Antibiotic-Warfarin Interaction Checker
Find out how your antibiotic affects warfarin
This tool shows the interaction risk, expected INR impact, and recommended monitoring schedule for different antibiotics when used with warfarin.
When you’re on warfarin a vitamin K antagonist used to prevent clots, adding an antibiotic can feel like stepping into a minefield. A sudden jump in your INR (International Normalized Ratio) may turn routine bruises into serious bleeds, and many patients aren’t sure how to stay safe. This guide walks you through why the interaction happens, which antibiotics are the biggest culprits, and what you can do to keep your blood in the right range.
Why antibiotics mess with warfarin
Two main mechanisms drive the clash:
- Gut‑flora disruption: Certain antibiotics wipe out vitamin K‑producing bacteria (like Bacteroides and Eubacterium). Since those microbes supply 10‑15% of the body’s vitamin K, their loss can raise INR within a week of starting the drug.
- CYP450 inhibition: Warfarin’s more potent S‑isomer is cleared mainly by CYP2C9. Antibiotics that block this enzyme (fluoroquinolones, macrolides, sulfamethoxazole/trimethoprim) cause warfarin levels to climb 30‑50% in just 48‑72 hours.
Because both pathways can act together, the INR may sky‑rocket faster than you expect.
High‑risk antibiotic classes
Not every antibiotic is equally risky. Here’s a quick look at the classes that regularly push INR over the safe limit.
| Antibiotic Class | Key Examples | Interaction Mechanism | Mean INR Rise |
|---|---|---|---|
| Fluoroquinolones | Ciprofloxacin, Levofloxacin | Strong CYP2C9 inhibition | +1.6 to +2.5 units |
| Macrolides | Erythromycin, Azithromycin | CYP3A4 (erythro) / minimal (azithro) | +0.8 to +1.4 units |
| Sulfamethoxazole/Trimethoprim | Bactrim | CYP2C9 inhibition + gut flora loss | +1.8 units |
| Cephalosporins (with N‑MTT side chain) | Cefotetan, Cefoperazone | Gut‑flora disruption | +1.5 to +2.2 units |
| Penicillin combos | Amoxicillin/Clavulanate | Gut‑flora disruption | +1.0 to +1.3 units |
| Rifampin | Rifampin | CYP induction (CYP2C9, CYP3A4) | -1.0 to -1.8 units (risk of under‑anticoagulation) |
Antibiotics like nitrofurantoin and fosfomycin have shown negligible effects on INR and usually don’t need extra checks.
When does the INR usually jump?
Timing matters. CYP inhibition shows up fast-often within 48-72 hours-while vitamin K depletion takes 5-7 days to reflect in the INR. The peak bleeding risk, according to the 2012 Medicare study, occurs between days 8‑14 of antibiotic therapy. After the antibiotic stops, CYP effects fade in about three days, but gut‑flora recovery can linger another week.
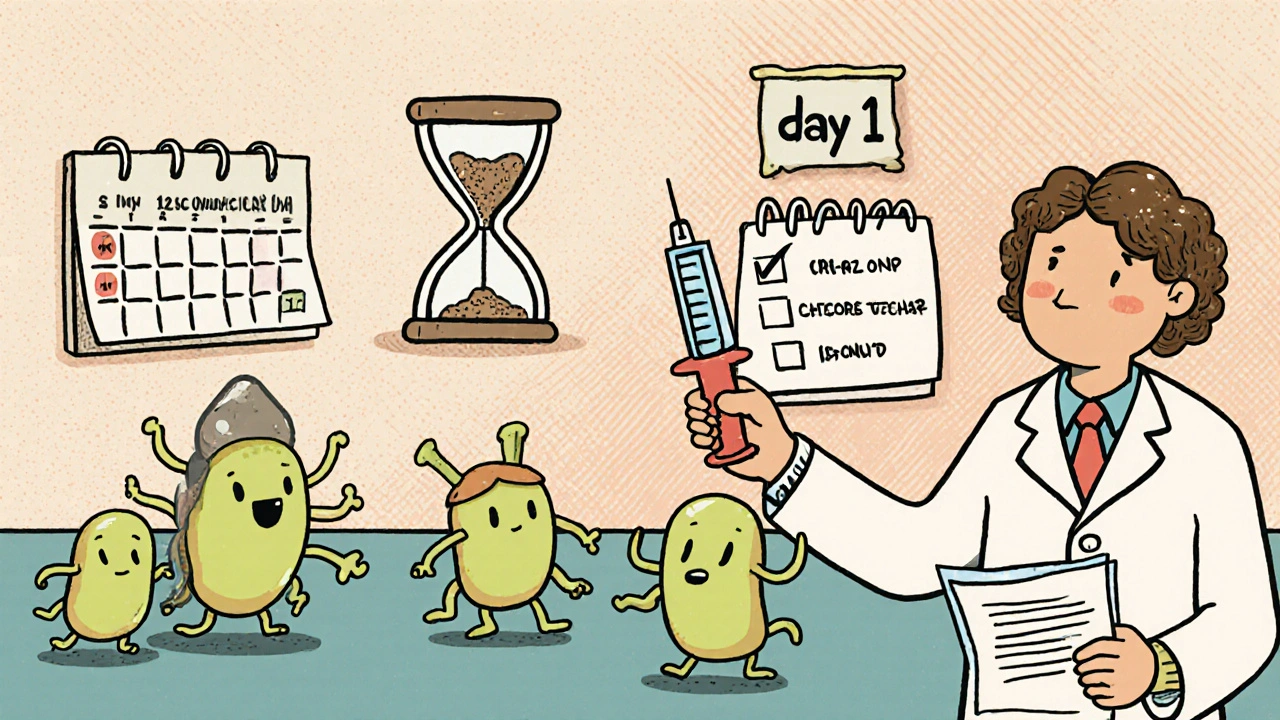
Practical monitoring plan
Here’s a step‑by‑step checklist you can share with your clinician or anticoagulation clinic:
- Identify the antibiotic class before the prescription is filled.
- Schedule an INR test within 72 hours of starting a high‑risk antibiotic (fluoroquinolone, macrolide, Bactrim).
- Repeat INR every 2‑3 days while the antibiotic is active.
- If INR climbs above the target range (2.0‑3.0 for most patients, 2.5‑3.5 for high‑risk conditions), consider a 20‑30% warfarin dose reduction.
- For gut‑flora disruptors (cephalosporins, amoxicillin/clavulanate), weekly checks are usually enough unless the INR jumps.
- Test again within 72 hours after stopping the antibiotic to catch any rebound.
- Educate yourself on bleeding signs: unusual bruising, pink‑tailed urine, prolonged bleeding from cuts, or blood in stool. Call your clinic immediately if you notice them.
Pharmacist‑managed warfarin programs have shown a 37% drop in bleeding events when they follow this exact schedule.
Adjusting warfarin dose during co‑therapy
Guidelines from the UC‑San Diego Anticoagulation Clinic split recommendations by interaction type:
- CYP inhibitors (fluoroquinolones, macrolides, Bactrim): reduce warfarin dose by 20‑30% at the start.
- Gut‑flora disruptors (cephalosporins, amoxicillin/clavulanate): hold dose adjustments unless INR exceeds the goal.
- CYP inducers (rifampin): increase warfarin dose by ~50% and monitor daily until stable.
These are starting points. Your exact reduction may differ based on age, liver function, and genetic factors (CYP2C9*2/*3 variants can amplify the INR rise by over two‑fold).
What to do if INR spikes
Don’t panic, but act fast:
- If INR is 4.0‑5.0 and you have no bleeding, hold the next warfarin dose and repeat INR in 24 hours.
- If INR > 5.0 or you notice bleeding, contact your anticoagulation clinic. They may give a low‑dose vitamin K oral tablet (2.5-5 mg) and/or pause warfarin until INR drops below 3.0.
- For major bleeding (intracranial, gastrointestinal), emergency care and prothrombin complex concentrate (PCC) are required.
Document every INR result in a notebook or app. Having a clear timeline helps clinicians spot patterns and adjust doses more accurately.
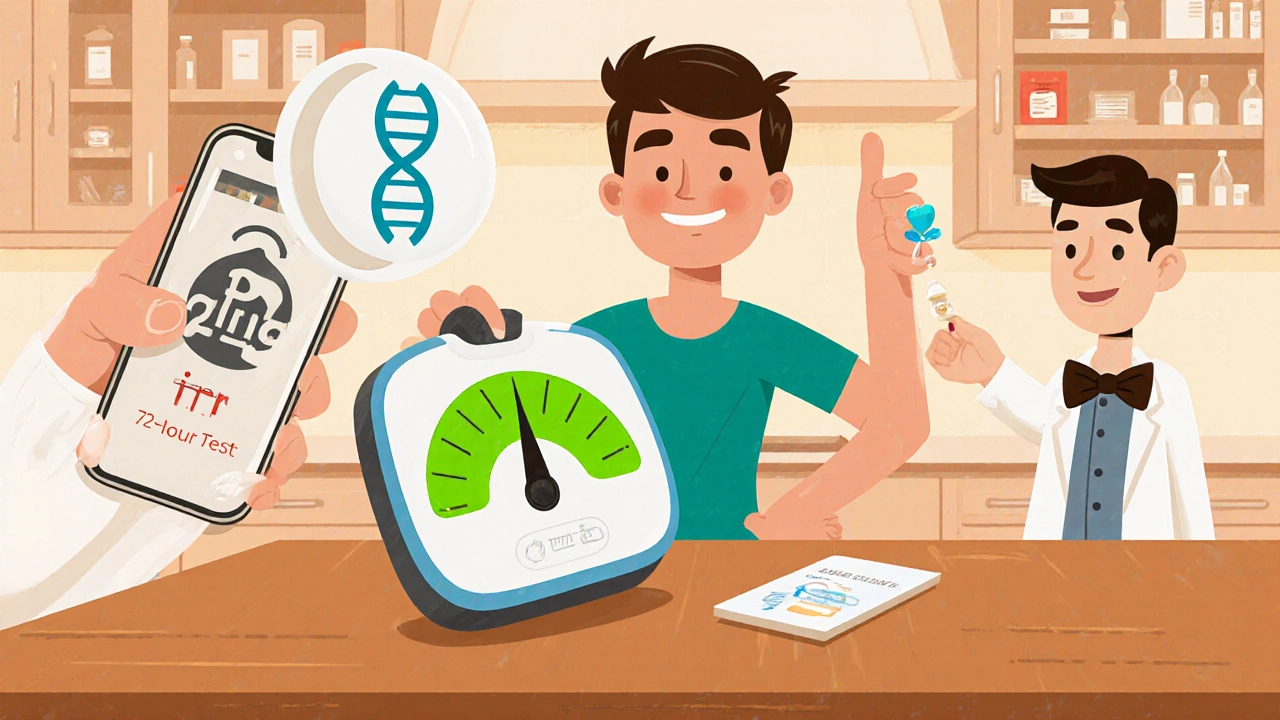
Technology tricks that help
Electronic health record alerts can shave off ~22% of adverse events, but they work best when paired with a dedicated anticoagulation pharmacist. Mobile apps that pull your latest INR from the clinic and cross‑reference prescribed antibiotics also cut confusion. If you use a home INR monitor, sync the device with your phone and set reminders for the 72‑hour checks.
Future directions - genetics and AI
Research is moving toward pre‑emptive genotyping. A 2022 pharmacogenomics study showed patients with CYP2C9*2/*3 variants faced 2.4‑fold higher INR spikes when on fluoroquinolones. The ongoing WARF‑GEN trial uses that data to feed an AI dosing algorithm, cutting instability by 41%. While routine genetic testing isn’t standard yet, if you have a family history of unusual warfarin responses, ask your doctor about a CYP2C9 test. It could spare you a risky dose adjustment later.
Quick reference cheat‑sheet
| Antibiotic Type | Initial Dose Change | First INR Check | Follow‑up Frequency |
|---|---|---|---|
| CYP Inhibitors (e.g., ciprofloxacin) | -20‑30% | within 72 h | every 2‑3 days |
| Gut‑Flora Disruptors (e.g., cefotetan) | none unless INR > goal | within 72 h | weekly |
| CYP Inducers (e.g., rifampin) | +50% | daily | daily until stable |
Keep this table on your phone or printed out at the kitchen counter-quick look‑ups win the day.
How quickly can an antibiotic raise my INR?
CYP‑blocking antibiotics can push INR up in 48‑72 hours, while those that suppress gut‑flora usually need 5‑7 days to show a rise.
Do all antibiotics require dose changes for warfarin?
No. Nitrofurantoin, fosfomycin, and many newer agents like tedizolid have minimal impact and generally don’t need a pre‑emptive dose tweak.
What bleeding signs should I watch for?
Look for unexplained bruises, blood in urine or stool, nosebleeds that last longer than a few minutes, or bleeding that won’t stop after a minor cut.
Can vitamin K tablets reverse a high INR safely?
For INR values between 4.0‑5.0 without bleeding, a low‑dose oral vitamin K (2.5‑5 mg) can bring the ratio back into range without causing clotting.
Is genetic testing worth it before starting antibiotics?
If you’ve had unpredictable warfarin responses or a family history of extreme INR swings, a CYP2C9 test can guide safer dose adjustments during antibiotic courses.








The pharmacokinetic synergy between ciprofloxacin and warfarin exemplifies a paradox where inhibition of CYP2C9 amplifies anticoagulant potency thereby demanding preemptive dose recalibration. Clinical stewardship must incorporate both enzymatic and microbiome considerations to mitigate hemorrhagic sequelae.
Thanks for sharing this detailed guide. It’s a solid roadmap for anyone juggling antibiotics with warfarin, especially the clear timing suggestions for INR checks.
Great rundown! I’ve found that setting a reminder on my phone for the 72‑hour INR test saves me a lot of worry, and most of the time the dose tweak is minor.
I totally agree with the importance of timing, and I’d like to add a few personal observations that might help other readers. First, when I was prescribed levofloxacin for a sinus infection, my INR jumped from 2.4 to 3.9 within two days, which forced me to hold a dose of warfarin. Second, I kept a paper log of every INR result, the exact date I started the antibiotic, and any dose changes; this simple habit made communication with my anticoagulation clinic much smoother. Third, I discovered that taking a low‑dose vitamin K supplement (0.5 mg) on alternate days helped stabilize my INR without compromising the antibiotic’s effectiveness. Fourth, I always ask the pharmacist whether the antibiotic is a known CYP2C9 inhibitor before filling the prescription. Fifth, if the antibiotic is a gut‑flora disruptor like amoxicillin‑clavulanate, I schedule a weekly INR check instead of an every‑2‑day check, which saves both time and lab visits. Sixth, I’ve noticed that older patients tend to have a more pronounced INR rise, possibly due to reduced hepatic clearance, so extra vigilance is warranted. Seventh, the guideline to reduce warfarin dose by 20‑30% at the start of a CYP inhibitor is a good rule of thumb, but I sometimes start with a 10‑15% reduction and titrate based on the first INR result. Eighth, I use a mobile app that syncs with my clinic’s portal, automatically alerting me when the next INR draw is due. Ninth, when my INR exceeded 5.0, my provider gave me a single oral dose of 2.5 mg vitamin K, and the INR came back to target within 24 hours. Tenth, I have never needed prothrombin complex concentrate because I caught the spike early and acted accordingly. Eleventh, for antibiotics that are CYP inducers like rifampin, I coordinate a rapid dose increase of warfarin and close INR monitoring to avoid under‑anticoagulation. Twelfth, discussing the potential interaction with the prescribing physician upfront can sometimes result in choosing an alternative antibiotic with less impact on warfarin. Thirteenth, patients with known CYP2C9*2/*3 genotypes should be especially careful, as they are prone to larger INR excursions. Fourteenth, keeping a list of your current medications handy when you go to the pharmacy can prevent accidental co‑prescribing of high‑risk drugs. Fifteenth, never ignore minor bruising; it can be an early sign of an INR that’s climbing. Finally, share this cheat‑sheet with family members who help you manage your medication-they’ll appreciate the clear, actionable steps.
Wow, this post is like a masterclass in anti‑coagulation alchemy 🧪💉 – I love how you break down the enzyme vs. flora mechanisms and actually give us a step‑by‑step action plan. The tables are pure gold, and the emoji‑free warning signs are a nice touch. 🙌
Appreciate the thoroughness, especially the reminder to check INR within 72 hours of starting a high‑risk antibiotic. Keeping a digital log and setting alerts can really smooth the whole process.
Just read through the whole thing, and I must say, what a comprehensive overview, especially the way you laid out the timing of CYP inhibition versus gut‑flora changes, really helpful for patients, and the cheat‑sheet at the end, brilliant, I’ll definitely pin that, thanks!
Holy smokes – this guide reads like a thriller, the stakes are real! I noticed a tiny typo in the table ("Cefotetan" was spelled “Cefotetan,”) but otherwise it’s spot‑on. The dramatic break‑downs really drive the point home.
Let me add that the half‑life of warfarin’s S‑isomer is approximately 40 hours, so any CYP2C9 inhibition can have a prolonged effect even after the antibiotic is stopped. Also, the protein binding displacement by some macrolides can contribute subtly to INR elevations.
Good point about half‑life. I’d also suggest a quick phone check with the anticoagulation clinic after the first INR spike – they can fine‑tune the dose before the next lab draw.
Useful info.
Okay, so you’re basically telling us that an antibiotic can turn our carefully calibrated warfarin regimen into a ticking time‑bomb, which, frankly, feels like the medical version of “it’s not a bug, it’s a feature.” In other words, if you’re not already a pharmacology Jedi, you might want to keep a spreadsheet, a calendar reminder, and maybe a therapist on speed‑dial.
Great summary – I’ll share this with my older mom who’s on warfarin; the clear steps make it less intimidating for her.