NMS Symptom Checker
Neuroleptic Malignant Syndrome (NMS) is a rare but deadly reaction to dopamine-blocking medications. It's a medical emergency requiring immediate attention. This tool helps you recognize key signs of NMS based on the four critical symptoms.
Important Notes
Time is critical - NMS can be fatal if not treated within hours.
Don't wait - If you suspect NMS, call emergency services immediately.
Medications involved include antipsychotics (haloperidol, risperidone), anti-nausea drugs (metoclopramide), and others.
Check for these key symptoms:
- NMS can progress rapidly within hours
- Every minute counts
- Do not wait for symptoms to worsen
- Do not assume it's just "psychosis" or "infection"
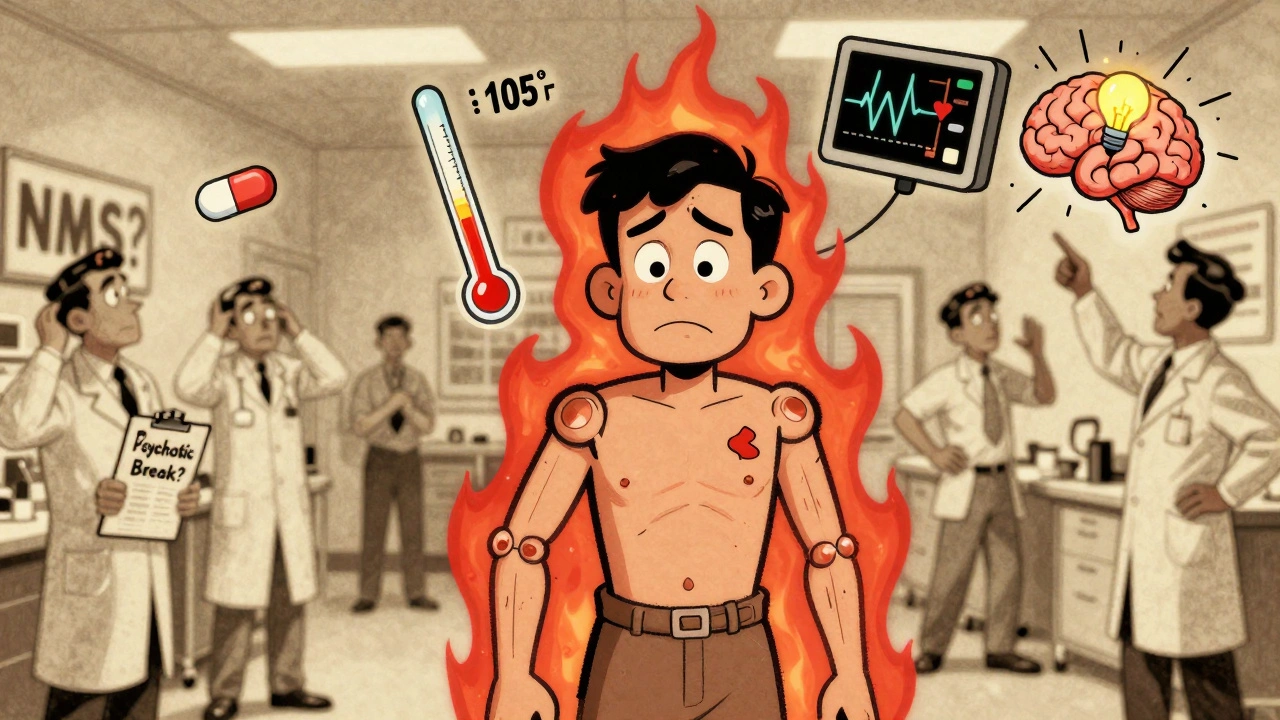
Neuroleptic Malignant Syndrome (NMS) isn’t something most people hear about until it’s too late. It doesn’t show up in TV medical dramas as a quick diagnosis. It doesn’t come with a clear warning label. But when it hits, it’s fast, brutal, and often mistaken for something else entirely. This isn’t just a side effect-it’s a medical emergency that can kill within hours if missed.
What Exactly Is Neuroleptic Malignant Syndrome?
NMS is a rare but deadly reaction triggered by medications that block dopamine in the brain. These include antipsychotics like haloperidol, risperidone, and olanzapine, but also anti-nausea drugs like metoclopramide and promethazine. The core problem? Dopamine stops working where it’s needed-especially in the parts of the brain that control movement, temperature, and alertness.
It’s not an allergy. It’s not psychosis getting worse. It’s a physiological breakdown. The body loses its ability to regulate muscle tension, heat, and heart function. The result? A dangerous mix of symptoms that can spiral out of control.
The Four Signs You Can’t Ignore
If someone on an antipsychotic suddenly starts acting strange, their muscles lock up, and their body temperature spikes, don’t wait. Look for the full tetrad:
- Muscle rigidity - not just stiffness, but lead pipe rigidity. When you try to move their arm or leg, it feels like bending a steel rod. No give. No resistance that changes with speed.
- High fever - 100.4°F (38°C) or higher, often climbing past 104°F (40°C). This isn’t a typical fever from infection. It’s internal heat from muscles locked in constant contraction.
- Altered mental state - confusion, agitation, mutism, or even coma. The person might stop speaking, stare blankly, or become violently restless. This often comes first, which is why it’s mistaken for a psychiatric flare-up.
- Autonomic chaos - rapid heartbeat (over 90 bpm), blood pressure swings, sweating, and fast breathing. Their body is in survival mode, but it’s running wild.
These symptoms usually show up within 1 to 2 weeks after starting or increasing a medication. But they can appear in as little as 48 hours-or even months later. There’s no safe window.
Why It’s So Often Missed
Doctors misdiagnose NMS in up to 12% of cases. Why? Because the symptoms look like other things.
Is the patient agitated and feverish? Maybe it’s an infection. Is their muscle tightness worsening? Maybe their schizophrenia is flaring. Is their heart racing? Maybe anxiety. Emergency room staff aren’t trained to think of NMS unless they’ve seen it before. A 2021 study found only 60% of ER physicians correctly identified NMS when it was staring them in the face.
One Reddit user shared how their father, on risperidone, stopped speaking and couldn’t move. The ER team thought it was a psychotic break. It took 48 hours to diagnose NMS. By then, his temperature was 105.1°F. He spent 9 days in the ICU.
Another common mistake? Blaming the patient. Families and even some clinicians assume the person is “just being difficult” or “not taking their meds properly.” That delay can be fatal.

What Happens Inside the Body
NMS isn’t just a list of symptoms-it’s a cascade of failures. When dopamine receptors are blocked in the hypothalamus, the brain loses its thermostat. In the basal ganglia, muscles freeze up. The constant contraction of muscles burns energy and releases massive amounts of creatine kinase (CK) into the blood.
CK levels often spike above 1,000 IU/L. In severe cases, they hit 100,000 IU/L. That’s the body’s muscle tissue breaking down-rhabdomyolysis. The muscle debris floods the kidneys, causing acute kidney injury in about 30% of cases. Some patients need dialysis.
Other signs show up in labs: high white blood cell count, low iron, acid in the blood, and elevated liver enzymes. These aren’t random. They’re clues that the body is under extreme stress.
NMS vs. Serotonin Syndrome vs. Malignant Hyperthermia
People confuse NMS with two other life-threatening conditions. Here’s how to tell them apart:
| Feature | Neuroleptic Malignant Syndrome (NMS) | Serotonin Syndrome | Malignant Hyperthermia |
|---|---|---|---|
| Onset | 1-14 days after starting/changing dose | Hours after taking serotonergic drug | Minutes after anesthesia exposure |
| Muscle Rigidity | Lead-pipe (uniform, constant) | Clonus (involuntary jerking), hyperreflexia | Masseter spasm (jaw tightness), generalized |
| Mental Status | Mutism, stupor, delirium | Agitation, hallucinations, tremor | Usually normal until late stage |
| Trigger | Antipsychotics, antiemetics | SSRIs, SNRIs, tramadol, MDMA | Volatile anesthetics, succinylcholine |
| Key Lab Finding | CK >1,000 IU/L (often >10,000) | Normal or mild CK elevation | High CK, acidosis, hyperkalemia |
Getting this wrong leads to the wrong treatment. Giving a serotonin syndrome patient dantrolene won’t help if they need cyproheptadine. Giving a malignant hyperthermia patient bromocriptine is useless if they need dantrolene and cooling.
How It’s Treated-And Why Speed Matters
There’s no magic pill. But there is a proven protocol. Every minute counts.
- Stop the drug immediately. No exceptions. Even if it’s the only thing keeping the person stable mentally, it has to go.
- Get to the ICU. Continuous monitoring of heart, temperature, kidneys, and breathing is non-negotiable.
- Cool the body. Ice packs, cooling blankets, IV fluids. Fever above 102°F (38.9°C) must be brought down fast to prevent brain damage.
- Hydrate aggressively. At least 1-2 liters of IV fluids right away, then 100-150 mL/hour to flush out muscle toxins and protect the kidneys.
- Use dantrolene or bromocriptine. Dantrolene (1-2.5 mg/kg IV) relaxes muscles and reduces heat production. Bromocriptine (2.5-10 mg every 8 hours) replaces dopamine activity. Not all hospitals use both, but many now do.
CK levels are checked every 6-12 hours. They usually peak at 72-96 hours. Recovery takes 7-10 days if treated early. But if treatment is delayed more than 24 hours, complications like kidney failure or pneumonia become far more likely.

Who’s at Highest Risk?
NMS isn’t random. Certain patterns show up again and again:
- High-potency first-generation antipsychotics - haloperidol, fluphenazine. These carry a 0.5-2% risk.
- Rapid dose increases - jumping haloperidol by more than 5 mg/day is a red flag.
- Parenteral (injection) use - intramuscular antipsychotics spike blood levels too fast.
- Combining with lithium - this combo triples the risk.
- Young males with mood disorders - men under 40 with bipolar disorder are more likely than those with schizophrenia.
- Stopping Parkinson’s meds - sudden withdrawal of levodopa can trigger NMS-like symptoms in 5% of cases.
And here’s the scary part: 12% of NMS cases happen in people on normal, approved doses-with no known risk factors. That’s why every patient on these drugs needs to be watched.
Recovery and Long-Term Impact
Survival rates have improved dramatically-from 76% in the 1980s to 95% today-thanks to faster recognition and better ICU care. But recovery isn’t simple.
Many survivors have lingering muscle weakness. One person on a schizophrenia support forum said it took 8 weeks to walk without help. Others report chronic pain, fatigue, and fear of ever taking antipsychotics again.
A 2022 survey found 65% of NMS survivors refused to restart antipsychotics-even when their psychosis returned. That creates a brutal dilemma: stay mentally ill, or risk dying from a reaction.
Some patients are later switched to atypical antipsychotics like quetiapine or clozapine, which have a much lower risk (0.01-0.02%). But even then, caution is needed. NMS can still happen.
What You Need to Know Now
If you or someone you care for is on an antipsychotic or anti-nausea drug:
- Know the four signs: rigidity, fever, mental changes, autonomic chaos.
- Don’t wait for “it to pass.” If symptoms appear, go to the ER and say: “I’m worried about Neuroleptic Malignant Syndrome.”
- Keep a list of all medications-including over-the-counter ones like metoclopramide (Reglan) or promethazine (Phenergan).
- Ask your doctor: “What’s the risk of NMS with this drug? What should I watch for?”
- Carry a medical alert card or phone note that says: “On antipsychotic. Risk of NMS. Do not delay treatment.”
NMS is rare-but not rare enough to ignore. It doesn’t care if you’re young, healthy, or on a low dose. It strikes without warning. The only thing that saves lives is awareness-and acting fast.
Can NMS happen with medications other than antipsychotics?
Yes. While antipsychotics are the most common trigger, NMS can also be caused by anti-nausea drugs like metoclopramide (Reglan) and promethazine (Phenergan). These are dopamine blockers too. About 15% of NMS cases come from these medications, not psychiatric drugs. Even some older antihistamines and anti-Parkinson’s drugs can contribute if used incorrectly.
Is NMS the same as a drug allergy?
No. NMS is not an allergic reaction. It doesn’t involve histamine, hives, or swelling. It’s a toxic response caused by dopamine blockade in the brain and muscles. You can’t test for it with skin tests or blood allergy panels. It’s a pharmacological effect, not an immune one.
How long does it take to recover from NMS?
With prompt treatment, most people start improving within 3-7 days. Full recovery usually takes 7-10 days. But muscle damage can linger. Some survivors report weakness, pain, or fatigue for weeks or even months. About 15% still have noticeable muscle problems at 30 days after onset.
Can NMS come back if I take antipsychotics again?
Yes. If you’ve had NMS once, you’re at higher risk of getting it again-even with a different drug. Re-challenging with any dopamine-blocking medication is dangerous. If absolutely necessary, doctors may try a very low dose of a low-risk antipsychotic like clozapine under strict monitoring. But many patients avoid all antipsychotics after NMS due to fear.
Are second-generation antipsychotics safe from NMS?
They’re much safer, but not risk-free. Second-generation drugs like olanzapine, quetiapine, and aripiprazole have reduced NMS risk to 0.01-0.02%-a 95% drop from older drugs. But cases still happen, even on therapeutic doses. The FDA now requires all antipsychotics to carry a black box warning about NMS, regardless of generation.
What should I do if I suspect NMS in someone?
Call emergency services immediately. Tell them you suspect Neuroleptic Malignant Syndrome. Do not wait for a doctor’s appointment. Do not assume it’s just psychosis or infection. Time is critical. If you know what medications the person is taking, bring the list to the hospital. If possible, stop the drug before transport-but only if it’s safe to do so. Never try to treat this at home.






Yeah right, like anyone in the ER actually reads a damn blog post before they diagnose 'psychotic break' and dose someone with more antipsychotics. I’ve seen it. Dad was on risperidone, started twitching, fever hit 104, and the nurse told us he was just 'acting out.' Took 36 hours before someone finally checked his CK levels. By then, his kidneys were already screaming. This isn’t education-it’s a funeral waiting to happen.
While I appreciate the clinical detail, the tone of this post borders on alarmist. NMS is exceedingly rare, and the vast majority of patients on antipsychotics never experience it. To suggest that every patient should carry a medical alert card is impractical and potentially harmful-it stigmatizes necessary psychiatric treatment. Medicine requires balance, not fear-driven overcorrection.
You speak of dopamine blockade as if it were a mechanical failure-but it is a metaphysical unraveling. The mind, when denied its natural neurotransmitter, becomes a cathedral without a priest. The body, in its desperation, burns itself alive-not from poison, but from the silence of its own chemistry. This is not merely a syndrome. It is the soul screaming through muscle and fever. And yet, we call it 'side effect' and move on. What kind of civilization reduces transcendence to a pharmacological footnote?
Let’s be real-this whole system is rigged. Big Pharma knows NMS is deadly, but they keep pushing these drugs because they make billions. The FDA? They’re asleep. Doctors? They’re trained to trust the label, not the patient. And now you want us to carry cards? Like we’re criminals? This isn’t prevention-it’s damage control for a system that refuses to change.
so like… if you get NMS from reglan… is that like… a bad tummy pill revenge? 😐 i mean, i took that for nausea and now i’m supposed to be scared of my own digestion??
It is imperative to emphasize that the diagnostic criteria for Neuroleptic Malignant Syndrome, as delineated by the DSM-5 and supported by the American Psychiatric Association, require the presence of all four cardinal signs: muscular rigidity, hyperthermia, altered mental status, and autonomic instability. Failure to meet this full constellation may lead to misclassification, which in turn may result in inappropriate therapeutic interventions. Therefore, while vigilance is warranted, diagnostic precision remains paramount.
Of course it’s rare. That’s why it’s only killing Americans. In Europe, they’ve got real doctors who know how to spot this. Here? We’re too busy arguing about gender pronouns to notice a patient turning into a human furnace. You want to save lives? Start by firing the ER nurses who think 'agitation' means 'just be a little nicer to them.'
This is exactly the kind of information that needs to be shared-not just with clinicians, but with families, caregivers, and patients themselves. I’ve worked in mental health for 18 years, and I’ve seen too many people dismissed because their symptoms didn’t fit the 'expected' profile. Thank you for making this so clear. If you’re reading this and you’re on an antipsychotic, please, keep this page open. Bookmark it. Print it. Your life might depend on it.
Wait… so if NMS is caused by dopamine blockers… and dopamine blockers are used to treat psychosis… and psychosis is sometimes caused by government mind control… then is NMS just the body fighting back against the surveillance state? 🤔 I mean, think about it-why else would they hide this? Why don’t they warn people? It’s all connected. They don’t want you to know your own body can rebel.
okay i’m a nurse and i’ve seen this twice. first time i thought it was sepsis. second time i thought it was catatonia. both times we almost lost them. don’t wait. if someone on antipsychotics goes quiet + hot + stiff → say NMS out loud. even if you’re wrong. better to be loud and wrong than quiet and dead. you got this. ❤️