Opioid & Antihistamine Safety Checker
Important Safety Information
Combining opioids with first-generation antihistamines (like Benadryl) can cause life-threatening breathing suppression. This tool helps identify dangerous combinations.
Combining opioids with antihistamines might seem harmless-after all, many people take over-the-counter allergy meds like Benadryl for a runny nose or itchy skin while also using prescription painkillers. But this mix can be deadly. Both drugs slow down your brain’s control over breathing. Together, they don’t just add up-they multiply the danger.
Why This Combination Is So Dangerous
Opioids like oxycodone, hydrocodone, and fentanyl work by binding to receptors in your brain and spinal cord to block pain. But they also depress the part of your brain that tells you to breathe. That’s why people on high doses can stop breathing entirely, especially when they’re asleep. First-generation antihistamines-like diphenhydramine (Benadryl), hydroxyzine (Atarax), and doxylamine (Unisom)-do something similar. They cross into the brain and block histamine, which normally keeps you alert. That’s why you get sleepy after taking them. But they don’t just make you drowsy. They also suppress the brainstem’s drive to breathe. When you take both at the same time, your body gets hit with a double hit to its breathing control system. There’s no safety buffer. Your brain doesn’t know how to compensate. It just shuts down. The FDA warned about this in 2016, specifically calling out combinations with other CNS depressants-including antihistamines. Since then, case reports keep pouring in. One 68-year-old man in North Carolina ended up in the ICU after taking hydrocodone for back pain and Benadryl for itching. He was unresponsive for 36 hours. Another patient fractured her hip after falling asleep while on oxycodone and hydroxyzine. Neither knew the risks.Who’s at Highest Risk?
Not everyone who takes this combo will have a problem. But some people are far more vulnerable. Older adults are at the top of the list. Their bodies clear drugs slower. Their brains are more sensitive to sedation. The Beers Criteria, used by geriatric specialists, lists diphenhydramine and hydroxyzine as potentially inappropriate for people over 65 because of their strong anticholinergic effects. These drugs can cause confusion, falls, urinary retention, and worse. People with COPD or sleep apnea are also in danger. Their lungs already struggle to get enough oxygen. Add opioids and antihistamines, and their breathing can stop during sleep without warning. Studies show opioid-induced respiratory depression happens most often in the first 24 hours after surgery-and patients with lung or heart disease are at highest risk. People taking high doses of either drug are more likely to crash. But even low doses can be dangerous together. One study found that patients given both opioids and benzodiazepines had 10 times higher risk of overdose death than those on opioids alone. While similar large-scale numbers for antihistamines are harder to find, the pharmacology is identical. The risk isn’t theoretical-it’s proven in emergency rooms and ICUs.Why Doctors Miss This
Many prescribers focus on the big-name drugs: opioids, benzodiazepines, alcohol. Antihistamines? They’re seen as harmless. But that’s the problem. Over-the-counter meds are easy to get. You don’t need a prescription. You don’t need to tell your doctor. But that doesn’t mean they’re safe with opioids. A 2021 NIH survey found that 68% of patients don’t mention OTC drugs to their doctors. That means if you’re on oxycodone and take Benadryl for allergies, your doctor might have no idea. Even when they do know, many providers still prescribe both. Why? Because they don’t realize how strong the interaction is. Or they assume the patient will “just take a little.” But a single 25mg dose of diphenhydramine can double the sedation effect of an opioid. And since there’s no antidote for antihistamine overdose-unlike naloxone for opioids-there’s no quick fix if things go wrong.
What You Can Do
If you’re on an opioid, here’s what you need to know:- Stop taking first-generation antihistamines. That includes Benadryl, Unisom, Atarax, and any generic version labeled “PM” or “for sleep.”
- Switch to second-generation antihistamines. Fexofenadine (Allegra), loratadine (Claritin), and cetirizine (Zyrtec) have minimal brain penetration. They treat allergies without making you sleepy. Fexofenadine, in particular, causes almost no sedation-even at full doses.
- Check every medication label. Many cold and flu pills, sleep aids, and motion sickness remedies contain diphenhydramine or doxylamine. They’re hidden in plain sight.
- Tell your doctor and pharmacist about every pill you take. Even if you think it’s “just an allergy pill.”
What Healthcare Providers Should Do
Hospitals and clinics are starting to catch on. Epic Systems, the largest electronic health record vendor in the U.S., now has “hard stop” alerts in 92% of hospitals using their system when opioids are prescribed with known CNS depressants. But not all systems are updated. And many still don’t flag OTC drugs. The CDC’s 2022 opioid prescribing guidelines say: “Avoid prescribing opioids and other CNS depressants concurrently whenever possible.” That includes antihistamines. Best practice? Screen every patient on opioids for OTC use. Ask directly: “Do you take anything for allergies, sleep, or colds?” Don’t assume they’ll volunteer it. Offer safer alternatives. Switch to non-sedating antihistamines. Use non-drug options like saline sprays or humidifiers for congestion. And if you’re managing pain in an elderly patient with COPD? Avoid antihistamines entirely. Use acetaminophen or NSAIDs if appropriate. Consider non-pharmacological options like physical therapy or nerve blocks.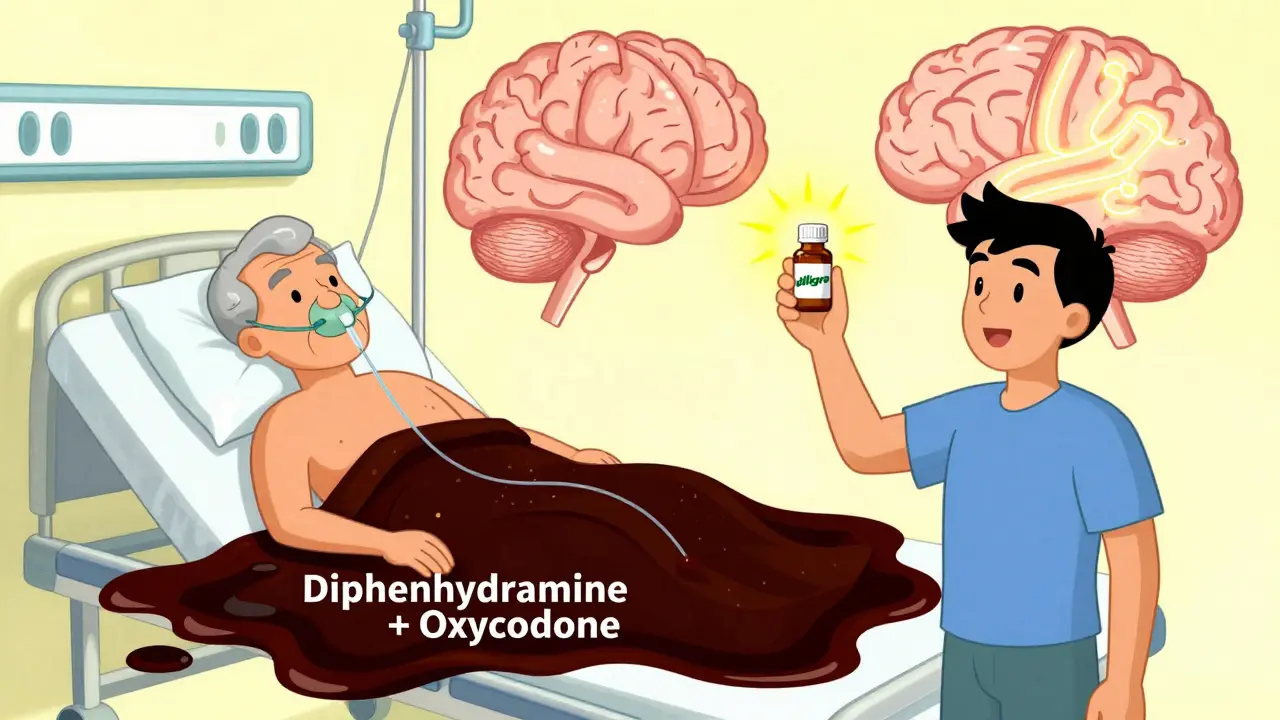
The Bigger Picture
This isn’t just about two drugs. It’s about how we treat pain, allergies, and sleep as separate problems-without looking at the whole person. In 2021, over 107,000 people in the U.S. died from drug overdoses. Synthetic opioids like fentanyl were involved in 80% of those deaths. But many of those deaths weren’t from heroin or street drugs-they were from prescriptions mixed with OTC meds. The FDA is now updating its opioid REMS program to require all 1.4 million prescribers in the U.S. to get trained on all CNS depressant interactions-not just benzodiazepines. That’s a step forward. But real change needs to start with patients. If you’re on an opioid, your life could depend on knowing this one thing: Don’t mix it with any sleep aid, allergy pill, or cold medicine unless your doctor says it’s safe.What to Do If You’ve Already Taken Them Together
If you’ve accidentally taken an opioid and an antihistamine together and feel extremely drowsy, confused, or have slow or shallow breathing:- Call 999 immediately.
- Don’t wait to see if it gets better.
- If someone else is with you, have them stay with you and monitor your breathing.
- If you have naloxone on hand, use it-but know it won’t reverse the antihistamine effect. It only helps with the opioid part.
Bottom Line
Opioids and antihistamines don’t just cause drowsiness. They can stop your breathing. Forever. And it doesn’t take much. One extra pill. One forgotten label. One assumption that “it’s just an allergy med.” The safest choice? Avoid the combo entirely. Switch to non-sedating allergy meds. Talk to your doctor. Read every label. And never assume something is safe just because it’s sold over the counter. Your life isn’t worth the risk.Can I take Benadryl with my opioid painkiller?
No. Taking Benadryl (diphenhydramine) with an opioid like oxycodone or hydrocodone can cause extreme drowsiness, slowed breathing, coma, or death. Both drugs depress the central nervous system, and together they greatly increase the risk of fatal respiratory depression. Even one dose can be dangerous, especially in older adults or people with lung disease.
Are all antihistamines dangerous with opioids?
No. Only first-generation antihistamines like diphenhydramine, hydroxyzine, and doxylamine are risky because they enter the brain and cause sedation. Second-generation antihistamines like fexofenadine (Allegra), loratadine (Claritin), and cetirizine (Zyrtec) have very little brain penetration and are generally safe to use with opioids. Always check the active ingredient on the label.
Why don’t doctors warn patients about this?
Many doctors focus on major drug interactions like opioids with benzodiazepines or alcohol, and overlook over-the-counter meds. Patients also rarely mention taking antihistamines, assuming they’re harmless. A 2021 NIH survey found 68% of patients don’t tell their doctors about OTC drug use. This gap in communication puts people at risk.
What should I use instead of Benadryl for allergies if I’m on opioids?
Switch to a non-sedating antihistamine like fexofenadine (Allegra), loratadine (Claritin), or cetirizine (Zyrtec). These work just as well for allergies but don’t cross into the brain, so they won’t increase sedation or breathing risks. Always confirm with your pharmacist or doctor before switching.
Can naloxone reverse an overdose from this combination?
Naloxone can reverse the opioid part of the overdose, but it does nothing to counteract the antihistamine’s effects. If someone overdoses from mixing opioids and antihistamines, naloxone might help a little-but they still need emergency medical care. The antihistamine will continue to suppress breathing. Never rely on naloxone alone in this situation.
Is this risk only for people with chronic pain?
No. Anyone taking opioids-even for a few days after surgery-can be at risk. In fact, opioid-induced respiratory depression is most common in the first 24 hours after surgery. Elderly patients, those with sleep apnea, or lung disease are especially vulnerable, but even healthy young adults have died from this combination.
How common are deaths from this interaction?
Exact numbers are hard to track because antihistamines are often unreported. But the Institute for Safe Medication Practices received 87 reports of serious adverse events involving opioids and sedating antihistamines between 2019 and 2022, with 12 resulting in death. Studies show similar risks to opioid-benzodiazepine combinations, which are known to increase overdose risk by 10 times. Experts agree this is an underrecognized cause of preventable death.






My grandma took Benadryl with her oxycodone for years and never had a problem. She’s 82, sleeps like a baby, and still knits sweaters. Maybe it’s not as dangerous as they make it sound? I’ve seen people panic over everything these days.
Oh here we go again with the fearmongering. You think people are stupid? Of course they know mixing drugs is risky. But you wanna know what’s really dangerous? The medical industrial complex turning every OTC pill into a death sentence so they can sell you pricier ‘safe’ alternatives. Benadryl’s been around since 1946. People lived. They slept. They didn’t die. Now we got a whole industry profiting off your paranoia.
Stop treating adults like toddlers who can’t read labels. If you’re taking opioids and diphenhydramine without knowing the risks, maybe you shouldn’t be trusted with a toaster.
And don’t get me started on ‘second-gen antihistamines’-they’re just corporate rebrands with the same active ingredients, just with less drowsiness so you can keep working while your body’s slowly shutting down. Wake up.
It’s not the drugs. It’s the narrative. The fear. The way we’ve turned medicine into a moral test. You take the wrong combo? You’re a liability. You die? You deserved it. That’s not medicine. That’s punishment dressed in white coats.
Real safety isn’t about banning things. It’s about empowering people with truth-not fear.
wait so zyrtec is safe with opioids? i’ve been taking it with my tramadol for months and never thought twice… should i be worried?
Yes, Zyrtec (cetirizine) is generally safe with opioids-minimal brain penetration, so it doesn’t add to respiratory depression. But if you’re elderly or have COPD, even Zyrtec can cause mild sedation in some people. Still, way safer than Benadryl. Your doctor should’ve flagged this, but better late than never. Keep using Zyrtec, ditch anything with ‘PM’ or ‘diphenhydramine’ on the label.
Let’s deconstruct this like the ideological scaffolding it is. The post frames antihistamines as silent assassins, but the real villain is the neoliberal pharmacopoeia that commodifies sleep, allergies, and pain as discrete pathologies requiring discrete pharmaceutical solutions. We’ve been trained to believe that every physiological discomfort demands a molecular intervention-when what we really need is systemic recalibration.
The FDA’s ‘hard stop’ alerts? A performative gesture. A digital placebo. It doesn’t address the root: a healthcare system that incentivizes prescription volume over patient autonomy. You want to reduce overdose deaths? Stop prescribing opioids in the first place. Stop pathologizing normal human experiences like fatigue or seasonal rhinitis. Stop treating the body like a broken machine that needs constant firmware updates.
And let’s be real-most of these ‘case reports’ come from people who didn’t just take one Benadryl. They took ten. They mixed it with whiskey. They didn’t sleep for three days. Then they wonder why they woke up in the ICU. Blame the drug? Or blame the culture that normalizes polypharmacy as self-care?
This isn’t about pharmacology. It’s about epistemology. We’ve outsourced our bodily wisdom to algorithms and pamphlets. The real danger isn’t diphenhydramine. It’s the belief that someone else knows better than your own intuition.
As a healthcare administrator in a rural U.S. clinic, I see this every week. Elderly patients come in with 12 different bottles. Half are OTC. None are documented. We’ve started printing simple one-page handouts in plain language and handing them out with every opioid prescription. We also train our pharmacists to ask, ‘Do you take anything for sleep or allergies?’-not ‘Do you take Benadryl?’ because most don’t know the name. Simple changes. Big impact.
bro i took benadryl with my hydrocodone last week after my tooth extraction and i just passed out on the couch for 5 hours. woke up with my dog licking my face and my wife screaming. i thought i was dead. never again. also my head felt like it was stuffed with wet cotton. worst. sleep. ever.
Knowledge is power. Read the label. Ask your pharmacist. Don’t gamble with your breath. This isn’t hype-it’s survival. If you’re on opioids, treat every sleep aid like a loaded gun. Because it is.
Y’all are acting like the government’s about to ban Benadryl. This is America. You want to mix opioids and antihistamines? Go ahead. But don’t cry when you get your name on the obituary. Freedom means taking stupid risks. And if you die? At least you died on your own terms. Not some CDC-managed, algorithm-approved life.