Women get sick from medications more often than men - and it’s not because they’re more sensitive.
Every year, millions of women take the same pills as men - same dose, same instructions - and end up in the ER with nausea, dizziness, or worse. Meanwhile, men taking the exact same drug often feel fine. This isn’t coincidence. It’s a systemic failure built into how drugs are tested, approved, and prescribed.
The problem goes back decades. In the 1970s, the FDA told pharmaceutical companies to exclude women of childbearing age from early drug trials. The goal was to protect unborn babies. But the rule stuck. Even after the NIH mandated women’s inclusion in 1993, researchers kept treating male bodies as the default. By 2023, women made up nearly half of clinical trial participants - but only 12% of pharmacokinetic studies even looked at how their bodies processed drugs differently.
What happened? Drugs were dosed for men. And women - who make up 51% of the U.S. population and take 59% of all prescriptions - were left guessing what would happen when they swallowed them.
Biological differences aren’t optional - they’re essential
Women aren’t just smaller men. Their bodies work differently. And those differences change how drugs move through them.
Take liver enzymes. Women have about 40% less CYP3A4 activity than men - the main enzyme that breaks down half of all prescription drugs. That means medications like statins, benzodiazepines, and even some painkillers stay in a woman’s system longer. A standard dose for a man might be too strong for a woman.
Body fat plays a role too. On average, women have 10-12% more body fat than men. Fat-soluble drugs - like diazepam (Valium) - get stored in fat tissue. That means they’re released slowly, lingering in the bloodstream 20-30% longer in women. One study found women cleared lithium 22% slower than men. That’s not a small difference. That’s the difference between a safe dose and a toxic one.
Hormones add another layer. Oral contraceptives can slash the effectiveness of lamotrigine (an epilepsy drug) by up to 60%. During certain phases of the menstrual cycle, drug metabolism can shift by 30%. Yet most prescriptions don’t account for this. Doctors don’t ask when your period started. They just hand you the same pill they gave your brother, husband, or male coworker.
Real drugs. Real consequences.
The numbers don’t lie. Women suffer adverse drug reactions 80-90% more often than men. And it’s not just random. Certain drugs show clear, documented patterns.
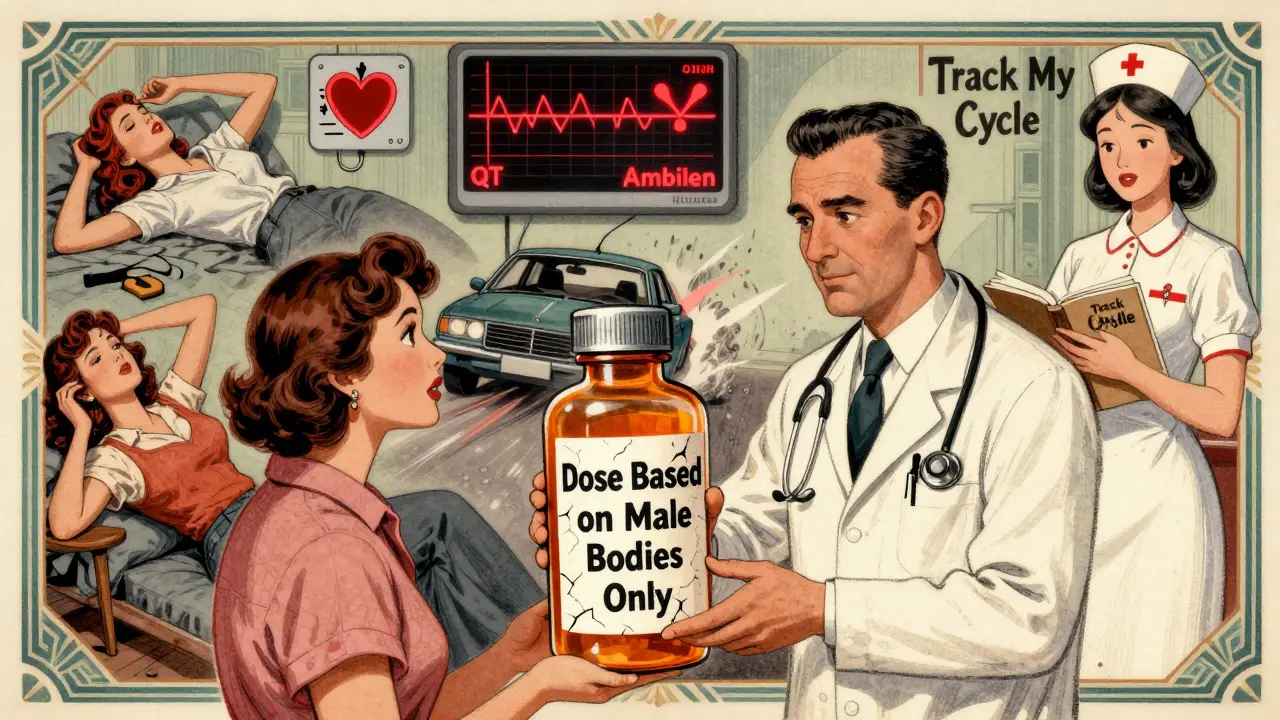
Zolpidem (Ambien) is the poster child. In 2013, the FDA finally acted after years of evidence showing women metabolized the drug 50% slower. The result? Women woke up groggy, drowsy, even impaired - driving while still asleep. The FDA cut the recommended dose for women in half. After the change, adverse event reports from women dropped by 38%.
Digoxin, used for heart failure, builds up to 20-30% higher levels in women at standard doses. That raises the risk of toxicity by 40%. Yet most doctors still prescribe the same dose regardless of sex.
SSRIs like sertraline and fluoxetine cause 1.5-2 times more nausea and dizziness in women. Men? They’re more likely to report sexual side effects - 35% more than women. But women report those too, and they’re often dismissed as "normal" or "just part of the treatment."
Antibiotics like sulfamethoxazole trigger severe skin reactions in women at 47% higher rates. Antipsychotics like haloperidol cause QT prolongation - a dangerous heart rhythm - 2.3 times more often in women.
And it’s not just prescription drugs. Even over-the-counter painkillers like ibuprofen and acetaminophen show sex-based differences in how they’re processed. But you won’t see that on the bottle.
Doctors don’t know - and that’s dangerous
Here’s the kicker: most doctors don’t know this stuff.
A 2022 AMA survey found only 28% of physicians routinely consider sex differences when prescribing common medications. Two out of three didn’t even know about the FDA’s 2013 Ambien dose change for women.
Why? Because medical schools barely teach it. Drug labels rarely mention it. Only 15 of the 200 most commonly prescribed medications in the U.S. have sex-specific dosing instructions. That means 92% of prescriptions are handed out without any sex-based guidance.
And when women report side effects? They’re often told they’re "overreacting," "anxious," or "just sensitive." One woman on Reddit, a nurse with 12 years in the ER, said she’d seen at least twice as many women come in with adverse reactions to standard pain meds. She wasn’t imagining it. The data backs her up.
It’s not just biology - it’s behavior
Not everyone agrees that biology alone explains the gap.
Dr. Sarah Richardson from Harvard analyzed 33 million FDA adverse event reports. When she accounted for the fact that women take 56% more prescriptions than men on average, the sex-based difference in adverse reactions dropped to under 5%. Her point? Women are more likely to notice side effects. They’re more likely to report them. They’re more likely to see doctors.
That doesn’t mean biology doesn’t matter. It means we’re missing part of the picture. Women aren’t just biologically different - they’re also more visible in the system. And that visibility makes their suffering harder to ignore.
Dr. Janine Austin Clayton from the NIH puts it simply: "Biological differences certainly exist, but we must also consider that women are more likely to report symptoms and seek healthcare."
So it’s not either/or. It’s both. Biology creates vulnerability. Behavior amplifies it. And the system ignores both.
What’s being done - and what’s still broken
Change is coming. Slowly.
The FDA launched its "Sex and Gender Roadmap" in 2023, aiming to integrate sex and gender into every part of drug regulation by 2026. The European Medicines Agency now requires sex-stratified data in all Phase III trials. The NIH just invested $12.5 million in a center at Harvard Medical School focused on sex differences in medicine.
Companies like Adyn and Womb Society are building drugs specifically for women’s bodies. The global women’s health pharmaceutical market is growing at 8.7% a year.
But here’s the reality: only 37% of new drug approvals in 2022 included meaningful sex-specific safety or efficacy data. Only 4% of drug labels contain sex-based dosing instructions. And a 2023 study in Nature Medicine found that while 78% of cancer trials track sex, only 32% of heart disease trials do.
Meanwhile, the cost of inaction? Over $30 billion a year in U.S. healthcare spending on preventable adverse drug reactions - 63-70% of which happen to women.
What you can do right now
You don’t have to wait for the system to fix itself.
- Ask your doctor: "Is this dose right for a woman my size?" or "Has this been studied in women?"
- Track your side effects: Use an app or journal. Note timing, symptoms, and your menstrual cycle phase. This data matters.
- Check your prescriptions: Look up your drug on the FDA’s Drug Trials Snapshots. See if sex-specific data is available.
- Speak up: If you feel worse after starting a new drug, don’t assume it’s "normal." Push for a dose review.
There’s no shame in asking. You’re not being difficult. You’re being informed.
The FDA’s dose reduction for Ambien saved lives. It didn’t happen because someone had a good idea. It happened because women kept reporting it. Because researchers kept publishing it. Because someone finally listened.
That’s the model. That’s the path forward.
Frequently Asked Questions
Why are women more likely to have side effects from medications?
Women experience more side effects because their bodies process drugs differently. They have lower levels of key liver enzymes, higher body fat percentages, and hormonal fluctuations that affect how medications are absorbed, metabolized, and cleared. These biological differences, combined with decades of clinical trials focused mostly on men, mean many drugs are dosed too high for women.
What medications have known sex-based dosing differences?
Zolpidem (Ambien) is the most well-known - the FDA cut the dose for women by 50% in 2013. Other drugs with documented differences include digoxin (heart medication), lamotrigine (seizure drug), lithium (mood stabilizer), and some SSRIs like sertraline. Even common painkillers like ibuprofen and acetaminophen show sex-based metabolism differences, though labeling doesn’t reflect this yet.
Are drug companies starting to make gender-specific medications?
Yes, but it’s still rare. Companies like Adyn and Womb Society are developing drugs specifically for women’s physiology. However, they represent less than 0.5% of total pharmaceutical R&D. Most drug development still uses male-dominant models. Regulatory pressure is growing, but change is slow.
Why don’t drug labels mention sex differences more often?
Because the data isn’t required. Until recently, regulators didn’t demand sex-stratified analysis in trials. Even now, only 15 of the 200 most commonly prescribed medications in the U.S. have sex-specific dosing info on the label. Most manufacturers don’t test for it, and without clear evidence, they don’t update the label.
Can I ask my doctor to lower my dose because I’m a woman?
Absolutely. You have the right to ask. Say something like: "I’ve read that women metabolize this drug differently. Could we start with a lower dose to see how I respond?" Many doctors will agree - especially if you’ve had side effects before. Starting low and going slow is always safer.
Is this issue getting better?
Slowly. The FDA’s new roadmap, NIH funding, and global regulatory changes are pushing progress. Studies like UC Berkeley’s JUST Dose project are using AI to build personalized dosing models. But without mandatory requirements, progress will remain uneven. The key is patient advocacy - if enough people demand better data, the system will have to change.









Let’s be real - this isn’t just about biology. It’s about who got to sit at the table when these drugs were first tested. Men. White men. In lab coats. While women were told to "wait their turn" or "be careful with hormones." The fact that we’re only now catching up is a scandal. And it’s not like the data was hidden - it was ignored. Again and again. Until women started dying. Again and again.
I work in pharma. We used to joke that "female subjects" were a liability. Now we’re scrambling to retrofit studies. Pathetic. And expensive. Literally billions in ER visits because no one wanted to do the work.
But hey, at least we’ve got a roadmap now. Too bad it took 50 years of women being told they were "overreacting" to get here.
OMG YES. I took Ambien for a week and woke up making toast at 3am with no memory of it. My roommate had to call me because I was standing in the kitchen in my underwear holding a spatula. I thought I was dreaming. Turns out? I wasn’t. And my doctor laughed. Like I was being dramatic. I stopped taking it. Never again. Why is this even a question??
Oh please. Women are just more hypochondriac. You take the same pill, same dose, and suddenly you’re in the ER because your "hormones are acting up." Meanwhile, my uncle takes 3x the dose and runs marathons. It’s not science - it’s narrative.
And don’t get me started on this "women are 59% of prescriptions" nonsense. Of course they are - they’re the ones taking birth control, thyroid meds, antidepressants, and supplements. Of course they’re going to report more side effects. They’re on more drugs. Duh.
Stop making everything about gender. Just fix the damn dosing. And stop blaming the system. People are just bad at taking meds.
While I appreciate the data presented, I must respectfully challenge the framing. The assertion that "women are more sensitive" is not only misleading - it’s dangerous. It reduces complex physiological differences to a stereotype of fragility. This isn’t about sensitivity. It’s about pharmacokinetics, hormonal modulation, and systemic neglect.
Moreover, the claim that women are "more visible" in healthcare systems doesn’t diminish the biological truth - it underscores the moral imperative. If women are more likely to seek care, then we have a responsibility to listen, not to dismiss. To adjust, not to assume.
Let’s not confuse visibility with exaggeration. The data doesn’t lie. The system does.
One thing no one talks about: the lack of female researchers in early drug trials. If more women had been designing these studies, would we have missed this? Probably not. We’d have had stratified data from day one.
And the fact that medical schools still don’t teach sex-based pharmacology? That’s not an oversight. It’s a curriculum failure. I had a professor in med school tell me "sex differences are too messy to teach" - and he was tenured.
Meanwhile, my sister took sertraline for anxiety and spent three weeks vomiting. Her doctor said "it’s normal" - until she showed him the FDA’s own data. Then he changed her dose. Took 20 minutes. Why didn’t he know this before?
Knowledge isn’t power if it’s locked behind paywalls and outdated textbooks.
Interesting. In India, we don’t even have proper dosing for men, let alone women. Most pills are sold in standard sizes. Doctors just hand out whatever’s cheapest. No one tracks side effects. No one cares. We’re lucky if we get a prescription at all.
But here’s the twist: women here are more likely to hide symptoms. They don’t go to doctors. They take grandma’s herbal tea. So the data we have? It’s skewed. We’re not seeing the full picture - we’re seeing the tip of a very silent iceberg.
Maybe the problem isn’t just Western medicine. Maybe it’s global medical arrogance.
I’m a guy who’s taken 12 different antidepressants. I’ve had side effects - but never the kind that land you in the ER. I didn’t realize how much this was a gendered issue until my wife started taking lamotrigine and her mood crashed. We found out later her birth control was neutralizing it. No one warned her.
This isn’t about blame. It’s about awareness. I’m glad someone finally wrote this. I’m sharing it with my doctor tomorrow. Maybe he’ll actually read it.
Look, I don’t care if it’s biology or patriarchy. What I care about is that my sister was prescribed a drug that made her hallucinate - and her doctor said "women are just more emotional." That’s not a diagnosis. That’s a dismissal. And now she’s terrified to take anything. Even Advil.
They told her it was "in her head." Turns out, it was in her liver. And her hormones. And her DNA. But no one checked.
Now she’s a nurse. And she’s the first one to ask: "Was this tested on women?" And if the answer’s no? She refuses to give it to her patients.
Who funded this article? Big Pharma? The FDA? The NIH? Because if you look at the timeline - the same people who excluded women from trials in the 70s are now "leading" the solution. Coincidence? I think not.
This isn’t about science. It’s about control. Women are being told to "advocate" for themselves - but the system was built to silence them. Now they’re giving us a roadmap? Like we’re children being handed a crayon after being locked in a closet for 50 years.
Don’t be fooled. They’re not fixing the system. They’re rebranding it.
Why is no one talking about the fact that women are 3x more likely to be prescribed antidepressants? Of course they’re having side effects - they’re on 5 meds at once while men are on 1 or 2! It’s not biology - it’s overprescribing! And don’t even get me started on how doctors treat women like walking anxiety machines…
Also - who wrote this? It’s like a TED Talk with footnotes.