When your doctor suspects a heart problem, they often turn to imaging to see what’s really going on inside. Two tests come up again and again: cardiac MRI and echocardiography. Both show your heart in detail, but they’re not the same. One uses sound waves. The other uses magnets. One is quick and available in most clinics. The other takes longer but gives deeper answers. Choosing the right one isn’t about which is better-it’s about which is right for your situation.
How Echocardiography Works
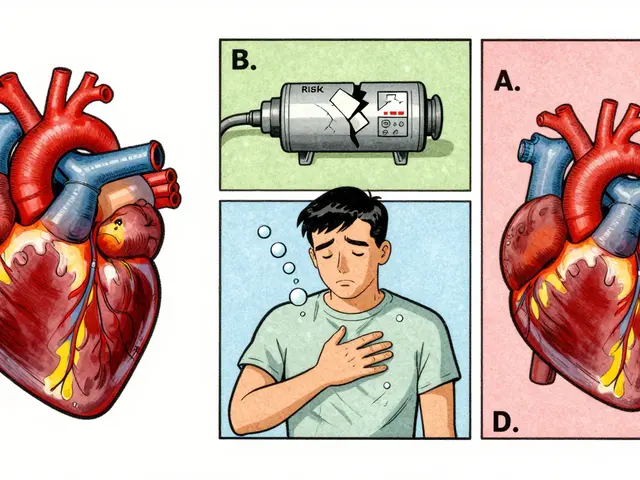
Echocardiography, or echo, is the most common heart imaging test in the U.S. Every year, about 15 million people get one. It uses high-frequency sound waves-ultrasound-to create moving pictures of your heart. A technician moves a small device called a transducer over your chest. It sends out sound waves that bounce off your heart and return as echoes. A computer turns those echoes into real-time video.What can echo show? The size of your heart chambers, how thick your heart walls are, how well your valves open and close, and how much blood your heart pumps out with each beat-called ejection fraction. Normal left ventricular ejection fraction is between 50% and 75%. Normal left ventricular end-diastolic dimension is 37 to 56 mm. These numbers help doctors spot problems like heart failure, valve leaks, or thickened muscle from high blood pressure.
One big advantage? Speed. An echo takes 20 to 45 minutes. It’s done right in the office. No special prep. No radiation. No needles. You can walk in and walk out. That’s why it’s the first test most doctors order. In an emergency, like chest pain or sudden shortness of breath, echo can be done at the bedside. It’s how doctors quickly rule out a heart attack or detect fluid around the heart.
How Cardiac MRI Works
Cardiac MRI, or CMR, is more complex. It uses powerful magnets and radio waves-not sound-to build incredibly detailed 3D images of your heart. You lie inside a long tube, similar to a regular MRI machine. The machine takes hundreds of images over 30 to 60 minutes, capturing your heart beating at different points in the cycle.What makes cardiac MRI special is its ability to show tissue, not just motion. It can detect scar tissue, inflammation, and fat deposits inside the heart muscle. This is done through a technique called late gadolinium enhancement (LGE), where a contrast dye highlights damaged areas. That’s something echo simply can’t do.
Cardiac MRI also gives the most accurate measurements of heart volume and muscle mass. Unlike echo, which uses math formulas to estimate size based on shape, MRI counts every pixel in 3D space. This means fewer errors. Studies show echo often underestimates heart chamber size by nearly 100 mL compared to MRI. Wall thickness readings from echo are also typically 1.1 mm thicker than MRI measurements.
Normal cardiac MRI values are different from echo. For men, left ventricular end-diastolic volume (LVEDV) ranges from 67 to 155 mL. For women, it’s 55 to 105 mL. LV mass is 49-115 g for men and 37-81 g for women. These numbers matter because they’re used to track disease progression over time-especially in conditions like hypertrophic cardiomyopathy or after chemotherapy.
When Echo Is the Best First Step
Most heart problems start with an echo. It’s fast, cheap, and widely available. If you have new shortness of breath, an irregular heartbeat, or a heart murmur, your doctor will almost always start with echo. It’s also the go-to for monitoring patients with known conditions like mitral valve prolapse or mild heart failure.It’s especially useful in emergencies. In a case of suspected aortic dissection, echo can show a tear in the aorta within minutes. If you’re in the ER and unstable, waiting for an MRI isn’t an option. Echo gives immediate answers.
It’s also the best tool for checking right heart function in some cases. The myocardial performance index, a measure of how efficiently the right ventricle works, is more reliable on echo than on MRI. Echo can also detect abnormal blood flow patterns using Doppler technology-like leaks through valves or narrowing in arteries.
But echo has limits. If you’re overweight, have chronic lung disease, or have a lot of scar tissue from past surgeries, the sound waves can’t get through well. That’s called a poor acoustic window. In those cases, the images are blurry or incomplete. And even under the best conditions, echo measurements vary more between doctors than MRI does. One study showed echo’s inter-observer variability for ejection fraction was 6.8%, compared to just 2.6% for MRI.
When Cardiac MRI Takes Over
Cardiac MRI isn’t the first test-but it’s often the final answer. When echo results are unclear, or when your doctor needs to know exactly what’s happening inside the heart muscle, MRI steps in.It’s the gold standard for diagnosing conditions like myocarditis, cardiac sarcoidosis, and amyloidosis. These diseases change the texture of heart tissue long before they affect pumping function. Echo might look normal. MRI shows the inflammation or scarring.
It’s also the best test for measuring heart muscle mass in people with hypertrophic cardiomyopathy. A thickened wall might look normal on echo, but MRI can reveal hidden areas of abnormal thickening. That changes treatment. In one study, MRI changed management in 19% of patients because echo missed key findings.
For cancer patients getting chemotherapy, cardiac MRI is critical. Some drugs damage the heart slowly. Echo might miss early changes. MRI can detect tiny amounts of fibrosis before the heart starts to weaken. A 2023 study found echo underestimated ejection fraction by 3% on average-and in 10% of cases, that led to wrong decisions about whether to keep giving chemo.
Cardiac MRI is also the most reliable way to track changes over time. If you’re being treated for heart failure or a genetic condition, your doctor needs to know if your heart is improving or getting worse. MRI’s low variability means small changes are real-not just measurement error.
Accuracy Differences Between the Two
The numbers don’t lie. Cardiac MRI is more accurate. But it’s not just about precision-it’s about what kind of precision matters.For volume and mass measurements, MRI wins by a wide margin. A 2011 study in the Journal of Cardiovascular Magnetic Resonance showed echo consistently measured smaller heart chambers and thicker walls than MRI. That’s because echo relies on geometric assumptions. If your heart isn’t a perfect ellipse, the math is off. MRI doesn’t assume anything. It counts every bit of tissue.
For ejection fraction, the gap is smaller but still meaningful. Echo’s variability is nearly three times higher than MRI’s. That means two different doctors could give you two different EF numbers on echo. On MRI, they’d likely agree within 3%.
Here’s the kicker: a 2023 study in the American Journal of Cardiology found that echo measurements were about 19% higher for wall thickness than MRI. That’s a big deal. If your echo says your septum is 15 mm thick, MRI might say it’s really 12.5 mm. That could mean the difference between a diagnosis of hypertrophy and a normal result.
3D echo has narrowed the gap. New machines with AI-assisted analysis now reduce echo variability to around 4.2%. But even the best 3D echo still can’t match MRI’s ability to show tissue changes.

Cost, Access, and Practical Reality
Echo costs between $500 and $1,500. Cardiac MRI costs $1,500 to $3,500. That’s a big difference. Insurance often requires echo first, then approves MRI only if needed.Access is another issue. Most community hospitals have echo machines on-site. You can get one the same day. Cardiac MRI? Only 35% of community hospitals offer same-week access. In some places, you wait two weeks or more for a non-urgent scan.
Cardiac MRI also has more restrictions. People with pacemakers, defibrillators, or certain metal implants can’t have it. Even newer MRI-safe devices sometimes cause artifacts that ruin the images. Echo has no such limits.
Training matters too. An echo tech can become proficient after 300-500 exams. A cardiac MRI specialist needs 1,000-1,500 interpretations. That’s why MRI is mostly done in academic centers. Fewer people know how to read it well.
What Doctors Actually Do in Practice
A 2022 survey of 127 cardiologists found that 89% use echo every day. Almost all of them rely on it for initial assessments. But 76% turn to cardiac MRI when echo doesn’t give clear answers.Real-world stories tell the rest. One echo tech with 15 years of experience said: “I’ve seen too many cases where echo missed the real problem-until MRI showed the fibrosis.” Another cardiologist shared: “I had three patients last year where MRI found tiny scars echo missed. That changed their treatment plan.”
On the flip side, patients often complain about the MRI experience. It’s loud. It’s long. You have to lie still. Some get anxious. Others can’t fit in the machine. And if you have an irregular heartbeat, the images get blurry unless special techniques are used.
Still, when the stakes are high-like diagnosing a rare heart disease or deciding whether to implant a defibrillator-doctors trust MRI more. It’s not about preference. It’s about certainty.
The Future: Hybrid Imaging
The field is moving toward combining the best of both. New ultrasound machines now use AI to auto-calculate volumes and detect subtle changes. New low-field MRI scanners (0.55 Tesla) can be used safely in patients with older pacemakers. Parametric mapping-measuring T1, T2, and ECV values-gives even more detailed tissue data than traditional LGE.By 2030, experts predict hybrid protocols will become standard. An echo will be done first. If it’s unclear, a targeted MRI will follow. That way, you get speed and accessibility when you need it-and precision when it matters most.
For now, the rule is simple: echo first, MRI when needed. Neither replaces the other. They complement each other. Your heart doesn’t care which machine is used-it just wants the right answer.
Which is better for measuring heart function: cardiac MRI or echocardiography?
Cardiac MRI is more accurate for measuring heart function, especially ejection fraction and chamber volumes. It doesn’t rely on assumptions about heart shape, unlike echocardiography. MRI’s inter-observer variability is under 3%, compared to nearly 7% for echo. That makes MRI the gold standard for tracking changes over time, especially in complex conditions like heart failure or cardiomyopathy.
Can I have a cardiac MRI if I have a pacemaker?
It depends. Older pacemakers and defibrillators are still a strict no-go for standard MRI machines. But newer MRI-conditional devices are designed to be safe. Also, new low-field MRI scanners (like Siemens’ 0.55 Tesla system) can image patients with many older implants. Always tell your doctor about any device before scheduling an MRI. They’ll check the model and decide if it’s safe.
Why does my doctor order an echo before an MRI?
Echo is faster, cheaper, and available everywhere. It’s perfect for the first look at your heart. If it shows a clear problem-like a leaky valve or reduced pumping-no further test may be needed. MRI is reserved for when echo can’t give a complete picture: unclear results, suspected tissue damage, or when precise measurements are critical for treatment decisions.
Does cardiac MRI use radiation?
No. Cardiac MRI uses powerful magnets and radio waves, not X-rays or radiation. That’s one reason it’s preferred for repeated imaging, especially in younger patients or those needing long-term monitoring. The only potential concern is the gadolinium contrast dye, which is rarely used and carries a small risk in people with severe kidney disease.
How long does it take to get results from a cardiac MRI?
The scan itself takes 30 to 60 minutes. But interpretation by a specialized radiologist or cardiologist can take several days, especially in busy centers. Echo results are often available the same day. For urgent cases, MRI reports can be expedited. Always ask your doctor when to expect results and if there’s a way to get them faster if needed.





This article is literally a masterpiece but let me tell you something - if you're in India and your doctor says 'get an echo,' you're lucky if you even get a decent machine. I had to travel 300 km because the local hospital's echo machine was older than my grandfather's transistor radio. And don't even get me started on MRI wait times - 6 weeks?! My heart was beating out of my chest the whole time. They should just give us portable MRI drones already.
So echo is cheap and fast but MRI is more accurate right but like how much does that actually matter if you're not a cardiologist I mean I had an echo and they said my EF was 58 and I'm fine but what if it was really 52 according to MRI does that change anything for me or is it just doctor math
Cardiac MRI is like the VIP lounge of heart scans 🎫❤️🩹 while echo is the bus that gets you there 🚌 But honestly I'd rather take the bus if it means I don't have to scream into a tube for an hour 😅
Let's be real. Echo is a glorified guess. MRI is the only thing that tells you what's actually happening in your myocardium. The fact that insurance makes you jump through hoops to get an MRI is criminal. I had a patient with suspected sarcoidosis - echo looked fine. MRI showed fibrosis everywhere. They delayed treatment for three months because of 'cost-effectiveness.' That's not medicine. That's accounting with a stethoscope.
It is a matter of profound concern that the United States continues to promote echocardiography as a primary diagnostic modality while the United Kingdom and other European nations have long since integrated cardiac MRI into standard clinical pathways. The disparity in healthcare outcomes is not merely technological - it is cultural. We must demand higher standards. The British Heart Foundation has published clear guidelines on this matter since 2018. Why are we still using 1980s logic in 2025?
I wonder if we're over-indexing on precision when what we really need is context. A number is just a number - whether it's 58% or 55% ejection fraction. What matters is how the person feels, how they live, how their heart responds to stress. Maybe the real question isn't which machine is better - but which patient are we trying to heal?
Let me break this down for the laypeople - echo is a 2D approximation using geometric assumptions that assume your heart is a perfect ellipsoid which it isn't. MRI is 3D volumetric pixel-perfect quantification with LGE for fibrosis detection and parametric mapping for T1/T2/ECV profiling - the gold standard for tissue characterization. If your cardiologist is still relying solely on echo for HCM or amyloidosis, they're practicing medicine like it's 2005. Get a second opinion. Now.
I had an MRI last year and the tech said I moved a little and the images were blurry so they had to redo it. I was sweating bullets just lying there. Echo was way easier. I was in and out in 20 minutes and I didn't even need to take my shirt off
My dad had an echo last month. They said his valves were fine. He kept feeling off. Got an MRI three weeks later - turned out he had early myocarditis. Echo missed it. I'm just glad we pushed for more. Sometimes you gotta fight for the truth.
Why are we even talking about this in the US when India has better access to MRI now with government health schemes and AI-powered portable scanners being rolled out in rural clinics. Echo is outdated. We're moving forward while you're stuck in the 90s
Cost difference is huge. MRI is $3000. Echo is $800. Insurance won't pay unless echo fails. That's the system. Stop complaining. Do the math.
So let me get this straight… echo is the fast food version of heart scans and MRI is the five-star Michelin tasting menu? 🍽️ And we're surprised people are confused? I’d order the fancy one if I could afford it but my deductible says ‘go eat the burger and pray.’
If we're going to talk about accuracy, we need to talk about intention. Echo is designed for screening. MRI is for diagnosis. One is a net. The other is a scalpel. We don't use a scalpel to cut bread - we use it to dissect a tumor. The question isn't which is better. It's which tool serves the purpose. And sometimes, the purpose is just to rule out the worst-case scenario. Echo does that. And that's enough for now.