Triptan Medication Interaction Checker
This tool helps you identify potential dangerous interactions between triptans and medications you're taking. Triptans can interact with certain drugs, especially antidepressants and vasoconstrictors, potentially causing serious health risks. Always consult your doctor before making changes to your medication regimen.
Triptans changed how we treat migraines. Before they existed, people relied on painkillers that barely touched the root of the problem. Now, with drugs like sumatriptan, rizatriptan, and zolmitriptan, many people get real relief-sometimes within an hour. But triptans aren’t magic pills. They come with serious rules, hidden risks, and limits most people never hear about until it’s too late.
How Triptans Actually Work
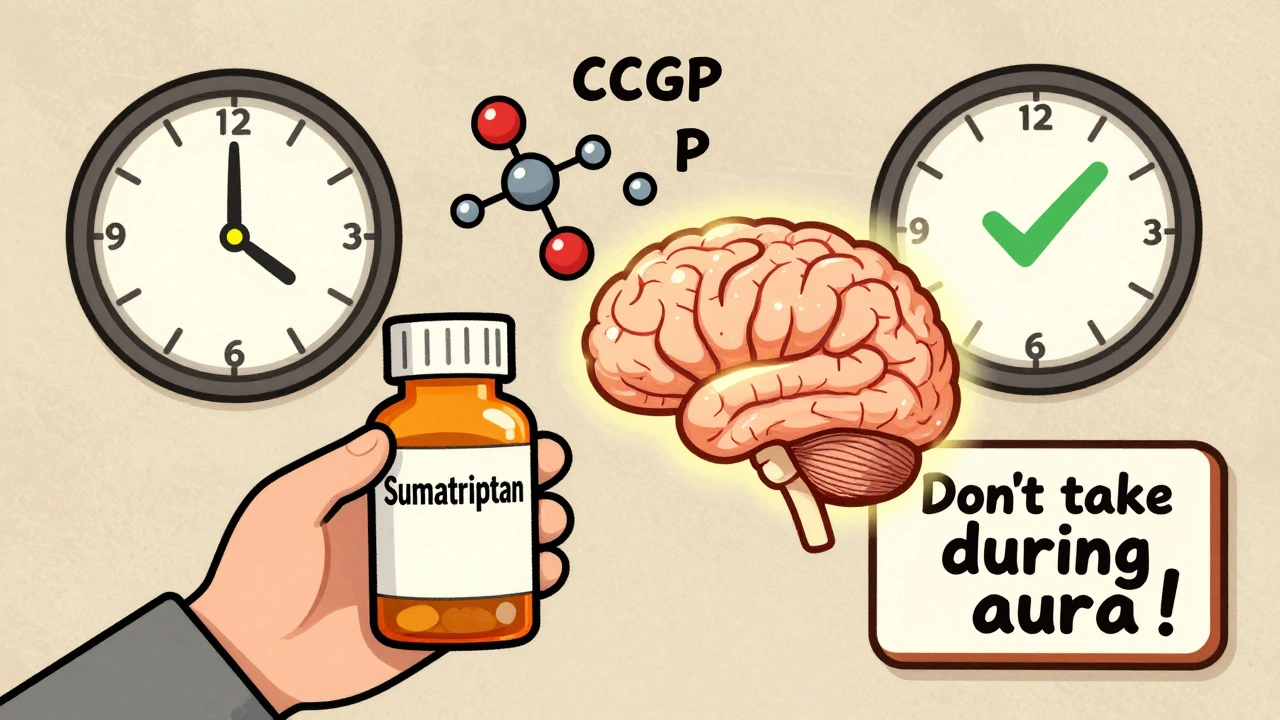
Triptans don’t just numb pain. They target the nerve pathways that spark migraine attacks. When a migraine hits, blood vessels in the brain swell and nerves release chemicals like CGRP and substance P. These trigger inflammation and pain. Triptans lock onto 5-HT1B and 5-HT1D receptors on those nerves and blood vessels. This causes the swollen vessels to shrink and stops the chemicals from flooding the system.
It’s not guesswork. Studies show sumatriptan lowers CGRP levels in the blood as the headache fades. That’s proof it’s working at the source. But here’s the catch: timing matters. If you take a triptan during the aura phase-before the headache starts-you might make things worse. Blood vessels are already constricted then. Adding a vasoconstrictor can trigger more neurological symptoms, not less.
Which Triptans Work Best-and Why
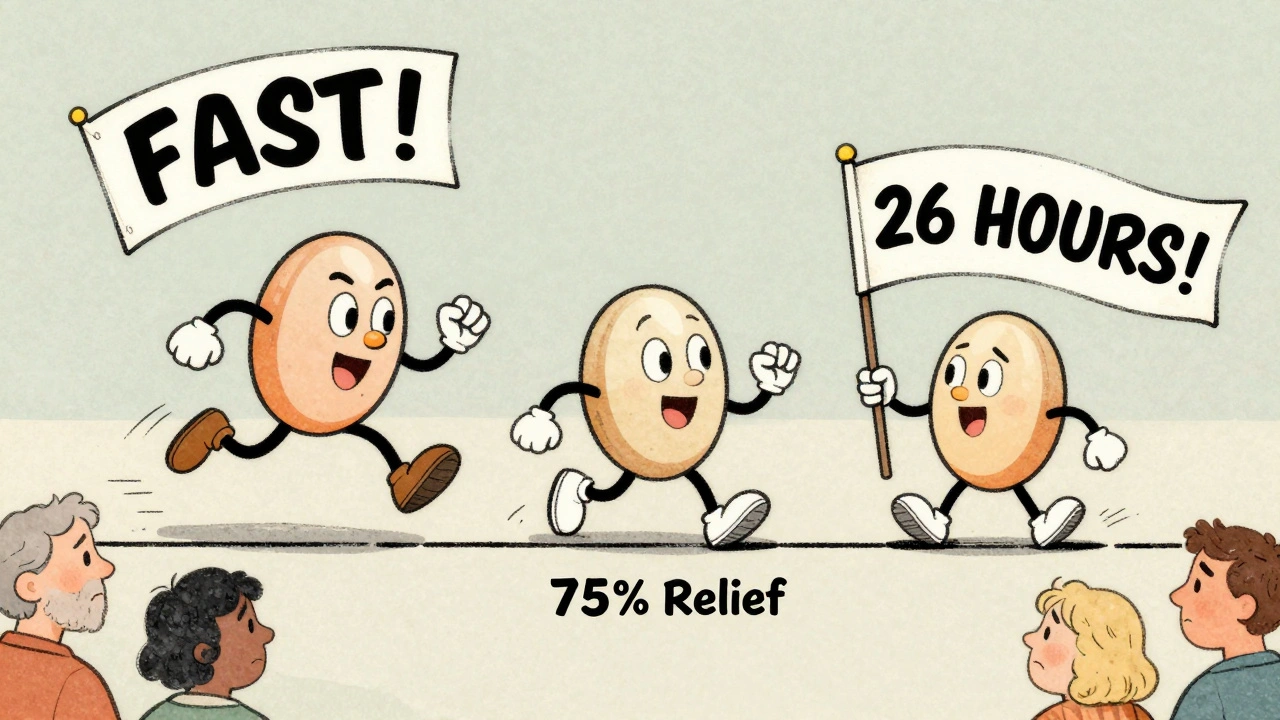
There are seven FDA-approved triptans. They all have the same goal, but they don’t work the same way. Rizatriptan hits fast: 10 mg gives relief in under an hour for many. Eletriptan has the highest success rate at two hours-75% of users report headache relief. But it doesn’t last long. Frovatriptan? It’s slow to start but lasts up to 26 hours. That’s why it’s often chosen for menstrual migraines.
Oral absorption varies too. Sumatriptan gets only 15% into your bloodstream. Rizatriptan? Nearly 45%. That’s why some people swear by rizatriptan orally disintegrating tablets-they work faster and more reliably than pills.
And effectiveness isn’t one-size-fits-all. About 30-40% of migraine sufferers don’t respond to a given triptan. But here’s the good news: if one fails, another might work. Around 30-40% of people who don’t respond to one triptan find relief with a different one. That’s because each has slightly different receptor preferences and how fast it moves through the body.
The Hidden Risks: What You’re Not Told
Triptans are safe for most people-but not everyone. If you have heart disease, a history of stroke, uncontrolled high blood pressure, or poor circulation, you should never take them. These drugs narrow blood vessels. In someone with clogged arteries, that can trigger a heart attack or stroke. The risk is small-about 0.08 cases per 10,000 users per year-but it’s real.
And it’s not just heart issues. People with severe liver problems can’t clear triptans properly. That means the drug builds up. Doses that are safe for others become dangerous.
Even if you’re healthy, side effects are common. About 5-7% feel chest or throat tightness-like someone’s squeezing their throat. It’s not a heart attack, but it’s scary. Dizziness and fatigue hit 4-10% of users. Most people push through it, but some stop taking triptans because of it.
Drug Interactions You Can’t Ignore
Triptans and antidepressants are a risky mix. If you’re on an SSRI like sertraline or an SNRI like venlafaxine, you’re at risk for serotonin syndrome. This isn’t a myth. It’s rare, but it’s deadly. Symptoms include confusion, rapid heartbeat, high fever, muscle stiffness, and seizures. It happens when too much serotonin builds up in your brain. Triptans boost serotonin. So do SSRIs and SNRIs. Together, they can push levels past the safety line.
There’s no blanket ban on using them together. But doctors need to know what you’re taking. If you’re on antidepressants and your migraine suddenly gets worse or you feel strange after taking a triptan, get help immediately. Don’t wait.
Also, don’t mix triptans with other vasoconstrictors. That includes decongestants like pseudoephedrine. Even over-the-counter cold meds can raise your blood pressure dangerously when combined with a triptan.
Why Triptans Often Fail
Many people try a triptan once, it doesn’t work, and they give up. But failure isn’t always the drug’s fault. Timing is everything. If you wait until the pain is at its peak-say, two hours in-you’ve missed the window. The best results come when you take it within 20 minutes of the headache starting.
Another big reason triptans fail? Cutaneous allodynia. That’s when your skin becomes painfully sensitive. Brushing your hair, wearing a shirt, or even a light touch hurts. If you have this, triptans are only about 30-40% effective. Without it, they work 70-80% of the time. That’s why some people feel like triptans “stopped working.” They didn’t. Their migraine evolved.
And recurrence is common. Up to 40% of people get the headache back within 24 hours. That’s why some triptans, like frovatriptan, are dosed twice a day. But no more than two doses total per day. Exceed that, and you risk medication-overuse headache-a vicious cycle where the medicine itself causes more headaches.
What Comes After Triptans?
Triptans still make up nearly half of all migraine prescriptions. But new options are rising. Gepants (like ubrogepant and rimegepant) block CGRP without narrowing blood vessels. That makes them safe for people with heart conditions. Ditans like lasmiditan target a different serotonin receptor (5-HT1F) and don’t cause vasoconstriction at all.
Combination pills are also gaining ground. Sumatriptan plus naproxen (a common NSAID) works better than either alone. The combo gives a 27% chance of being pain-free at two hours, compared to 18% with sumatriptan alone.
But here’s the truth: triptans are still the most studied, most proven, and most affordable option for most people. Newer drugs cost 10 times more. And while they’re great for those who can’t use triptans, they’re not always better for those who can.
What to Do If Triptans Don’t Work
If one triptan fails, try another. Don’t assume they’re all the same. Switching isn’t giving up-it’s smart troubleshooting. Try rizatriptan if sumatriptan didn’t help. Try zolmitriptan nasal spray if pills make you nauseous.
If you’ve tried three or four and nothing works, it’s time to look beyond triptans. Talk to a neurologist. Consider preventive options like CGRP monoclonal antibodies. Or explore non-drug treatments like nerve stimulation devices.
And if you’re taking triptans more than 10 days a month, you’re at risk for medication-overuse headache. That’s not just a side effect-it’s a diagnosis. You might need to taper off under medical supervision before anything else will work.
Real Numbers, Real People
A survey of 2,500 migraine patients found:
- 68% found relief with at least one triptan
- 22% had to try two or more before finding one that worked
- 10% got no benefit from any triptan
That means 1 in 10 people with migraines have no option in this class. For them, alternatives aren’t optional-they’re essential.
And here’s the quiet truth: half of all people who start a triptan stop using it within a year. Not because it’s dangerous. But because it didn’t work well enough, or the side effects were too much, or it cost too much. That’s not failure. That’s the reality of migraine treatment.
Can I take a triptan if I have high blood pressure?
No, if your blood pressure is uncontrolled. Triptans narrow blood vessels, which can spike pressure dangerously. If your BP is stable and managed with medication, your doctor may allow it-but only after a full heart and vascular check. Never self-prescribe.
Why do I feel tightness in my chest after taking a triptan?
It’s a common side effect, not a heart attack. Triptans cause mild constriction of blood vessels throughout the body, including those around the heart and throat. This can feel like pressure, heaviness, or tightness. It usually lasts less than 15 minutes. If it lasts longer, or you have pain, sweating, or shortness of breath, seek help immediately.
Are triptans addictive?
No, triptans aren’t addictive in the way opioids or benzodiazepines are. They don’t create cravings or euphoria. But using them too often-more than 10 days a month-can cause medication-overuse headache. That’s not addiction. It’s a rebound effect your brain develops from too much acute treatment.
Can I take a triptan with my antidepressant?
It depends. SSRIs and SNRIs can increase the risk of serotonin syndrome when combined with triptans. The risk is low, but real. If you’re on one of these antidepressants, tell your doctor before using a triptan. They may adjust your dose, suggest a different migraine treatment, or monitor you closely.
What’s the best time to take a triptan?
At the first sign of headache pain-not during aura. If you have aura (flashing lights, tingling), wait until the pain starts. Taking it too early can worsen neurological symptoms. The sweet spot is within 20 minutes of pain onset. After that, effectiveness drops sharply.
Why do some people need to switch triptans?
Because not all triptans are the same. They vary in how fast they work, how long they last, and which serotonin receptors they target most. One person might respond to rizatriptan but not sumatriptan because of genetic differences in how their nerves react. Switching isn’t failure-it’s finding the right tool for your body.
Do triptans work for cluster headaches?
Yes, but only in specific cases. Sumatriptan injections are sometimes used for cluster headaches because they act fast. But triptans aren’t first-line for cluster headaches like they are for migraines. Oxygen therapy is more effective and safer for most cluster patients.
Can I take a triptan if I’m pregnant?
There’s no clear safety data. Most doctors avoid triptans during pregnancy unless the benefit clearly outweighs the risk. For mild migraines, acetaminophen or rest are preferred. If migraines are severe and frequent, your neurologist may consider a triptan-but only after careful evaluation.









Triptans are overhyped. I took sumatriptan three times last year and it did nothing. Just spent $80 on a fancy pill that made my chest feel like a vise. I’d rather nap and suffer.
Let’s be real-most people don’t understand pharmacokinetics. Rizatriptan’s 45% bioavailability isn’t magic, it’s molecular design. And yet, the average patient treats it like a lottery ticket. Meanwhile, the real issue is delayed administration. You wait until the pain’s at 9/10? Of course it fails. Timing isn’t a suggestion-it’s the protocol.
Triptans are dangerous for Indians we have high BP and liver issues and no one tells us this. My cousin took one after a headache and ended up in ICU. Doctors here just hand them out like candy. This is not healthcare this is profit-driven nonsense. We need better awareness not more pills.
I’ve been on SSRIs for years and I never knew triptans could mess with that. I took one last month and felt like my brain was vibrating. Didn’t connect the dots until now. Thanks for the warning.
Ugh. Another ‘triptych’ article. So much jargon. So little empathy. People aren’t data points. Some of us have migraines so bad we cry while brushing our hair. And now you’re lecturing us about CGRP levels? I just want to not die in a dark room.
Important clarification: cutaneous allodynia is a critical biomarker for triptan efficacy. When skin sensitivity develops, it signals central sensitization-meaning the migraine has progressed beyond vascular constriction into cortical hyperexcitability. Triptans target vascular and peripheral neural components, not central sensitization. That’s why efficacy drops to 30-40%. Gepants or ditans may be superior in this phase because they act centrally without vasoconstriction. Also, combination therapy with naproxen enhances efficacy by modulating peripheral inflammation-something triptans alone don’t touch.
Life is pain. Pain is inevitable. But triptans? They’re just another way we’ve learned to numb ourselves instead of listening to our bodies. We’ve turned migraines into a chemical problem when maybe, just maybe, it’s a signal. Sleep. Stress. Hydration. Light. All ignored. We take pills because it’s easier than changing our lives. But the pills don’t fix the life.
i tried 4 diff triptans and none worked but then i started using a migraine app to track triggers and now i avoid cheese and red wine and my attacks are way less. just sayin 😊
It is imperative to acknowledge that the pharmaceutical industry has systematically underemphasized the non-pharmacological dimensions of migraine management. The overreliance on triptans as a first-line intervention reflects a reductionist paradigm in neurology-one that prioritizes chemical intervention over holistic, environmental, and behavioral modulation. While triptans may provide temporary relief, they do not address the root causes-sleep deprivation, circadian disruption, chronic stress, and nutritional deficiencies-which remain empirically validated contributors to migraine pathophysiology. A truly patient-centered approach demands integration of cognitive behavioral therapy, biofeedback, and dietary modification alongside pharmacotherapy-not replacement.
My doc told me to try frovatriptan for my monthly migraines. Worked like a charm. But then I took two doses in one day because the headache came back. Next thing I know, I’m having headaches every day. Turns out I gave myself medication-overuse headache. Took 3 months to reset. Don’t be me.
Respectfully, triptans are tools not solutions. The true healer is discipline. Rest. Hydration. Consistent sleep. Medication should be the last resort, not the first. Your body speaks. Listen before you swallow.
Triptans are American medicine at its finest. If you’re from India or somewhere with no real healthcare you don’t get it. We have science. We have data. We have options. Stop complaining and take the pill. This isn’t a third world country.