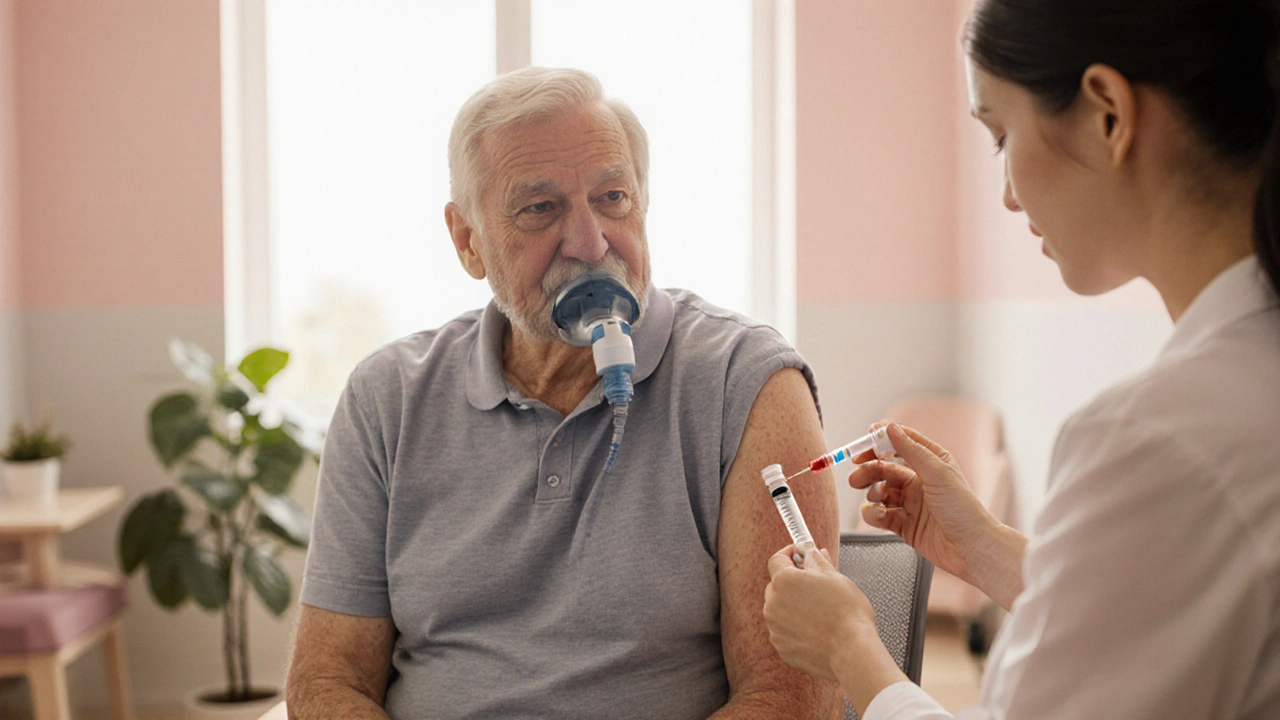
COPD Vaccine Recommendation Checker
Your Vaccine Recommendations
Key Points to Remember:
- Annual flu vaccination is strongly recommended for all COPD patients
- Pneumococcal vaccines are critical for preventing serious bacterial pneumonia
- COVID-19 vaccination is essential for protecting against severe illness
- Keep a record of all vaccinations and discuss with your healthcare team
When managing Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition that limits airflow, staying ahead of infections becomes a daily battle. Respiratory viruses and bacteria can trigger sudden worsening called COPD exacerbation, often landing patients in the emergency department. The good news? Proven vaccinations for COPD patients dramatically cut that risk.
Quick Take
- Flu, pneumococcal, and COVID‑19 shots are the three vaccines most strongly recommended for COPD.
- Vaccination reduces COPD‑related hospital stays by 30‑50% in most studies.
- Guidelines from the Global Initiative for Chronic Obstructive Lung Disease (GOLD) call for annual flu shots and at least one pneumococcal series.
- Side‑effects are usually mild-sore arm, low‑grade fever, or brief fatigue.
- Talk to your clinician, keep a vaccination record, and schedule boosters ahead of flu season.
How Vaccines Shield the Lungs
Respiratory infections hit COPD patients harder because the airways are already narrowed and inflamed. When a virus like influenza lands on the irritated lining, it can trigger a cascade: increased mucus, bronchospasm, and a drop in oxygen exchange. The body’s immune response then adds inflammation, further compromising airflow. A vaccine works by teaching the immune system to recognize the culprit without suffering the full infection. That pre‑armed defense either prevents the disease outright or blunts its severity, keeping the lungs from spiraling into an acute exacerbation.
Vaccines Every COPD Patient Should Have
Below is the core set of shots endorsed by the GOLD guidelines, the American Thoracic Society, and major public‑health agencies.
| Vaccine | Typical Schedule | Main Benefit for COPD |
|---|---|---|
| Influenza (flu) vaccine | Annually, before flu season (usually September‑October) | Prevents flu‑triggered exacerbations; cuts hospitalizations by ~40% |
| Pneumococcal vaccine (PCV13 then PPSV23) | PCV13 once, followed by PPSV23 ≥8 weeks later; booster every 5‑10years | Reduces bacterial pneumonia, a leading cause of COPD death |
| COVID‑19 vaccine | Primary series + booster every 6‑12months, per national guidance | Stops severe COVID‑19, which can cause prolonged lung injury |

Evidence: Numbers That Matter
Large‑scale cohort studies from the United States, Europe, and Asia consistently show the impact of immunization on COPD outcomes. One 2023 review of 12clinical trials found:
- Annual flu vaccination cut the risk of COPD exacerbation by 30‑45%.
- Patients who received both PCV13 and PPSV23 experienced a 38% reduction in pneumonia‑related admissions.
- COVID‑19‑vaccinated COPD cohorts had a 55% lower odds of intensive‑care admission compared with unvaccinated peers.
These figures translate into real‑world savings: fewer emergency‑room trips, less time on steroids, and a better quality of life.
Common Concerns-and the Facts
It’s natural to wonder whether a weakened immune system makes vaccines risky. The truth is that most COPD patients have a normal ability to generate protective antibodies, especially when disease‑modifying therapies are optimized.
- Mild side‑effects: pain at the injection site, low‑grade fever, or muscle aches; they resolve within 48hours.
- Severe reactions: anaphylaxis is exceedingly rare (<1 per million doses) and clinics are prepared to manage it.
- Contraindications: severe allergic reaction to a previous dose or to any vaccine component (e.g., egg protein for some flu shots).
If you’re on chronic steroids or immunosuppressants, discuss timing with your provider; sometimes a short pause in medication can improve vaccine response without compromising COPD control.
Practical Steps: From Doctor’s Office to Pharmacy
- Make a list. Write down the three core vaccines and any local boosters (e.g., shingles if you’re over 50).
- Check your records. Your pulmonologist or primary‑care chart often notes which shots you’ve already received.
- Schedule ahead. Aim for the flu shot in early September; pneumococcal series can be administered anytime but many clinics bundle it with the annual flu visit.
- Ask about formulation. High‑dose or adjuvanted flu vaccines may offer better protection for older adults.
- Keep a vaccination card. Write the date, vaccine type, and lot number. This aids future visits and insurance claims.
Many pharmacies now offer walk‑in appointments, and several health‑plan apps let you book directly with your local clinic. If transportation is a barrier, community health programs often provide mobile immunization units.
Checklist for COPD Patients
- ✅ Confirm annual flu vaccine before November.
- ✅ Verify pneumococcal series (PCV13→PPSV23) completed; schedule booster if >5years since last dose.
- ✅ Stay current on COVID‑19 boosters per national schedule.
- ✅ Discuss any new medications (e.g., long‑term steroids) with your doctor before vaccination.
- ✅ Keep a personal vaccination record and share it with every healthcare provider.

Frequently Asked Questions
Can I get the flu shot if I’m already on inhaled steroids?
Yes. Inhaled steroids do not interfere with the flu vaccine’s ability to spark an immune response. In fact, getting vaccinated can reduce the need for higher‑dose oral steroids during an exacerbation.
What if I miss the annual flu vaccine?
A late flu shot still offers protection, especially against severe disease. Aim to get it as soon as the pharmacy stocks the current season’s formulation, even if it’s October or November.
Are there any vaccines I should avoid because of COPD?
No routine vaccine is contraindicated for COPD itself. The only exceptions are individual allergic reactions to vaccine ingredients. Discuss any prior reactions with your clinician.
How often should the pneumococcal vaccine be repeated?
After the initial series (PCV13 then PPSV23), a booster of PPSV23 is recommended every 5years for high‑risk patients, including those with moderate‑to‑severe COPD.
Do the vaccines interfere with my COPD medications?
Vaccines are safe alongside most COPD drugs. If you’re on a short course of oral steroids, your doctor may advise a brief pause to maximize antibody production, but routine inhalers and bronchodilators pose no issue.








Vaccines are a key part of keeping COPD under control. Getting the flu shot each year cuts down on flare‑ups, and the pneumococcal series helps stop bacterial pneumonia, which is one of the biggest risks for us.
If you think skipping the flu jab is okay, you’re ignoring the data that shows a 40% drop in hospital visits for COPD patients who get vaccinated.
Hey folks 😊, just wanted to add that staying on top of the three main shots-flu, pneumonia and COVID-really eases the day‑to‑day for anyone with COPD. The flu vaccine alone can shave off almost half of the seasonal exacerbations, which means fewer steroids and doctor trips. Pneumococcal shots are a bit more involved (PCV13 then PPSV23), but they protect against the nasty bacterial pneumonia that can be fatal. And yes, the COVID‑19 boosters are still recommended because the virus can cause long‑lasting lung damage even in vaccinated people. Keep a vaccination log, set reminders, and talk to your pulmonologist about the timing. It’s a small routine that pays big dividends for breathing easier. 🌟
Behold, the relentless siege upon the compromised airways of a COPD patient; each viral invader is a marauding legion, and the only armor we possess is vaccination. The influenza inoculation stands as a bastion against seasonal onslaughts, while the pneumococcal preparation fortifies the lungs against invasive bacterial assaults. Even the COVID‑19 vaccine, a modern marvel, shields the fragile respiratory frontier from catastrophic collapse. Neglecting these defenses is tantamount to surrendering one’s breath to inexorable decline. Therefore, let the schedule be observed with the solemnity of a treaty, lest we invite ruin upon our very exhalations.
I completely agree with the point about flu and pneumococcal shots. It’s also helpful to write down the dates of each dose so you can track when boosters are due. Many clinics offer reminder texts, which can take the guesswork out of scheduling.
Our country’s public‑health program has done a solid job rolling out flu and COVID vaccines, and we should all support the effort. Skipping your shots isn’t just a personal risk-it undermines the collective defense that keeps our communities strong.
Flu yearly, pneumonia series once, COVID as advised – that’s the simple plan.
Think of vaccination as an investment in the future of your breath. Each dose adds a layer of protection that lets you pursue the things you love-walking the park, playing with grandchildren, or simply enjoying a deep sigh without fear. The numbers don’t lie: fewer exacerbations mean more quality time. So treat your vaccine appointments like any other rehearsal for a better performance of life.
Vax up, breathe easy, live large – that’s the golden rule for any COPD warrior.
When you line up your flu shot before the season starts, you’re giving yourself a head‑start against triggers. Pair that with the pneumococcal series and the COVID boosters, and you’re building a solid shield. Keep that schedule in your phone calendar and you’ll stay ahead of the curve.
It is worth taking a moment to reflect on the broader public‑health context within which these vaccination recommendations sit, because the statistics cited in the article are not merely abstract figures but outcomes that have been observed across diverse populations over many years. The influenza vaccine, for instance, has consistently demonstrated a reduction in COPD‑related hospitalizations by approximately thirty to forty percent, a figure that emerges from pooled analyses of randomized controlled trials as well as observational cohort studies conducted in both North America and Europe. Equally compelling is the evidence surrounding pneumococcal immunization; the sequential administration of PCV13 followed by PPSV23 not only lowers the incidence of invasive pneumococcal disease but also diminishes the frequency of bacterial pneumonia that often precipitates acute exacerbations in patients with compromised airway clearance. Furthermore, the COVID‑19 vaccines, which were rapidly developed in response to an unprecedented global pandemic, have been shown to decrease intensive‑care unit admissions among COPD patients by more than fifty percent, a benefit that translates directly into reduced exposure to invasive monitoring and mechanical ventilation. From a mechanistic standpoint, each of these vaccines operates by priming the adaptive immune system to recognize specific antigens, thereby enabling a swifter and more efficient neutralizing response upon actual pathogen encounter; this pre‑emptive immunological training is especially valuable for individuals whose baseline pulmonary reserve is already limited. In addition to the clinical efficacy data, one must also consider the safety profile, which remains overwhelmingly favorable, with most adverse events limited to mild injection‑site discomfort and transient low‑grade fever. The tolerability of vaccines, even in older adults with multiple comorbidities, reinforces the argument for universal uptake among the COPD community. Moreover, adherence to vaccination schedules can be facilitated through systematic reminders, integrated electronic health records, and coordinated care pathways that align primary‑care visits with immunization opportunities. Health‑care providers are encouraged to engage patients in shared decision‑making, explaining both the quantitative benefits and the practical steps required to maintain up‑to‑date protection. Ultimately, the cumulative impact of these prevention strategies is a measurable reduction in health‑care costs, fewer lost work days, and an enhanced quality of life for patients who can remain active and independent for longer periods. As such, the guideline recommendations are not merely advisory but constitute a cornerstone of comprehensive COPD management. By internalizing these principles and acting on them consistently, patients can significantly alter the trajectory of their disease. This proactive approach embodies the very essence of modern, evidence‑based medicine. Patients should also discuss any concerns about allergy history with their physicians, as modern formulations have minimal excipient risks. Regular review of vaccination status during pulmonary function visits ensures gaps are identified early. The synergy of immunization with optimal bronchodilator therapy further stabilizes airway inflammation.
Nice rundown, but remember that not everyone can chase every booster like a checklist – life gets busy, and some of us just want the basics without the extra drama 😅.
Sure, because nothing says “I care about my lungs” like lining up for shots on a Tuesday while pretending the flu isn’t already knocking on the door. 🙄
From a systems‑biology perspective, the immunogenic epitopes presented by the polyvalent formulations may induce a state of trained immunity that, paradoxically, could modulate the host’s inflammatory cascade in COPD; however, the heterogeneity of patient phenotypes necessitates a more nuanced risk‑benefit calculus than the blanket recommendations suggest.
While the data are compelling, the article fails to address the cost‑effectiveness analysis that would be crucial for policy makers evaluating large‑scale vaccination programs for COPD cohorts.
lol the whole thing sounds like another pharma push, u sure u trust the src?