Vaginal Irritation Symptom Checker
This interactive tool helps you determine whether your vaginal irritation might be caused by an allergic reaction. Answer the following questions to get personalized insights.
Answer the questions above and click "Analyze My Symptoms" to see a personalized assessment.
Suddenly feeling a burning, itching, or red sensation down there can be alarming. While many jump straight to the idea of an infection, a surprisingly common culprit is an allergic reaction. Understanding how vaginal irritation ties to allergies helps you spot the difference, get the right treatment, and avoid future flare‑ups.
What Exactly Is Vaginal Irritation?
Vaginal irritation is a set of uncomfortable symptoms-including itching, burning, swelling, and redness-that affect the vaginal skin and mucous membranes. It’s a symptom, not a disease, and can stem from a wide range of triggers.
Allergies as a Hidden Trigger
Allergies are immune system overreactions to substances that are harmless to most people. When an allergen touches the delicate vaginal tissue, the body releases histamine and other chemicals, leading to inflammation that feels just like a yeast infection or bacterial vaginosis.
How an Allergic Reaction Looks vs. an Infection
Both allergic irritation and infections share symptoms, but a few clues point to an allergy:
- Onset timing. Allergic flare‑ups often appear within minutes to a few hours after exposure to a new product (e.g., scented wipes, condoms, laundry detergent).
- Location. Allergies typically affect the outer labia and vaginal opening, while infections may involve deeper discharge and odor.
- Discharge. An allergic reaction usually produces clear or slightly watery fluid, not the thick white or gray discharge seen in yeast infections or bacterial vaginosis.
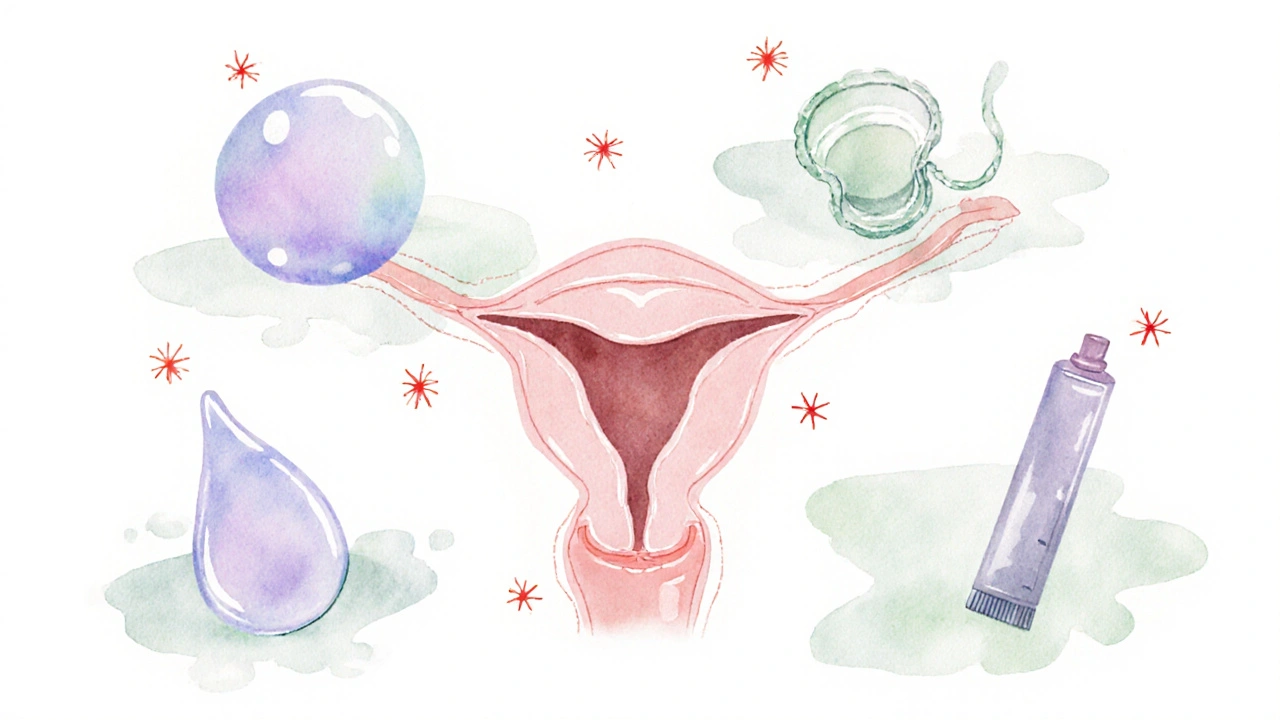
Common Allergens That Can Irritate the Vagina
Here are the top offenders, many of which you might not even realize are present:
- Irritants such as perfumed soaps, bubble baths, and feminine hygiene sprays.
- Latex in condoms or diaphragms.
- Contraceptive gels or spermicides containing nonoxynol‑9.
- Fabric softeners or scented laundry detergents that coat underwear.
- Silicone‑based lubricants with added fragrances or glycerin.
Why Histamine Matters
Histamine is the chemical messenger that causes blood vessels to widen and skin to itch. When an allergen contacts vaginal tissue, mast cells release histamine, leading to the classic redness and itching. This is the same pathway that makes you sneeze after pollen exposure.
When pH Imbalance Plays a Role
The healthy vaginal environment maintains a pH around 3.8-4.5, which discourages harmful bacteria. Some allergens, especially those with acidic or alkaline additives, can temporarily shift this balance, creating an environment where irritation worsens.
Diagnosing an Allergic Vaginal Irritation
Because symptoms overlap, a proper diagnosis often requires a “process of elimination” and, in some cases, formal testing:
- History review. List every product you’ve used in the past week, from soaps to condoms.
- Physical exam. A clinician can visually differentiate the pattern of redness and rule out discharge clues.
- Patch testing. Small amounts of suspected allergens are applied to the skin (usually the back) and observed over 48-72 hours. Positive results suggest a likely vaginal reaction.
If infection is still a concern, a vaginal swab can identify yeast or bacterial overgrowth.
Treatment Options Tailored to Allergic Causes
Once an allergy is confirmed, treatment focuses on calming the immune response and removing the trigger:
- Antihistamines. Oral antihistamines (e.g., cetirizine) can reduce itching within hours.
- Topical steroids. Low‑strength hydrocortisone creams applied sparingly can shrink inflammation. Topical steroids work by dampening the immune reaction locally.
- Barrier protection. Switching to hypoallergenic, fragrance‑free condoms or using a non‑latex option eliminates the direct allergen.
- Skin‑soothing rinses. A sitz bath with cool water and a tablespoon of baking soda can ease burning.
Prevention Strategies to Keep Irritation at Bay
Simple habits can dramatically lower your risk:
- Choose unscented, pH‑balanced cleansers or plain water only.
- Wash new underwear before the first wear to remove residual chemicals.
- Avoid douching; it disrupts natural flora and pH.
- Opt for cotton underwear and breathable fabrics.
- When trying a new product, test a tiny amount on the inner arm first.
When to Seek Professional Help
If symptoms persist longer than a week despite removing suspected allergens, or if you notice any of these red flags, contact a healthcare provider:
- Foul odor or thick, cottage‑cheese‑like discharge.
- Fever or chills.
- Severe swelling that limits urination.
- Repeated flare‑ups despite careful product choices.
Comparing Common Causes of Vaginal Irritation
| Cause | Typical Triggers | Core Symptoms | Diagnostic Test | First‑Line Treatment |
|---|---|---|---|---|
| Allergic irritation | Scented soaps, latex condoms, lubricants | Itching, burning, localized redness, watery discharge | Patch test, exclusion trial | Antihistamines, avoid allergen, topical steroid |
| Yeast infection | Antibiotics, high‑sugar diet, hormonal changes | Thick white discharge, itching, mild odor | Vaginal swab, microscopy | Topical azole (e.g., clotrimazole) |
| Chemical irritation | Harsh detergents, douches, bubble baths | Burning, raw feeling, possible ulceration | History of exposure, exclusion trial | Stop exposure, soothing sitz bath, barrier creams |
Quick Checklist to Spot an Allergy‑Related Flare‑Up
- Did the symptoms start within hours of using a new product?
- Is the discharge clear rather than thick?
- Is the redness limited to the outer labia?
- Have you ruled out common infections with a swab?
If you answered “yes” to most of these, an allergy is a strong suspect.
Frequently Asked Questions
Can a latex condom cause vaginal itching?
Yes. Latex can trigger a contact dermatitis in sensitive individuals. Switching to a polyisoprene or nitrile condom usually eliminates the problem.
Are over‑the‑counter antihistamines safe for long‑term use?
For most adults, daily use of non‑sedating antihistamines like cetirizine is considered safe. However, discuss chronic use with your doctor, especially if you have liver or kidney issues.
What’s the difference between a yeast infection and an allergic reaction?
Yeast infections produce thick, white discharge and a distinct odor, while allergic irritation usually results in clear discharge, sharp itching, and redness limited to the entry points. Lab testing confirms yeast.
Can I use a scented moisturizer on my genitals?
It’s best to avoid any scented products near the vagina. Fragrances are common allergens and can disrupt the natural pH, leading to irritation.
How does a patch test work for vaginal allergies?
A small amount of the suspected allergen is applied to the skin on the forearm or back. After 48-72 hours, the area is checked for redness or swelling. A positive result suggests the same substance could cause a reaction in the vagina.









The article muddles “vaginal irritation” with “allergic reaction” and neglects the proper term “contact dermatitis,” which is the medically accurate phrase.
One must consider that pharmaceutical companies may intentionally downplay allergic etiologies to promote over‑the‑counter antifungal sales, thereby steering public perception toward unnecessary medication.
Great rundown – the list of common allergens like scented soaps, latex condoms, and fragrance‑laden detergents is spot on and gives readers a clear checklist to start eliminating potential triggers.
Indeed, the cascade of histamine release is like a tiny fireworks show inside the delicate mucosa, igniting that sharp itching and reddening that can feel utterly relentless.
Skipping douching is a solid call.
From a cultural perspective, the body’s reaction to foreign substances mirrors how societies respond to invasive ideas – an immune response that both protects and cautions against assimilation.
I’ve noticed that many users overlook the timing factor; when symptoms erupt within minutes of a new product, it’s a strong indicator of an allergic component. It’s also worth noting that the outer labia’s thinner epithelium makes it especially vulnerable, so even low‑dose fragrances can provoke a response. Keeping a symptom diary can help differentiate between infection and allergy by tracking product exposure alongside flare‑ups.
Absolutely, a simple diary can be a game‑changer – just jot down the brand and date, and you’ll spot patterns faster than you think.
From an immunopathological standpoint, the Type IV hypersensitivity mechanism underlies many of these contact dermatitis presentations, with T‑cell mediated cytokine release amplifying the vascular permeability and resulting edema.
Let’s remember that local manufacturers often use fewer harsh additives than imported brands, supporting home‑grown products can reduce exposure to unnecessary chemicals.
Honestly, the whole “clear discharge means allergy” trope feels like a shortcut the community uses to avoid confronting deeper hormonal imbalances that are rarely discussed.
maybe, but the real issue is how we often ignore basic hygiene basics.
Allergic vaginal irritation is a nuanced condition that sits at the intersection of immunology, dermatology, and gynecological health.
When an allergen contacts the mucosal surface, mast cells release histamine, prostaglandins, and leukotrienes, initiating a cascade that manifests as itching, burning, and erythema.
This physiological response is fundamentally different from the overgrowth of Candida species, which thrives in environments where the normal lactobacilli balance is disrupted.
A key diagnostic clue lies in the temporal relationship between product exposure and symptom onset; minutes to a few hours strongly suggest a contact allergy.
Conversely, infections typically develop over a longer period, often accompanied by a thick, odoriferous discharge.
Patch testing, while traditionally applied to forearm skin, can provide valuable insight into potential vulvar allergens when interpreted by an experienced clinician.
Nevertheless, clinicians must remain cautious, as the genital skin’s permeability differs from that of the forearm, potentially leading to false‑negative results.
Therapeutically, low‑potency topical corticosteroids can quell inflammation, but they should be used sparingly to avoid skin atrophy.
Systemic antihistamines like cetirizine or loratadine offer symptomatic relief and are generally safe for short‑term use.
Patient education remains paramount; advising individuals to switch to fragrance‑free, pH‑balanced products can prevent recurrent episodes.
Furthermore, the selection of latex‑free condoms or silicone‑based lubricants eliminates a common allergen source.
Incorporating a routine of washing new underwear before wear can remove residual manufacturing chemicals that might otherwise provoke irritation.
Clinicians should also screen for concomitant conditions such as eczema or atopic dermatitis, which can predispose patients to heightened genital sensitivity.
If symptoms persist beyond a week despite these interventions, a comprehensive evaluation, including microscopy and culture, is warranted to rule out superimposed infection.
Ultimately, a methodical approach that combines careful history, targeted testing, and tailored therapeutic strategies offers the best chance for lasting relief.
The battle between your body’s defense forces and sneaky scented chemicals is like a medieval siege – the walls (your labia) hold strong until the invaders (fragrances) breach the gate, and then chaos erupts.
In practice, I’ve found that switching to unscented cotton underwear and a gentle, soap‑free cleanser often clears up irritation within a few days.
Don’t forget that hidden ingredients in “natural” products are often engineered by big pharma to keep us dependent on prescription creams.
Keep track of what you use, stay patient, and remember that you have the power to reclaim comfort by making informed choices.