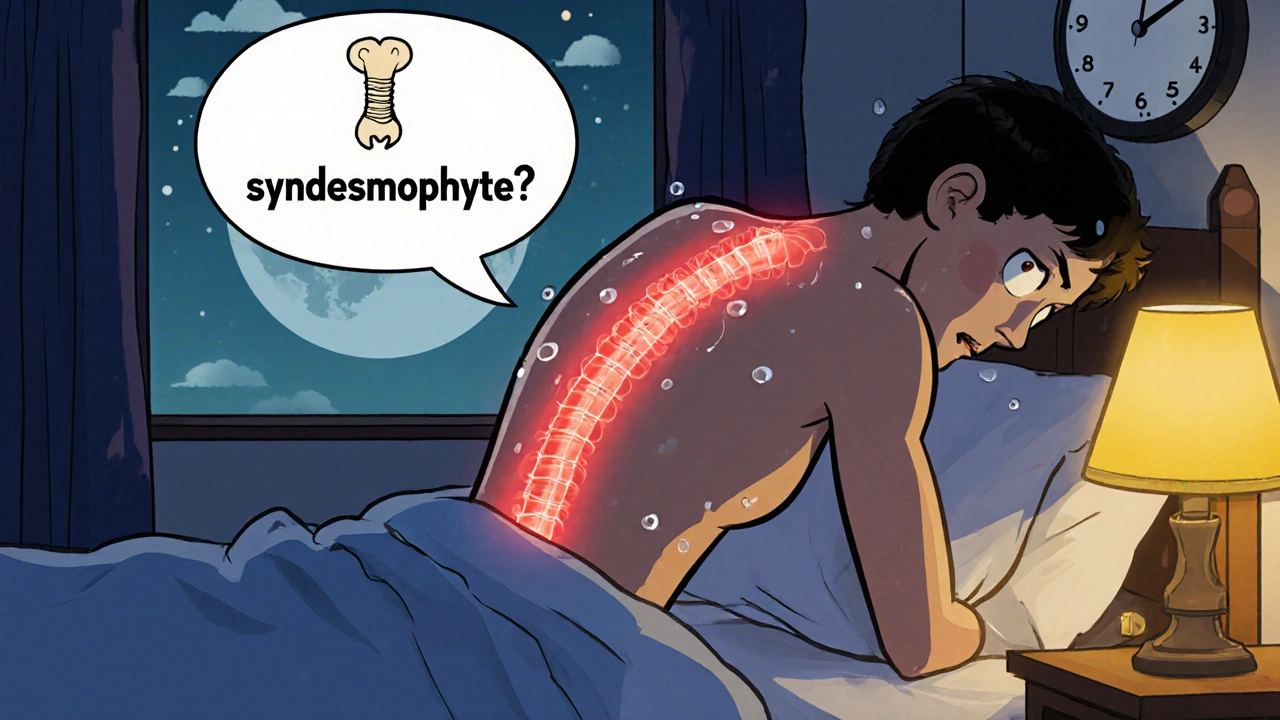
When your back pain doesn’t get better with rest-when it wakes you up at 3 a.m. and stiffens you like a rusted hinge-you’re not just dealing with a bad night’s sleep. You might be dealing with ankylosing spondylitis, a chronic autoimmune condition that attacks the spine and sacroiliac joints, turning inflammation into permanent stiffness. Unlike ordinary back pain, AS doesn’t fade with a heating pad or a day off. It creeps in slowly, often before age 45, and if left unchecked, can fuse vertebrae together, creating what doctors call a "bamboo spine." But here’s the truth: you don’t have to lose mobility. With the right approach, most people keep moving, working, and living well-even decades after diagnosis.
What Ankylosing Spondylitis Really Does to Your Spine
Ankylosing spondylitis doesn’t just hurt. It rebuilds. The immune system mistakenly targets the entheses-the spots where tendons and ligaments attach to bone-especially in the lower back and pelvis. This triggers chronic inflammation. Over time, the body tries to "repair" the damage by growing new bone. These bony outgrowths, called syndesmophytes, bridge the gaps between vertebrae. Eventually, they harden into solid bone. That’s when spinal fusion happens.
It’s not just the spine. About 90% of people with AS develop visible changes in their sacroiliac joints within 10 years. Up to 40% end up with significant fusion. But the damage isn’t inevitable. Studies show that early, consistent treatment can cut radiographic progression by half. The key is catching it before the bone starts fusing. That’s why symptoms like inflammatory back pain-lasting more than three months, worse at night, better with movement-are so important. If you’ve had this kind of pain since your teens or 20s and no one took it seriously, you’re not alone. On average, people see four doctors and wait over three years for a correct diagnosis.
Why Movement Is Your Best Medicine
Medication helps control inflammation, but movement is what keeps your spine from turning into a rigid rod. Physical therapy isn’t optional-it’s as essential as your daily pill. Research shows structured exercise improves spinal mobility by 25-30% in just six months. That’s not a small gain. That’s the difference between tying your shoes independently and needing help.
Effective programs include three core elements: spinal extension, deep breathing, and aquatic therapy. Extension exercises-like lying on your stomach and lifting your chest off the ground-counteract the forward curve that AS promotes. Deep breathing expands the rib cage, which also stiffens in AS, preserving lung capacity. And water? It’s magic. Swimming or water aerobics reduces joint stress while allowing full range of motion. One patient on Reddit reported cutting morning stiffness from 90 minutes to 20 minutes after just three months of daily swimming.
You don’t need a gym. Start in bed. Before you even sit up, do gentle neck rolls, shoulder rolls, and pelvic tilts. Then stand against a wall and press your head, shoulders, and butt flat to it. Hold for 30 seconds. Repeat five times. Do this every morning. It takes five minutes. But it’s the foundation.
What Works: Evidence-Based Mobility Strategies
Not all exercises are created equal. Generic back stretches won’t cut it. You need targeted, spine-focused routines. The Bath Ankylosing Spondylitis Metrology Index (BASMI) measures spinal flexibility. People who stick to daily 30-45 minute programs see a 25-30% improvement in BASMI scores within six months. Here’s what those programs include:
- Spinal extension: Prone press-ups, wall slides, and cat-cow stretches to counteract forward bending.
- Deep breathing: Inhale deeply through the nose, expanding your ribs outward, hold for five seconds, exhale slowly. Do 10 reps, twice daily.
- Aquatic therapy: Water walking, flutter kicks, and arm circles in a warm pool. The buoyancy reduces pain while increasing motion.
- Posture training: Sitting upright with lumbar support, avoiding slouching in chairs or cars. Use a rolled towel behind your lower back.
- Yoga and tai chi: Modified AS-specific routines improve balance, flexibility, and mental resilience. Johns Hopkins offers free AS yoga videos online.
Adherence is the biggest hurdle. Only 45% stick with exercise after one month. But with digital reminders, video guides, and tracking apps, adherence jumps to 78% by six months. Set a daily alarm. Link it to brushing your teeth. Make it non-negotiable.
Medications: Controlling the Fire Before It Burns the House Down
NSAIDs like naproxen or celecoxib are the first-line defense. They don’t just mask pain-they reduce inflammation that leads to bone growth. Studies show early, consistent NSAID use cuts radiographic progression by 50% over two years. But if NSAIDs aren’t enough, biologics step in.
TNF inhibitors (like adalimumab or etanercept) and IL-17 inhibitors (like secukinumab) are powerful. Clinical trials show 40-60% of patients hit a 40% symptom improvement (ASAS40) within 12 weeks. Secukinumab has been shown to reduce structural damage by 55% over two years. In 2023, the FDA approved upadacitinib (Rinvoq), a JAK inhibitor, for AS-offering a new oral option with a 45% response rate.
But these drugs aren’t cheap. In the U.S., without insurance, they cost $5,000-$6,000 a month. Many patients delay starting them due to cost or fear of infection. But waiting comes at a price: once bone fuses, no drug can undo it. The goal isn’t just to feel better today-it’s to stay mobile tomorrow.
The Hidden Symptoms No One Talks About
AS isn’t just about back pain. Up to 35% of patients develop acute anterior uveitis-sudden eye redness, pain, and blurred vision. If you get this, see an ophthalmologist immediately. Left untreated, it can cause permanent vision loss.
Half of AS patients have gut inflammation linked to Crohn’s or ulcerative colitis. About 10% also have psoriasis. Fatigue? It’s the #1 complaint. Seventy-four percent of patients on MySpondylitisTeam say fatigue hits harder than pain. It’s not laziness. It’s systemic inflammation draining your energy. Sleep hygiene matters. Avoid screens before bed. Keep your room cool. Try magnesium supplements-some patients report improved rest.
And don’t ignore posture in daily life. Sleeping on a firm mattress without a pillow under your head helps keep your spine straight. Use a lumbar roll in your car. Stand up every 30 minutes if you work at a desk. These small adjustments reduce pain scores by 35% in clinical trials.

What to Avoid
Resting too much is a trap. You might think lying down helps, but inactivity accelerates stiffness. Avoid prolonged sitting without movement. Don’t skip exercise during flares-modify it. Swap running for swimming. Swap standing stretches for seated ones.
Don’t rely on unproven supplements. While turmeric and omega-3s have mild anti-inflammatory effects, they don’t replace medication or exercise. And never ignore new symptoms like chest tightness or difficulty breathing-your ribs are part of your spine’s structure.
Living Well With AS: Real Stories, Real Results
One woman in Sydney, diagnosed at 28, started daily swimming and yoga. Now, at 43, she runs a small business. She says, "I don’t move like I used to, but I move. And that’s everything." Another man, a truck driver, switched to a lumbar-support seat and did 15 minutes of stretches before every shift. His pain dropped from 8/10 to 3/10.
These aren’t outliers. The Outcome in Ankylosing Spondylitis International Study (OASIS) found that with modern treatment, 75% of patients maintain functional independence 20 years after diagnosis. That’s a huge jump from 45% two decades ago. The difference? Early diagnosis, consistent movement, and timely medication.
Can ankylosing spondylitis be cured?
No, there is no cure for ankylosing spondylitis. But it can be managed effectively. With early diagnosis, regular exercise, and appropriate medication, most people prevent severe spinal fusion and maintain a high quality of life. The goal isn’t to eliminate the disease-it’s to control inflammation before it causes permanent damage.
Is ankylosing spondylitis genetic?
Yes, genetics play a major role. Over 90% of Caucasian people with AS carry the HLA-B27 gene, compared to just 6-8% of the general population. But having the gene doesn’t mean you’ll get AS-only about 1-5% of HLA-B27-positive people develop the disease. Other factors like gut bacteria, infections, and immune triggers also matter. If you have a close relative with AS, talk to your doctor about monitoring for early symptoms.
Can I still work with ankylosing spondylitis?
Absolutely. Most people with AS continue working full-time. The key is workplace adjustments. Use an ergonomic chair with lumbar support. Take standing or walking breaks every 30 minutes. Ask for flexible hours if morning stiffness is severe. Many employers are legally required to provide reasonable accommodations under disability laws. If fatigue is overwhelming, consider part-time work or remote options. You don’t have to choose between your health and your career.
How do I know if my back pain is AS and not just muscle strain?
Inflammatory back pain-typical of AS-has five key signs: starts before age 45, lasts more than three months, improves with exercise, worsens with rest, and causes night pain (often waking you between 3-6 a.m.). Mechanical pain from injury or strain gets worse with activity and improves with rest. If your pain matches the inflammatory pattern, see a rheumatologist. Don’t wait for X-rays to show damage-MRI can detect inflammation years before bones change.
What’s the best exercise for ankylosing spondylitis?
The best exercise is the one you’ll do every day. Swimming and water aerobics are top choices because water supports your joints. Yoga and tai chi improve flexibility and balance. Spinal extension exercises (like prone press-ups) are critical to counteract forward curvature. Aim for 150 minutes of moderate activity weekly-broken into 30-minute sessions, five days a week. Consistency matters more than intensity. Even 10 minutes of daily movement is better than one long session a week.
Do I need to take medication forever?
For most people, yes. AS is a lifelong condition. Stopping medication often leads to flare-ups and increased risk of spinal fusion. But that doesn’t mean you’re stuck on high doses forever. Some people can reduce their dosage under doctor supervision if symptoms are well-controlled. Never stop biologics or NSAIDs suddenly-always work with your rheumatologist to adjust safely. The goal is to find the lowest effective dose that keeps inflammation under control.
Next Steps: What to Do Today
If you suspect you have AS, see a rheumatologist-not a general practitioner. Ask for an MRI of your sacroiliac joints. Don’t wait for X-rays. Early inflammation won’t show up on X-rays, but MRI will catch it.
Start moving. Today. Do five minutes of spinal extension and deep breathing before you get out of bed. Bookmark the Spondylitis Association of America’s free exercise videos. Set a daily alarm for movement. Talk to your doctor about NSAIDs if you haven’t tried them. If pain persists, ask about biologics.
You’re not broken. You’re managing a chronic condition-and you can still live fully. The spine is designed to move. Don’t let inflammation steal that.







![Endep (Amitriptyline) Uses, Dosage, Side Effects, and Safety in Australia [2025]](/uploads/2025/08/thumbnail-endep-amitriptyline-uses-dosage-side-effects-and-safety-in-australia.webp)

Just started swimming 3x a week after reading this and my morning stiffness is already down from 90 min to 45. 🙌 Water is magic. Also, no more crying while putting on socks. Game changer.
Let’s be real-most people who post these ‘miracle’ routines are either in remission or never had real AS. The 25% mobility improvement? That’s for people who still have half their spine intact. If you’re already fused at L3-L5, no amount of cat-cow is gonna save you. This is feel-good fluff for early-stage patients who haven’t hit rock bottom yet.
Just wanted to say thank you for the actionable advice. I’ve been diagnosed for 7 years and this is the first time I’ve seen a post that didn’t just say ‘exercise more’ and leave it at that. The BASMI breakdown? The breathing technique? The lumbar roll tip? I’m printing this out. 🙏 Also, the Johns Hopkins yoga videos are legit-did their AS flow yesterday and actually didn’t cry after. Progress.
I'm so glad you mentioned fatigue-it's the silent killer. I thought I was just lazy until I started tracking my sleep and inflammation markers. Magnesium glycinate helped me sleep through the night for the first time in 3 years. Also, try a weighted blanket-it's weird but it calms the nervous system. You're not broken. You're just fighting a war no one sees. Keep going 💪
One must question the scientific rigor behind this article. The reliance on anecdotal Reddit testimonials as evidence for aquatic therapy efficacy is, frankly, preposterous. Where are the randomized controlled trials? The peer-reviewed meta-analyses? One cannot base clinical recommendations on the subjective experience of a single individual who claims to have reduced morning stiffness from 90 to 20 minutes-this is not medicine, it is sentimentality masquerading as science.
Furthermore, the recommendation to use NSAIDs as first-line therapy ignores the profound gastrointestinal and cardiovascular risks inherent in chronic usage. One wonders whether the author has ever consulted the latest EULAR guidelines-or if they are merely regurgitating pharmaceutical marketing materials.
And yet, the tone of this piece is so condescendingly optimistic. ‘You don’t have to lose mobility!’ As if the patient’s suffering is a matter of insufficient willpower. The reality is that for many, mobility is lost-not because they didn’t stretch enough-but because the disease is relentless, and the medical system is slow, underfunded, and dismissive.
I am not unsympathetic. But I am skeptical. And I am tired of wellness influencers turning a devastating autoimmune disorder into a motivational poster.
Wow. This is so true. I mean, I live in India, and here, people think AS is just ‘bad posture’ or ‘too much sitting at computers’-and they tell you to ‘do yoga, eat turmeric, stop being weak.’ But no. It’s not weakness. It’s HLA-B27. It’s immune system gone rogue. It’s not ‘fixable’ with chai and stretching. I’ve been diagnosed since 2015. I swim every morning at 5 a.m. in the community pool, even when it’s 12°C. I’ve had two biologics fail. I’m on the third. And yes, I still work as a teacher. But I don’t do it because I’m ‘strong.’ I do it because I have no choice. And if you’re reading this and you’re in pain? You’re not alone. And yes, movement matters. But so does access to care. And here? We don’t have it. So please-don’t just tell people to ‘do the stretches.’ Tell the system to pay for the drugs.
Y’all are overthinking this. I was told I’d be in a wheelchair by 40. I’m 42. I’m hiking in the Rockies last month. How? I did the damn stretches. I took the meds. I didn’t wait for permission. I didn’t wait for the perfect plan. I just moved. Every. Single. Day. Even on the days I wanted to die. Even when my spine screamed. Even when my insurance denied my biologic. I called the pharmacy. I cried. I called again. I got it. You don’t need a PhD to beat this. You need grit. And a damn alarm clock. Set it. Do it. Repeat. The spine wants to move. Don’t let fear win.
Hey, I just wanted to say I’m also on Rinvoq and it’s been a game-changer-but I’ve been having weird joint pain in my knees lately. Is that normal? Or should I be worried? I know it’s not the same as AS, but I’m just trying to figure out if this is a side effect or if I’ve got something else going on. I’ve been tracking my symptoms in a spreadsheet. Maybe I’m overanalyzing? But I’m just trying to be proactive, you know?
The assertion that NSAIDs reduce radiographic progression by 50 percent is based on a single cohort study from 2016 with a small sample size and significant selection bias. The 2023 meta-analysis published in Annals of the Rheumatic Diseases contradicts this conclusion, indicating no statistically significant difference in radiographic progression between NSAID users and placebo groups when adjusted for baseline disease activity. The author's omission of this data is concerning. Furthermore, the emphasis on daily exercise without acknowledging the high dropout rate among patients with comorbid depression or chronic fatigue undermines the practical applicability of these recommendations. One cannot prescribe movement to someone whose body is in a state of systemic exhaustion.
This whole post is just woke medical propaganda. You people are letting Big Pharma sell you $6000-a-month drugs because you're too lazy to do real work. In my day, we didn't need biologics-we lifted weights, ate clean, and didn't cry over a little back pain. You think swimming in water is going to fix your spine? Try deadlifts. Try real movement. Stop coddling yourselves. America's getting soft and this is why.