Imagine you’re in an accident. You’re unconscious. The paramedics rush you to the ER. They need to know what’s in your system-fast. But you can’t tell them. That’s where a simple metal bracelet on your wrist can save your life.
Medical alert bracelets aren’t just fashion accessories. They’re life-saving tools designed to communicate critical drug information when you can’t. In emergencies, every second counts. And according to a 2022 study in the Journal of Emergency Medicine, nearly 37% of ER errors involve medications. That’s not a small risk. It’s a preventable one.
Why Drug Safety Is the #1 Reason People Wear These Bracelets
Most people think medical alert bracelets are for diabetes or heart conditions. And yes, those matter. But the real game-changer? Drug safety.
Take blood thinners. Over 2.9 million Americans take warfarin or similar drugs. If you’re bleeding out after a fall, giving you a clot-busting drug could kill you. But if the ER team sees “ON BLOOD THINNERS” on your wrist, they pause. They adjust. They choose safer options.
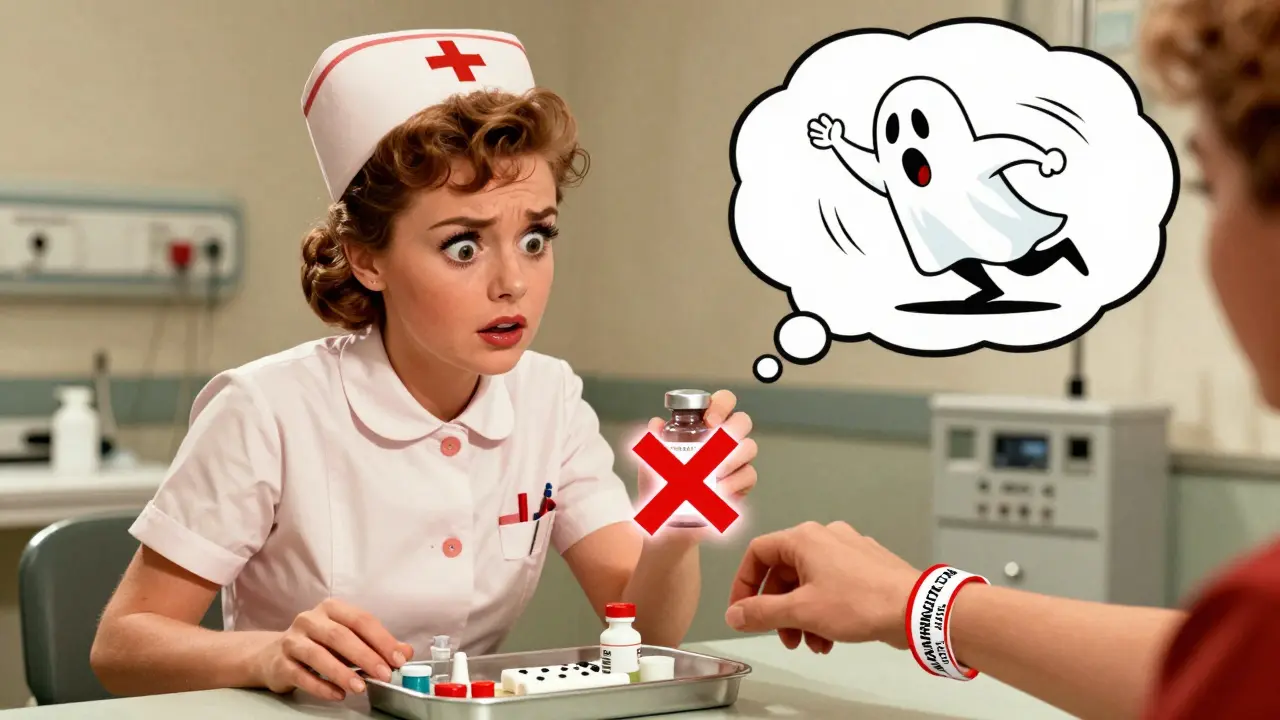
Same goes for allergies. Penicillin affects 1 in 10 people in the U.S. If you’re allergic and end up in the ER with an infection, a nurse might instinctively reach for it. But if your bracelet says “ANAPHYLACTIC TO PENICILLIN,” that mistake stops before it starts. One Reddit user, ‘AllergicAmy,’ shared how her bracelet stopped doctors from giving her penicillin during an appendectomy. She wrote: “They were seconds away. I’d have died.”
It’s not just allergies and blood thinners. NSAIDs like aspirin or ibuprofen can trigger dangerous reactions in people with asthma or kidney disease. Sedatives can cause respiratory failure in those with sleep apnea. These aren’t rare cases. They’re routine in ERs-unless the information is right there on your wrist.
What Should Actually Be on Your Bracelet?
Not everything matters equally. First responders don’t have time to read a novel. They’re trained to look for one thing: what could kill you right now.
The American College of Emergency Physicians (ACEP) has clear priorities:
- Drug allergies - List the exact drug, not just “allergic to antibiotics.” Write “ANAPHYLACTIC TO PENICILLIN,” not “allergy.”
- Critical medications - Blood thinners (warfarin, rivaroxaban), insulin, seizure meds, or drugs that affect anesthesia.
- Chronic conditions - Type 1 vs. Type 2 diabetes, heart failure, epilepsy. These guide treatment choices.
Space is limited on traditional metal bracelets. Most hold only 3-5 items. So pick wisely. “Diabetic” isn’t enough. “DIABETIC - INSULIN DEPENDENT” is. “ON BLOOD THINNERS” is vague. “ON RIVAROXABAN 20MG DAILY” is precise.
Here’s what real users have learned the hard way:
- A man with atrial fibrillation wore “ON BLOOD THINNERS” - but the ER didn’t know which one. They ran extra tests, delaying treatment.
- A woman with severe latex allergy didn’t include it. She went into surgery and had a reaction. She’s fine now-but she regrets not listing it.
Accuracy beats completeness. One clear, correct detail is worth five vague ones.
Traditional vs. QR Code Bracelets: Which One Actually Works Better?
There are two main types: engraved metal and QR code.
Traditional bracelets are durable, waterproof, and trusted by first responders worldwide. They’re the gold standard. But space is tight. You can’t fit your full medication list.
QR code bracelets changed the game. Scan the code, and you get a full digital profile: every drug, dosage, pharmacy, doctor, and even your emergency contacts. MedicAlert Foundation launched these in 2018. Now, over 4 million people use them globally.
Here’s the catch: QR codes only work if the profile is updated. And that’s where most people fail.
A 2024 study by the American Pharmacists Association found that 35% of users never update their bracelet info after changing meds. That’s worse than having no bracelet at all. If your bracelet says you’re on warfarin but you switched to apixaban last month? You’re at risk.
That’s why newer systems like MedicAlert’s SmartProfile (launched Jan 2024) sync with pharmacy databases. When your doctor changes your prescription, the bracelet updates automatically. No manual work. No forgotten updates.
For most people, a QR bracelet with auto-sync is the smartest choice. For those who prefer simplicity or live in areas with poor cell service, a well-written engraved bracelet still saves lives.
Who Needs One the Most?
You don’t have to be old or sick to need one. But certain groups are at higher risk:
- People on blood thinners - 41% of them wear one, and for good reason. A single wrong drug can cause internal bleeding.
- Those with severe allergies - Especially penicillin, latex, or sulfa. One reaction can be fatal.
- Diabetics on insulin - Mistaking Type 1 for Type 2 can lead to deadly glucose or insulin errors.
- People on multiple prescriptions - If you take five or more meds, the chance of a dangerous interaction rises fast.
- Those with cognitive issues - Dementia, Alzheimer’s, or brain injuries can leave you unable to speak during a crisis.
The National Council on Aging found that 73% of medical ID-related emergencies happen when people are away from home. Traveling. Working. Shopping. That’s when you’re most vulnerable.
What Happens When It’s Used?
First responders are trained to check wrists and necks within seconds of arriving at a scene. According to the ACEP, they’re taught to look for medical IDs as part of their standard protocol.
And it works. A 2023 study by MobileHelp tracked 142 cases where medical alert bracelets directly prevented fatal drug interactions. In 89% of cases where the bracelet was present and readable, responders used the info correctly.
One ER nurse in Chicago told a patient: “Your bracelet told us not to give you morphine. We would’ve given you 10mg. You’re on a drug that makes you stop breathing with opioids. You’re alive because you wore this.”
But it’s not perfect. A 2023 JAMA Internal Medicine review found that 19% of bracelets had outdated or incomplete info. That’s why accuracy matters more than having one.

Cost, Support, and Keeping It Up to Date
Traditional engraved bracelets start at $49.99. QR code versions start at $69.99, but they require an annual membership-usually $59.99-to keep your digital profile active. Some systems, like Medical Guardian’s 2025 model, bundle the bracelet with 24/7 monitoring for $29.95/month.
Customer service varies. MedicAlert scores 4.3/5 in J.D. Power’s 2024 study. Smaller brands? Around 3.1/5.
Here’s the secret to making this work: Set a reminder. Every time your meds change-whether it’s a new prescription, a dosage bump, or a drug you stopped-update your bracelet. Use your phone calendar. Set a quarterly alert. Or pick a date-like your birthday or the first of the month-and make it a habit.
And if you’re using a QR bracelet with auto-sync? Make sure your pharmacy and doctor are linked to the system. That’s the only way it stays accurate without you lifting a finger.
The Bigger Picture: Why This Isn’t Just About You
Medical alert bracelets are part of a larger shift in healthcare. The 2022 CARES Act now requires ERs to check for medical IDs. Hospitals like Johns Hopkins and Mayo Clinic now include ID verification in their intake checklists.
The FDA is pushing for standardized formatting. Epic and Cerner, the two biggest hospital EHR systems, are building APIs to auto-update medical IDs when your prescriptions change.
This isn’t just a personal safety tool. It’s becoming part of the system. And the more people wear them, the more hospitals will adapt.
Right now, only 14% of EMTs get formal training on reading medical ID info. That’s changing. But until it’s universal, your bracelet is your best defense.
It’s not about fear. It’s about control. You can’t control when an accident happens. But you can control whether your body’s story gets told when you can’t speak.
Do medical alert bracelets really work in emergencies?
Yes. First responders are trained to check for them. Studies show they’re used correctly in 89% of cases where the info is clear and readable. In one 2023 study, 142 life-threatening drug errors were prevented because of these bracelets.
Can I just write my info on a piece of paper instead?
No. Paper gets lost, wet, or torn. First responders don’t search pockets or bags during emergencies-they look at wrists and necks. A bracelet is visible, durable, and instantly recognizable. It’s the only reliable option.
What if I have multiple allergies or medications?
Prioritize. List the top 3-5 items that could kill you if ignored: severe allergies, blood thinners, insulin dependence. Use a QR code bracelet to store the full list. Traditional bracelets have limited space-don’t try to fit everything. Clarity beats completeness.
Are QR code bracelets reliable if my phone dies or I have no signal?
The QR code itself doesn’t need a signal. It’s printed on the bracelet. First responders scan it with a phone or tablet they carry. As long as the device is charged and the code is legible, they can access your profile-even without your phone.
How often should I update my medical alert bracelet?
Every time your meds change. That means after every doctor visit, pharmacy refill, or dosage adjustment. Set a quarterly reminder. If you use a QR bracelet with auto-sync, link it to your pharmacy-then you don’t have to remember.
Are medical alert bracelets covered by insurance?
Most insurance plans don’t cover them. But some Medicare Advantage plans and HSA/FSA accounts allow reimbursement. Check with your provider. Even without coverage, the cost is under $70 for a basic model-far less than the cost of an emergency error.










Okay, I just got my first medical bracelet last week after my dad had that near-miss in the ER. I thought it was overkill until I read this. Now I’m crying a little? Like, I never realized how much we rely on people being able to talk for us. My bracelet says ‘ANAPHYLACTIC TO PENICILLIN & SULFA’ and ‘DIABETIC - INSULIN DEPENDENT’ - short, sharp, no fluff. I feel like I finally have a voice when I can’t speak. Thank you for writing this. 🥹
OMG I’m from Delhi and I just showed this to my mom who’s 72 and on five meds. She’s like, ‘Beta, why would I wear metal? People will think I’m sick!’ But then I told her about the woman who almost died because they gave her penicillin. She paused. Then she said, ‘Fine. Buy me the QR one. But make it pretty.’ I cried. Not because it’s sad - because it’s so simple and nobody talks about it. We need to normalize this. Like, it’s not a badge of illness. It’s a badge of smart living. 💪❤️
So let me get this straight - you’re telling me that in 2025, the only way to not die because a nurse can’t read your handwriting on a sticky note is to buy a $70 accessory? 🤦♂️ I love that we’ve turned basic human safety into a lifestyle brand. Next up: ‘I survived a heart attack’ merch and ‘My insulin pump is a status symbol’ TikTok trends. But honestly? I’m getting one. Because I don’t want to be the guy who dies because I thought ‘I’ll remember to tell them’ - and then I didn’t. 😅
89% success rate sounds good until you realize 19% of bracelets have outdated info. That means nearly 1 in 5 people are walking around with false confidence. This isn’t safety. It’s placebo safety. And the auto-sync QR systems? They’re just corporate surveillance wrapped in a silver band. You think you’re protected? You’re just feeding your data to a subscription model that’ll charge you $60 a year to remind you not to die. How progressive.
I just want to say thank you for this. I’ve been on blood thinners for 8 years and never wore a bracelet because I thought ‘I’m fine, I’ll just tell them.’ Then I had a fall in a parking lot, hit my head, and woke up in the ER with a nurse saying, ‘We almost gave you tPA.’ I didn’t even know what that was. My mom had to scream from the waiting room, ‘He’s on rivaroxaban!’ I didn’t know how to say it. Now I have a bracelet. Simple. ‘ON RIVAROXABAN 20MG.’ No drama. Just facts. And I’m so glad I listened.
Y’all. I’m a 24-year-old with asthma and I take 6 meds. I used to think medical bracelets were for grandmas. Then I got hospitalized for a bad flare-up and the nurse asked, ‘Any allergies?’ I said, ‘I think I’m allergic to something…’ and she looked at me like I was from another planet. I got the QR one with auto-sync. It’s pink. It says ‘ASTHMA - NO NSAIDS - ON SINGULAIR.’ I feel like a superhero now. And I told my whole family to get one. No more guessing games. 💖
I’m from Kolkata. My aunt wears one. She’s diabetic and on warfarin. She says she doesn’t wear it for herself - she wears it so that if something happens on the bus or in the market, someone won’t panic. She says, ‘If I’m silent, let this speak.’ I think that’s the most beautiful thing I’ve heard all year.
QR codes are cool but what if the scanner is broken? Or the battery dies? Or the hospital doesn’t have a phone? The metal one doesn’t need tech. It just needs eyes. Keep it simple. Keep it visible. Keep it right.
So we’ve turned medical safety into a consumer product because the healthcare system failed us? Cool. I get it. But let’s not pretend this is a fix. It’s a Band-Aid on a hemorrhage. You wear a bracelet because you don’t trust the system to listen. And that’s the real tragedy. Not the bracelet. The fact that we need it.
The systemic failure of pharmacovigilance in the U.S. healthcare infrastructure is epitomized by the commodification of patient self-advocacy via wearable medical identification devices. The reliance on individualized, non-interoperable, subscription-based QR code platforms reflects a neoliberal displacement of institutional responsibility onto the patient-consumer, thereby exacerbating health inequities among marginalized populations who lack access to premium digital health services.
Interesting that the 2024 study showed 35% of QR users don’t update. But here’s the kicker - 72% of those users never even knew they needed to. The problem isn’t the tech. It’s the lack of patient education. We need mandatory counseling at pharmacy pickup. Not a bracelet. A conversation.
My cousin got a bracelet after her stroke. She’s 38. She has atrial fibrillation and takes apixaban. She got it because she didn’t want to be the reason someone gave her aspirin. She said, ‘I don’t want to be the reason someone’s life ends because they didn’t know.’ I cried. Then I got one too. ‘ON APIXABAN 5MG.’ That’s it. That’s all it needs to be.
I have a bracelet. It says ‘ALLERGIC TO PENICILLIN.’ I’ve never needed it. But I wear it anyway. Because one day, I might be unconscious. And I want someone to know.
So we’re telling people to spend money on a bracelet because the ER can’t read a chart? That’s not safety. That’s a failure of EHR integration. If your hospital can’t pull up your med list from Epic, why are you asking me to buy a shiny ring? This is capitalism fixing its own broken systems with consumer guilt.