Stress & Dermatitis Tracker
How stressed do you feel today? Select a number from 1 to 10:
Click "Track My Symptoms" to see your personalized insights.
Ever notice a rash popping up right after a tough day at work or a sleepless night? You’re not imagining it - stress and dermatitis are tightly linked, and the connection can turn a minor itch into a full‑blown flare‑up. Below you’ll learn why the mind‑body bridge matters for skin health and get practical steps to keep those red patches at bay.
Key Takeaways
- Stress triggers hormonal changes, especially cortisol, that weaken the skin barrier and boost inflammation.
- Both atopic and contact dermatitis are especially sensitive to emotional stress.
- Daily habits - sleep, nutrition, mindfulness, and gentle skin care - can dramatically lower flare‑up frequency.
- When home strategies aren’t enough, early medical intervention prevents chronic damage.
- Tracking stress levels alongside skin symptoms helps you spot patterns and act faster.
Understanding the Link Between Stress and Dermatitis
Stress is the body’s physiological response to perceived threats or pressures, releasing hormones like cortisol and adrenaline. While short‑term stress can be useful, chronic activation throws off the delicate balance of the immune system and the skin’s protective barrier.
Dermatitis refers to inflammatory skin conditions that cause redness, itching, and sometimes oozing; common forms include atopic, contact, and seborrheic dermatitis. Inflammation is the core symptom, and stress‑induced hormones act as a catalyst, amplifying that inflammation.
Research from the National Institute of Dermatology (2023) showed that patients reporting high stress scores were 2.4 times more likely to experience a dermatitis flare in the following month. The body’s “fight‑or‑flight” chemistry skews the immune response toward a Th2‑dominant profile, which is exactly what fuels many eczema‑type rashes.
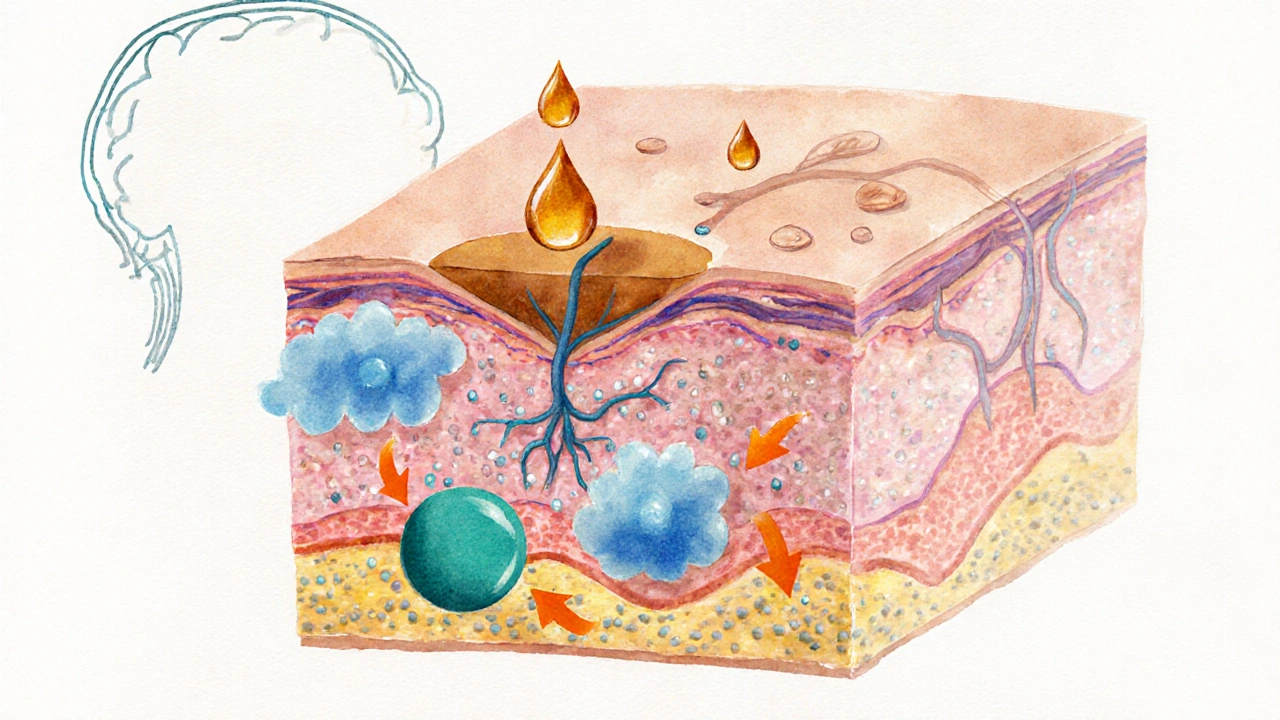
How Stress Physiology Messes With Your Skin
Three biological pathways bridge stress and skin irritation:
- Cortisol overload: Elevated cortisol reduces production of ceramides - the lipids that keep the skin barrier waterproof. A leaky barrier lets irritants and allergens slip through, sparking an immune reaction.
- Neuro‑inflammation: Stress activates the brain’s mast cells, which release histamine and other pro‑inflammatory mediators directly onto skin nerves, intensifying itching.
- Immune dysregulation: Chronic stress tilts the balance toward Th2 cells, which release interleukin‑4 (IL‑4) and interleukin‑13 (IL‑13), cytokines known to worsen atopic dermatitis.
Because these mechanisms overlap, even a mild anxiety spike can translate into an itchy, red patch within hours.
Which Types of Dermatitis React Most to Stress?
| Dermatitis Type | Typical Triggers | Stress Impact | Key Management Tip |
|---|---|---|---|
| Atopic Dermatitis (Eczema) | Allergens, dry skin, genetics | High - stress amplifies itch‑scratch cycle | Moisturize twice daily, practice mindfulness |
| Contact Dermatitis | Irritants, chemicals, metals | Moderate - stress lowers barrier, so irritants penetrate easier | Identify and avoid triggers, use barrier creams |
| Seborrheic Dermatitis | Malassezia yeast, oily skin | Low to moderate - stress may increase oil production | Antifungal shampoos, keep scalp clean |
| Psoriasis (though not classic dermatitis) | Autoimmune, genetics | High - stress can trigger new plaques | Phototherapy, systemic meds, stress‑reduction programs |
Notice the pattern? Atopic and contact dermatitis are the most stress‑sensitive, so they’re the best places to start when you’re looking to cut flare‑ups.
Practical Tips to Reduce Dermatitis Flare‑Ups
Below is a step‑by‑step routine you can embed into a busy day. Each item targets one of the three stress‑skin pathways described earlier.
- Track stress and skin logs: Use a simple notebook or phone app to note stress levels (1‑10) and any skin changes. Patterns emerge faster than you think.
- Prioritize sleep: Aim for 7-9 hours. Sleep deprivation spikes cortisol by up to 30%, directly weakening the skin barrier.
- Adopt a skin‑friendly diet: Include omega‑3 rich foods (salmon, walnuts) and antioxidants (berries, leafy greens). Studies link these nutrients to lower IL‑4 production.
- Hydrate the barrier: Apply a fragrance‑free ceramide‑based moisturizer within three minutes of showering. This restores lipids lost to cortisol.
- Practice brief mindfulness breaks: Even five minutes of deep breathing reduces cortisol by roughly 15% (Harvard Health, 2022). Try box breathing: inhale 4 sec, hold 4 sec, exhale 4 sec, hold 4 sec.
- Gentle cleansing: Use lukewarm water and a pH‑balanced, sulfate‑free cleanser. Hot water strips natural oils, making the barrier more vulnerable.
- Limit alcohol and caffeine: Both can aggravate dehydration and increase stress hormones.
- Use anti‑itch tools wisely: Cool compresses, colloidal oatmeal baths, or over‑the‑counter hydrocortisone (1%) for short‑term relief. Avoid frequent steroid use; it can thin skin over time.
Stick with these habits for at least two weeks before judging effectiveness - the skin’s recovery cycle isn’t instantaneous.
Lifestyle Shifts That Keep Stress in Check
Beyond daily skin care, broader lifestyle choices shape how your body reacts to stress.
- Regular physical activity: Moderate exercise (30 minutes, 4-5 times a week) lowers baseline cortisol and boosts endorphins, which naturally calm itching.
- Social support: Talking with friends or joining a support group reduces perceived stress by up to 40% (Psychology Today, 2024).
- Digital detox: Constant news scrolling spikes anxiety. Set a “no‑screen” hour before bedtime to improve sleep quality.
- Mind‑body therapies: Yoga, tai‑chi, and progressive muscle relaxation have documented benefits for eczema severity.
These changes don’t replace medical treatment, but they create a less hostile environment for your skin.

When to Seek Professional Help
If you notice any of the following, it’s time to call a dermatologist or your primary care provider:
- Flare‑ups covering more than 10% of body surface area.
- Painful cracks, bleeding, or signs of infection (pus, fever).
- Symptoms persisting despite consistent skin‑care and stress‑reduction for four weeks.
- Unexplained darkening or thickening of the skin (lichenification).
Professional options include prescription‑strength topical steroids, calcineurin inhibitors, or even systemic therapies like dupilumab for severe atopic dermatitis. Early intervention can prevent the chronic itching‑scratch cycle that leads to permanent skin changes.
Putting It All Together: A Sample 7‑Day Reset Plan
Use the table below as a cheat‑sheet. Adjust times and foods to fit your schedule, but keep the core actions intact.
| Day | Morning | Afternoon | Evening |
|---|---|---|---|
| 1 | Morning stretch + 10‑min box breathing; gentle cleanser + ceramide moisturizer | Walk 20min; log stress level; snack on walnuts | Digital detox 1hour before bed; oatmeal bath; journal skin notes |
| 2 | Yoga flow (15min); apply moisturizer | Hydrating lunch (salmon salad); short walk; note any itch | Warm shower <90°F; cool compress on itchy spots; read a book |
| 3 | Deep breathing (5min); fragrance‑free cleanser | Meet friend for coffee (limit caffeine); log stress 3/10 | Progressive muscle relaxation; apply hydrocortisone if needed |
| 4 | Light jog (20min); moisturize | Protein‑rich lunch; quick skin check | Screen‑free hour; oatmeal bath; update journal |
| 5 | Tai‑chi (15min); gentle cleanser | Snack on berries; review stress‑skin log for patterns | Warm shower; cool compress; early bedtime |
| 6 | Box breathing + moisturizer | Outdoor activity; hydrate well | Digital detox; calming music; apply barrier cream |
| 7 | Reflective journaling; moisturize | Plan next week’s stress‑reduction actions | Full night of 8‑hour sleep; celebrate skin improvement |
After a week, compare your stress scores to the skin notes. If itching dropped by at least 30%, you’ve found a winning formula. If not, tweak one variable at a time - maybe add a probiotic or try a different moisturizer.
Frequently Asked Questions
Can stress cause new dermatitis, or only worsen existing skin conditions?
Stress alone rarely creates a brand‑new dermatitis type, but it can trigger the first visible flare in people who are predisposed. The hormonal surge weakens the skin barrier, making it easier for allergens or irritants to ignite a rash.
Is there a specific cortisol level that predicts a flare‑up?
No single cutoff exists, but studies show that salivary cortisol above 0.2µg/dL in the evening correlates with a 45% rise in eczema activity. Monitoring through a simple home test can give you a rough idea of your personal threshold.
Do antihistamines help when stress‑related itching occurs?
They can provide short‑term relief because histamine is part of the itch pathway activated by stress. However, antihistamines don’t address the underlying barrier dysfunction, so they’re best used alongside moisturizers and stress‑reduction techniques.
How long does it usually take to see skin improvement after reducing stress?
Most people notice a decrease in itching and redness within 7-14days of consistent sleep, diet, and mindfulness. Full barrier repair may take 3-4weeks, especially for chronic atopic dermatitis.
Are there any natural supplements that support skin health under stress?
Omega‑3 fish oil, vitamin D3 (especially in winter months), and probiotic strains such as Lactobacillus rhamnosus have shown modest reductions in eczema severity by modulating immune responses and strengthening the barrier.









I totally get it, stress can really mess with your skin 😔💖
Cortisol surges during stress act like a double‑edged sword, breaking down the lipid matrix that keeps our skin barrier intact. When that barrier is compromised, irritants slip through like unwanted guests at a party. The immune system, sensing these intruders, releases histamines that intensify the itch‑scratch cycle. Moreover, chronic stress skews T‑helper cell differentiation toward a Th2 profile, which is a known driver of atopic dermatitis. Studies have shown that individuals with persistently high perceived stress scores experience flare‑ups up to 2.4 times more often than their low‑stress counterparts. This is not merely anecdotal; randomized trials measuring cortisol levels correlate spikes with measurable increases in skin erythema. The neuro‑inflammatory pathway also plays a role: mast cells in the dermis degranulate under adrenergic stimulation, releasing more inflammatory mediators. Consequently, even a mild anxiety episode can manifest as a red, burning patch within hours. Nutrition compounds the picture, as stress‑induced gut dysbiosis can reduce short‑chain fatty acid production, further weakening barrier repair. Sleep deprivation, another stressor, elevates cortisol by roughly 30 % and reduces growth hormone, which is essential for skin regeneration. Physical activity, paradoxically, can both lower baseline cortisol and, if excessive, increase skin temperature and sweat, a potential irritant for contact dermatitis. Therefore, a balanced approach is crucial: manage stress, protect the barrier, and monitor lifestyle factors. Simple interventions like mindful breathing have been demonstrated to cut cortisol output by about 15 % in controlled settings. Applying a ceramide‑rich moisturizer within three minutes of bathing restores lipids lost during the cortisol surge. Finally, when home measures fail, early consultation with a dermatologist can prevent chronic remodeling of the skin architecture. In summary, the cascade from mind to skin is a chain of biochemical events that can be interrupted at multiple points with the right strategies.
Wow, this guide is a game‑changer! I’ve tried a few of these tricks, like the 5‑minute box breathing, and my eczema calms down almost instantly. Pairing it with a good moisturizer right after a shower really locks in the skin’s moisture. Keep these tips coming, we need more skin‑savvy hacks! 🙌
Stop ignoring the barrier repair step; a fragrance‑free ceramide cream is non‑negotiable if you want any real improvement. Also, ditch the hot showers – they strip lipids faster than you can say “flare‑up”.
The battle between my mind and my skin feels like a raging storm!
Great breakdown! 🌟 Adding a quick journal entry each evening can help you spot the stress‑flare pattern even faster. And don’t forget to hydrate – water supports barrier function from the inside out. 👍
In many traditional societies, the connection between emotional equilibrium and skin health has been acknowledged for centuries, long before modern biochemistry attempted to quantify cortisol or interleukins. For example, Ayurvedic practitioners speak of “ojas” – the vital essence that, when depleted by mental turbulence, manifests as external blemishes and irritations. Similarly, ancient Chinese medicine emphasizes the liver’s role in allowing emotions to flow freely; stagnation is believed to cause “heat” that erupts on the surface as dermatitis. These holistic viewpoints align surprisingly well with contemporary research showing that psychological stress can compromise the stratum corneum, the outermost layer of the epidermis, thereby inviting pathogenic assaults. While Western dermatology often prescribes topical steroids as a first line, integrating practices such as mindfulness meditation, herbal teas, or gentle yoga can address the root cause rather than merely treating the symptom. Moreover, dietary customs that favor omega‑3 rich fish, fermented foods, and antioxidant‑laden fruits have been shown to modulate inflammatory pathways, echoing the wisdom embedded in traditional diets. It is also noteworthy that community support – the shared storytelling around skin struggles in many cultures – provides an emotional buffer that reduces perceived stress levels, which in turn can lessen flare‑ups. Thus, bridging the gap between time‑tested cultural remedies and evidence‑based medicine may offer a more comprehensive strategy for those battling chronic dermatitis. By honoring both the scientific and the cultural narratives, we empower patients to take ownership of their skin health in a manner that respects their heritage and their modern lifestyle. Ultimately, the synthesis of ancient insight and modern science creates a richer tapestry of care that benefits both mind and skin.
The analysis presented correctly identifies cortisol’s role in barrier disruption, yet it overlooks the contribution of neuropeptide substance P, which also potentiates mast cell degranulation. Furthermore, the recommendation to log stress levels lacks methodological rigor; a validated scale such as the Perceived Stress Scale would enhance data reliability. The suggested dietary interventions are sound, but the claim regarding omega‑3 reduction of IL‑4 requires citation of specific randomized controlled trials. In sum, the article provides a solid foundation but would benefit from deeper mechanistic citations and standardized assessment tools.
Excellent points-especially on substance P!; Adding a validated stress questionnaire is a must; and citing RCTs will strengthen the argument. 👍
Bottom line: combine barrier repair, stress tracking, and early dermatologist visits, and you’ll slash flare‑ups for good.