free syringe. That’s it. No lecture. No guilt. Just help. I wish more places did that. It’s not about being perfect. It’s about being supported. And honestly? If you’re scared you gave the wrong dose? Call Poison Control. They don’t judge. They just help. I did it once. They walked me through it. I felt like a hero for asking.
Every parent wants to do right by their child. The problem isn’t bad intentions - it’s bad design. Labels are tiny. Concentrations change between brands. Syringes disappear. And we’re expected to be pharmacists on 3 hours of sleep. We need standardized dosing across all brands. One color for 1 mg/mL. Another for 2.5 mg/mL. QR codes on every bottle. Simple. Universal. No reading required. That’s the real fix. Not blaming parents. Fixing the system.
Wait - so Zyrtec is safer than Benadryl? That’s new. I’ve been using Benadryl for my kid’s allergies since he was born because it makes him sleepy and he sleeps through the night. So now you’re saying that’s dangerous? But it works! If it’s not broken, why fix it? You’re telling me to switch to something that doesn’t knock him out? Then what’s the point? He’s not allergic. He just won’t sleep. Benadryl fixes that. You’re just making life harder.
Thank you for this. 🙏 I used to use a spoon. Now I keep 3 syringes in my diaper bag. One for each kid. One for Zyrtec. One for Benadryl (only for emergencies). One for tylenol. I label them. I’m not cool. But my kids are safe. And if you’re scared? Call 1-800-222-1222. They’re real people. And they’ve heard it all. You’re not alone. 💙