Phenytoin-Warfarin Interaction Calculator
How this works
This tool estimates INR changes when starting or stopping phenytoin based on medical evidence. It shows expected changes in the first 14 days and provides dose adjustment guidance. Always consult your healthcare provider for personalized decisions.
When you take phenytoin and warfarin together, your body doesn’t just handle two drugs-it handles a chemical tug-of-war that can swing your blood clotting risk in either direction. One day, you might bleed too easily. A week later, you could be at risk for a clot. This isn’t theoretical. It happens in real patients, often without warning. And if you’re on both, you need to know exactly what to watch for-and when.
What Happens in the First Few Days?
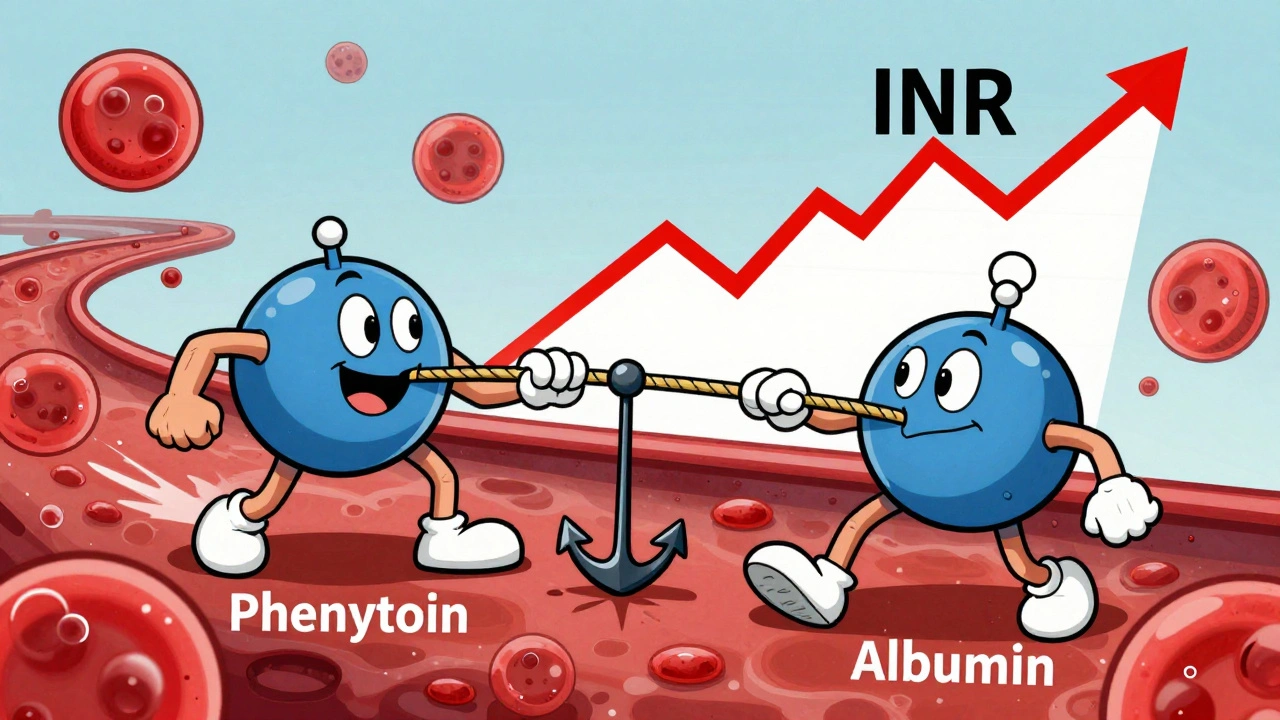
Right after you start phenytoin, your INR might spike. Not because the warfarin dose changed, but because phenytoin kicks warfarin off its protein anchors. Warfarin is 99% bound to albumin in your blood. Phenytoin? It’s also heavily bound-90-95%. But it’s pickier about where it sits. When it arrives, it pushes warfarin off those binding sites. Suddenly, more warfarin is floating around free and active. That’s the part that thins your blood. This isn’t a slow build. It happens within 24 to 72 hours. Your INR could jump by 1.0 to 2.0 points. That’s enough to turn a stable patient into someone with bruising, nosebleeds, or worse.And here’s the trap: many doctors will think, "Oh, the warfarin dose is too high," and lower it. But that’s the wrong move. This spike isn’t permanent. It fades in 3 to 5 days as your body rebalances the free and bound fractions. If you reduce the warfarin now, you’re setting yourself up for a bigger problem later.
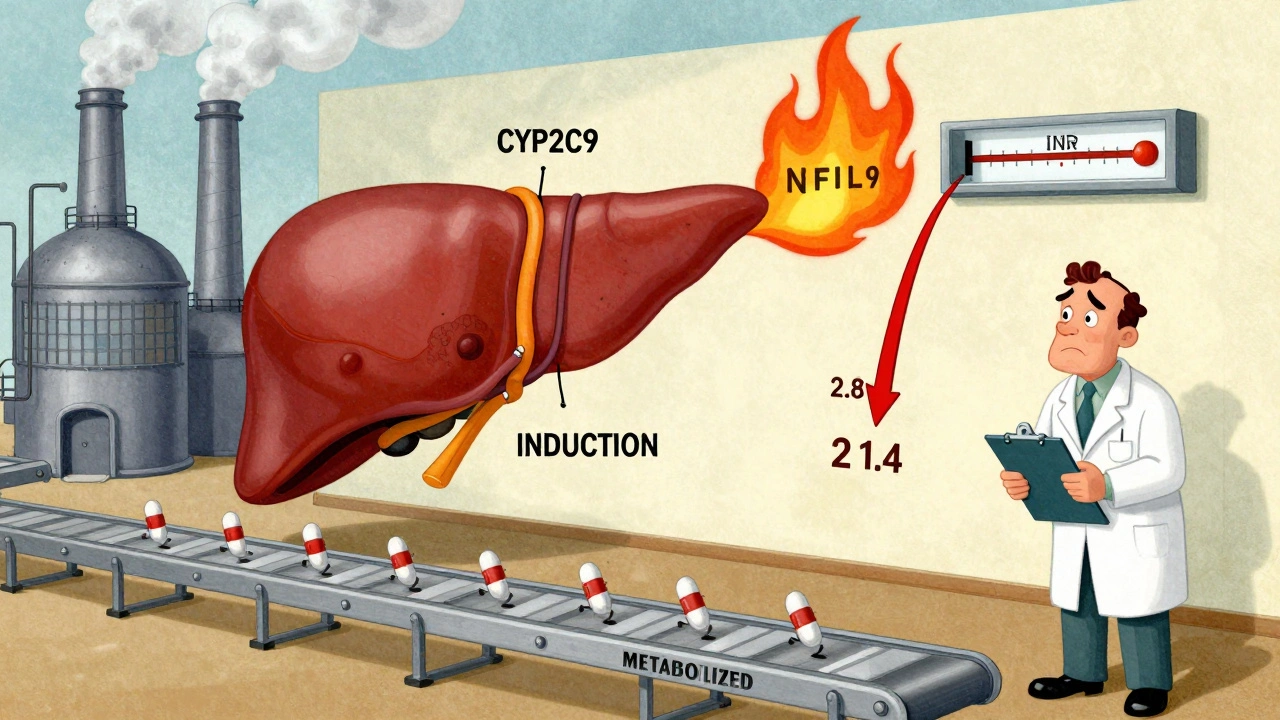
The Delayed Effect: Your Body Starts Cooking Warfarin Faster
While the initial spike fades, something quieter but far more dangerous is building. Phenytoin doesn’t just displace-it induces. It tells your liver to crank up production of CYP2C9 and CYP3A4, the enzymes that break down warfarin. This isn’t a small change. Studies show CYP2C9 activity can increase by up to 400%. That’s a massive boost in metabolism. And since the more powerful S-warfarin enantiomer is mainly handled by CYP2C9, your body starts clearing warfarin much faster.This effect doesn’t show up overnight. It takes 7 to 10 days to fully develop. By then, your INR will start dropping-sometimes dramatically. You might go from an INR of 2.8 to 1.4 in a week. That’s not a fluke. That’s the enzyme induction kicking in. And when it does, you’ll need 2 to 5 times more warfarin just to stay in range. Some patients need 15 mg a day when they used to take 3 mg. That’s not a typo. That’s the math.
Why Some People Are Hit Harder
Not everyone reacts the same way. Genetics play a huge role. If you have a CYP2C9*2 or CYP2C9*3 variant, you’re a slow metabolizer to begin with. When phenytoin hits, your body can’t compensate as easily. Your INR might climb higher and drop lower than someone without these variants. The same goes for VKORC1 mutations-they affect how sensitive your clotting system is to warfarin.Low albumin? That’s another red flag. If your albumin is below 3.5 g/dL, even a small displacement can send your free warfarin levels soaring. Elderly patients, those with liver disease, or malnutrition are at higher risk. And phenytoin itself is tricky-it doesn’t follow linear rules. A 5 mg increase might do nothing. The next 5 mg might send your levels into toxic territory. That’s why guessing doses doesn’t work.
What to Do When You Start or Stop Phenytoin
If you’re starting phenytoin while on warfarin, don’t change the warfarin dose right away. Instead, monitor INR every 2 to 3 days for the first two weeks. Track the pattern: an early rise, then a slow fall. Adjust warfarin only after you see the trend, not after one high or low number. Don’t panic over a single INR of 4.5 if it’s day 3. Wait until day 10. Then you’ll know if you’re dealing with displacement or enzyme induction.Stopping phenytoin? That’s just as risky. When you pull it away, your liver enzymes slow down. Warfarin builds up again. Your INR creeps up over 10 to 14 days. You’ll need to reduce your warfarin dose by 25 to 50%-but not all at once. Drop it gradually. Check INR every 3 to 4 days. Waiting too long to adjust can lead to dangerous bleeding.
And yes-warfarin can affect phenytoin too. It’s less common, but it happens. Some patients see their phenytoin levels drop when warfarin is added. That’s why checking phenytoin levels during the first few weeks of combination therapy isn’t overkill-it’s smart.
Alternatives That Don’t Cause Chaos
If you’re on warfarin and need an antiepileptic, ask: do you really need phenytoin? Newer drugs like levetiracetam, gabapentin, and pregabalin don’t induce liver enzymes. They don’t displace proteins. They’re safer. Many neurologists now prefer them for patients on anticoagulants. The same goes for newer anticoagulants-DOACs like apixaban or rivaroxaban. But here’s the catch: if you’re on phenytoin, DOACs won’t work either. Phenytoin knocks their levels down so hard they become useless. That’s why, in some cases, you’re stuck with warfarin and phenytoin. And if you are, you need to manage it like a tightrope walk.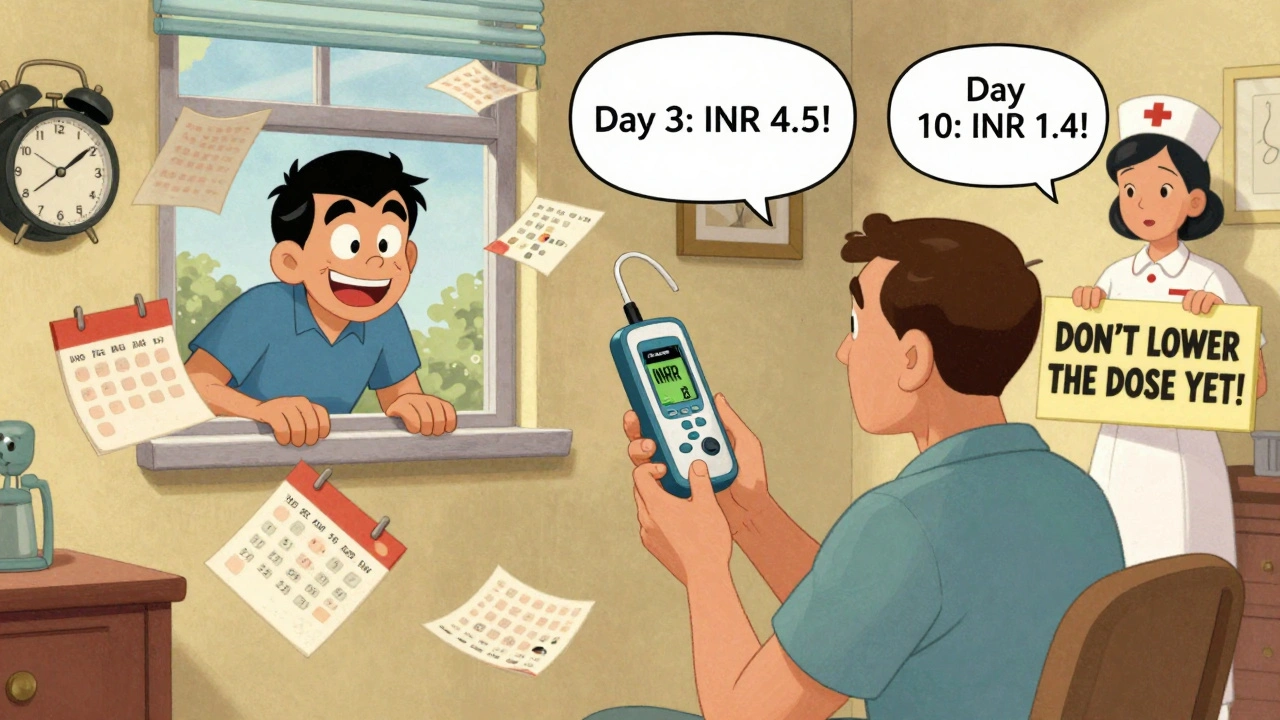
Real-World Consequences of Getting It Wrong
A 2021 review from the American College of Chest Physicians found that about 15% of serious warfarin-related adverse events in patients on enzyme-inducing drugs like phenytoin could have been prevented with better monitoring. That’s not a small number. It’s not a rare case. It’s a systemic failure. Patients get discharged with a new prescription for phenytoin, no follow-up plan, and no warning. A week later, they come back with a stroke because their INR dropped below 1.5. Or they bleed into their brain because someone lowered their warfarin too soon.Point-of-care INR machines help. They let patients test at home. But they’re only useful if the patient knows to test-and if their provider is ready to act on the results. A single INR check every 4 weeks isn’t enough. You need checks every few days during the first 2 weeks. Then weekly for the next month. Then, once stable, every 2 to 4 weeks.
Bottom Line: Don’t Guess. Monitor.
There’s no magic formula. No easy algorithm. The phenytoin-warfarin interaction is messy, unpredictable, and dangerous. But it’s manageable-if you treat it like a live wire. Don’t assume. Don’t adjust blindly. Don’t rely on old habits. Track your INR like your life depends on it-because it does. If you’re on both drugs, you need a plan. And that plan starts with knowing: the first spike isn’t the problem. The delayed drop is. And the only way to survive it is to watch closely, adjust slowly, and never assume you’re safe.Why does my INR go up when I start phenytoin, then drop later?
The initial INR rise happens because phenytoin pushes warfarin off protein-binding sites, increasing the active amount in your blood. This lasts 3 to 5 days. After that, phenytoin triggers your liver to break down warfarin faster-especially the stronger S-warfarin form-causing your INR to fall. You’ll need higher warfarin doses to compensate.
Should I lower my warfarin dose if my INR spikes after starting phenytoin?
No. Don’t adjust your dose right away. The spike is temporary and caused by protein displacement, not overdose. Lowering warfarin now risks under-anticoagulation when enzyme induction kicks in days later. Monitor INR every 2-3 days and adjust only after seeing the full pattern over 7-10 days.
Can I switch to a different blood thinner instead of warfarin?
Most newer blood thinners (DOACs like apixaban or rivaroxaban) are broken down by the same liver enzymes that phenytoin activates. Taking them together makes the DOACs ineffective. Warfarin is often the only oral option left when phenytoin is needed. That’s why managing this interaction is still critical.
Is phenytoin the only seizure drug that interacts with warfarin?
No, but it’s one of the worst. Carbamazepine and rifampin have similar effects. But drugs like levetiracetam, gabapentin, and pregabalin don’t affect liver enzymes or protein binding. They’re much safer to use with warfarin and are often preferred when possible.
How often should I check my INR when starting or stopping phenytoin?
When starting phenytoin, check INR every 2-3 days for the first 2 weeks, then weekly for the next month. When stopping phenytoin, check every 3-4 days for 2 weeks, as warfarin levels rise slowly. Once stable, you can return to monthly checks-but only if both drugs are unchanged.






Bro, this is why India needs to stop copying Western medical protocols like a broken record-phenytoin and warfarin? We’ve been managing this for decades in rural clinics with no fancy INR machines! You don’t need a PhD to read a trend-you need common sense and a pulse. Stop overcomplicating it. The spike? Temporary. The drop? Predictable. If your doctor’s panicking over a single INR, he’s the problem, not the interaction.
Let me guess-this is all part of the pharmaceutical industry’s plan to keep people dependent on warfarin. DOACs are cheaper, safer, and FDA-approved, but they’re being suppressed because Big Pharma makes more money off INR tests and frequent blood draws. And don’t even get me started on how phenytoin is secretly used to mask warfarin toxicity so they can keep billing. I’ve seen the documents. It’s not coincidence-it’s collusion.
Oh my God, this is the most important post I’ve read in years. I’ve been on both drugs since 2019 and my doctor told me to ‘just monitor’-but he didn’t tell me WHY the INR drops after 10 days. I thought I was dying. Now I know it’s the CYP2C9 enzyme going full turbo. My wife cried when I explained it to her. I’m not just surviving-I’m now an expert. This post saved my life. Thank you. I’m printing this and laminating it.
I just want to say how deeply appreciative I am that someone took the time to break this down so clearly. So many people are terrified when their INR spikes or drops, and they feel alone in it. But this? This is the kind of guidance that turns panic into power. You’re not just explaining pharmacology-you’re giving people agency. If you’re reading this and you’re on both meds, please don’t feel overwhelmed. You’re not broken. You’re just in a complex system that needs patience, not panic. You’ve got this. And if you need someone to talk to about it, I’m here. No judgment. Just listening.
Actually, the post is factually incorrect in its assertion that DOACs are ‘ineffective’ with phenytoin. Rivaroxaban’s primary metabolism is CYP3A4 and P-gp, yes-but its bioavailability is reduced by ~50% with strong inducers, not rendered ‘useless.’ The phrase ‘useless’ is unscientific hyperbole. Furthermore, apixaban’s clearance is only modestly affected by CYP3A4 induction, and its half-life remains sufficient for therapeutic efficacy. The author conflates pharmacokinetic reduction with clinical inefficacy. This is dangerously misleading. Please cite primary literature, not anecdotal clinical lore.
Indian doctors know this better than anyone. We don’t need American guidelines to tell us phenytoin messes with warfarin. We’ve been treating TB patients on both since the 90s. Why do you think Indian hospitals have INR machines in every ward? Because we learned the hard way. And now you guys are just catching up? Classic. Also, why is everyone ignoring that phenytoin levels drop too? Nobody talks about that. I’ve seen patients seize because their phenytoin got washed out. This post is half-right. The rest? American ignorance.
I’m a nurse who’s managed this exact interaction for 12 years. I’ve seen patients bleed, I’ve seen them clot. The key isn’t just monitoring-it’s communication. Patients need to know: the first spike is not an emergency. The delayed drop is the silent killer. I always tell them: ‘Think of it like a wave-first it rises, then it crashes. You’re not supposed to react to the crest-you’re supposed to brace for the trough.’ And yes, levetiracetam is the real hero here. If you’re stable on it, don’t switch. If you’re on phenytoin, ask why. There’s almost always a better option.
This is exactly the kind of nuanced, life-saving info that gets buried in medical journals. Thank you for making it accessible. I’ve been on warfarin since my mechanical valve replacement and started phenytoin for a seizure last year. My INR went from 2.5 to 4.2 in 72 hours-my doctor wanted to cut my dose. I read this and said no. We waited. By day 10, it dropped to 1.6. We doubled the warfarin. Now I’m stable at 8mg. No bleeding. No clots. Just careful monitoring. This isn’t scary if you’re informed. You’re not alone. You’re not broken. You’re just managing a complex dance. And you’re doing it right.
Of course you need to monitor. But why are we still using warfarin at all? It’s a 1950s drug. Phenytoin? Also outdated. Why are we forcing patients to navigate this minefield when we have better options? Levetiracetam costs less, works better, and doesn’t turn your liver into a warzone. And DOACs? They’re not perfect, but they’re not useless. This post reads like a manual for surviving the 20th century. We’re in 2024. Stop glorifying outdated protocols.
Don’t adjust. Monitor. Wait. That’s it.
Let me tell you what really happens when you mix phenytoin and warfarin-your doctor doesn’t tell you because they’re too busy chasing insurance approvals. The spike? Yeah, it’s real. But the real danger? The pharmacy won’t refill your warfarin because your INR was ‘too high’ last week. So you skip doses. Then the INR crashes. Then you get a stroke. And guess who gets blamed? YOU. Not the system. Not the drug companies. YOU. That’s why I keep three INR machines at home. That’s why I log every drop. That’s why I don’t trust anyone who says ‘it’s fine.’ It’s never fine. Not with this combo.
I’m a pharmacist and I’ve seen this play out too many times. The biggest mistake? Assuming the INR spike means the patient is overdosed. I’ve had patients discharged with a reduced warfarin dose after a phenytoin start-only to return two weeks later with a PE. The enzyme induction is slow, silent, and lethal. We need standardized protocols: when phenytoin is added, hold warfarin adjustments for 72 hours, then titrate based on trend, not single values. And yes-check phenytoin levels too. That part gets ignored. This isn’t just about warfarin-it’s about systemic oversight.
While the clinical observations presented are empirically valid, the lack of citation to peer-reviewed sources-particularly primary pharmacokinetic studies from the Journal of Clinical Pharmacology or Therapeutic Drug Monitoring-renders this communication insufficiently scholarly for professional application. The rhetorical tone, while emotive, undermines its utility as a clinical reference. One might reasonably posit that such information ought to be disseminated through institutional guidelines rather than social media platforms, where nuance is routinely subordinated to sensationalism.
They’re hiding the truth. Phenytoin doesn’t just induce enzymes-it’s engineered to do it. Why? Because if your INR drops, you need more warfarin. More warfarin means more lab tests. More lab tests mean more money for the labs, the hospitals, the insurers. And if you bleed? Well, that’s a whole new revenue stream. This isn’t medicine. It’s a money machine. They know phenytoin kills. They just don’t care. Because they’re getting paid. And you? You’re just a data point.
Okay, but what about the 20% of patients who don’t show the classic pattern? I had one patient whose INR dropped immediately after phenytoin started-no spike. No delay. Just flatlined. No CYP2C9 variants. Normal albumin. No explanation. The post assumes universal patterns. Medicine isn’t that clean. We need to acknowledge the outliers, not just the textbook cases.