Anti-Nausea Medication Assistant
Find Your Right Anti-Nausea Treatment
Select your primary medication to get personalized recommendations for nausea relief.
Your Recommendations
Recommended Anti-Nausea Medication
Dosage Information
Cost Estimate
Key Timing Tips
Important: Always consult your doctor before changing medications or dosages. This tool is for informational purposes only.
Why Some Medications Make You Feel Sick
It’s not just bad luck if you feel nauseous after taking a pill. Many common medicines-antibiotics, painkillers, even multivitamins-can trigger nausea and vomiting. This isn’t rare. Up to 80% of people on strong cancer drugs experience it without treatment. Even routine meds like ibuprofen or amoxicillin can upset your stomach. The problem isn’t always your body being sensitive. It’s how the drug interacts with your brain and gut.
Medications cause nausea in a few ways. Some irritate your stomach lining directly. Others trigger a part of your brain called the chemoreceptor trigger zone, which doesn’t care what’s in your stomach-it just reacts to chemicals in your blood. Then there’s the vomiting center in your brainstem, which gets activated by signals from your gut, inner ear, or even your emotions. That’s why stress or the sight of your pill bottle can make you feel sick, even before you take the medicine.
First-Line Fixes: What to Do Before Reaching for More Pills
Before you start taking extra anti-nausea drugs, try simple, proven steps. Most doctors agree: start here. If your pill says to take it on an empty stomach, that’s one thing. But if it doesn’t, take it with food. A small snack like crackers or toast can make a huge difference with antibiotics, NSAIDs, or iron supplements. Avoid greasy, spicy, or overly sweet foods-they make nausea worse.
Drink slowly. Sipping water, ginger tea, or clear broth helps. Dehydration makes nausea feel worse, but chugging fluids can trigger vomiting. Try a few sips every 15 minutes. If you can’t keep liquids down, use ice chips or popsicles. They hydrate without overwhelming your stomach.
Timing matters too. Some meds, like SSRIs for depression, cause more nausea when taken in the morning. Taking them at bedtime often reduces dizziness and queasiness. Always check with your pharmacist or doctor before switching times.
Ginger, Fresh Air, and Other Natural Helpers
Ginger isn’t just for cooking. It’s one of the most studied natural remedies for nausea. People on chemotherapy report cutting their nausea from an 8 out of 10 to a 3 out of 10 just by chewing ginger candies every two hours. Ginger tea, capsules, or even ginger ale made with real ginger (not just flavoring) can help. Look for products with at least 250mg of ginger per dose.
Get some fresh air. If you feel sick, step outside-even just to the porch or balcony. Stale, warm air makes nausea worse. Cool air helps reset your senses. Open a window. Sit near a fan. Breathe slowly and deeply. Breathing exercises aren’t just for meditation-they’re practical tools. Try inhaling for four counts, holding for four, exhaling for six. Repeat five times.
Avoid your favorite foods while you’re feeling off. It sounds odd, but if you eat your favorite meal while nauseous, your brain may link that food with feeling sick. Later, just smelling it could trigger nausea. Save those meals for when you’re back to normal.
When You Need Medicine to Stop the Nausea
If food, ginger, and fresh air aren’t enough, there are effective drugs-but they’re not all the same. The right one depends on what’s causing the nausea and how severe it is.
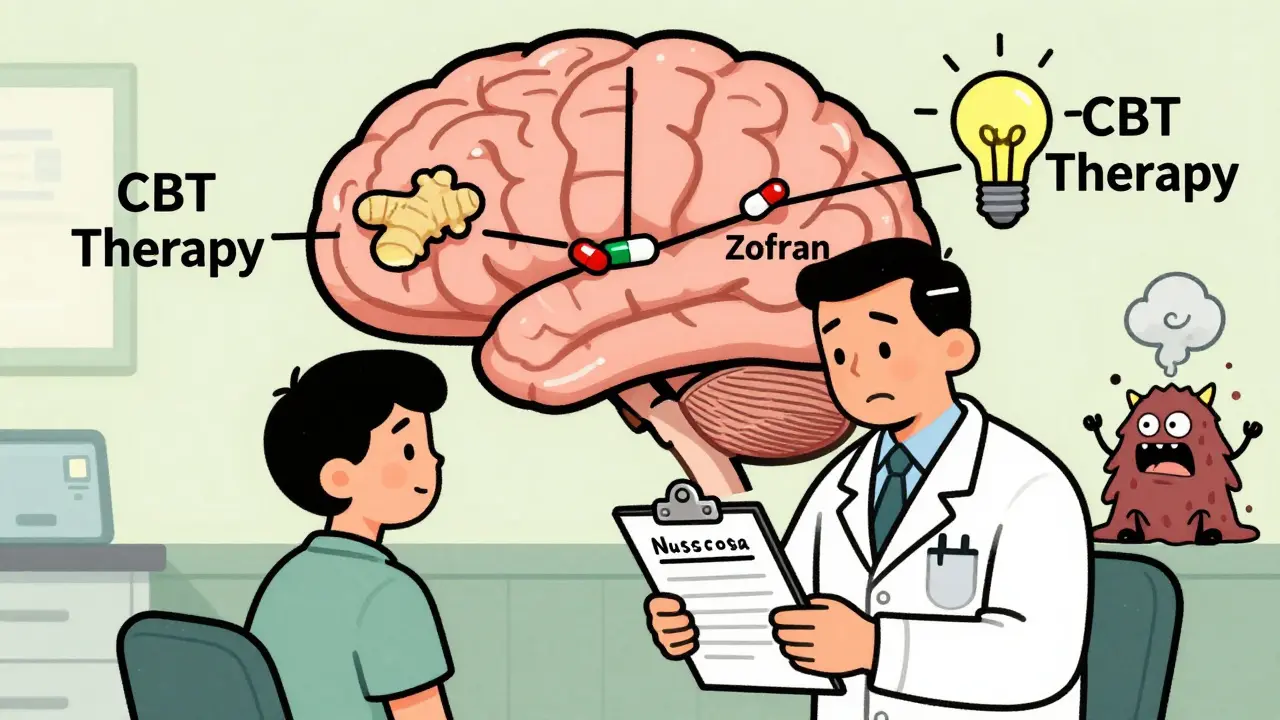
For chemotherapy or strong pain meds, serotonin blockers like ondansetron (Zofran) or granisetron (Kytril) are first choice. They block the signal from your gut to your brain. Taken 30 minutes before your main drug, they work well for most people. A 4mg tablet is common, but some need 8mg. Don’t take more than prescribed-too much can cause headaches or constipation.
For longer-lasting nausea, especially after chemo, drugs like aprepitant (Emend) or rolapitant (Varubi) are added. These block a different brain pathway and are often used with ondansetron and a steroid like dexamethasone. Together, they stop nausea in 75-85% of cases. But they’re expensive. Without insurance, a single dose can cost $150-$300. If cost is a problem, ask your doctor about generics or patient assistance programs.
For post-surgery nausea, a combination of ondansetron and dexamethasone works better than either alone. One study showed patients who got both before leaving the hospital had 23% less vomiting than those who got just one. For people who get nauseous from motion or vertigo, meclizine or dimenhydrinate (Dramamine) can help, but they cause drowsiness.
What Doesn’t Work-And What Can Make It Worse
Not every remedy is backed by science. Don’t rely on peppermint oil, acupuncture bands, or homeopathic drops if you’re dealing with serious drug-induced nausea. They might feel soothing, but they won’t stop the signal from your brainstem.
Also, don’t skip doses of your main medication just because you feel sick. Many people reduce or stop antibiotics, cancer drugs, or blood pressure meds to avoid nausea. That’s dangerous. Instead, talk to your doctor. They can adjust the dose, change the timing, or add an antiemetic. One survey found 35% of patients cut their meds without telling anyone-leading to treatment failure or worse outcomes.
Some anti-nausea drugs have risks too. Metoclopramide (Reglan) can cause involuntary muscle movements if used too long. Dolasetron can affect heart rhythm. Always ask your pharmacist about side effects and interactions. If you’re on other meds, they might clash.
Chronic Nausea? It Might Not Be the Drug
Some people feel nauseous for weeks or months after starting a new medication. If the nausea doesn’t improve after a few days, or if it gets worse, it might not be the drug at all. Other causes-like stomach infections, acid reflux, anxiety, or even thyroid problems-can mimic drug-induced nausea.
Doctors call this a “systematic investigation.” That means checking: Did the nausea start right after the drug? Does it get better if you skip a dose? Are there other triggers-stress, meals, sleep? If you’re on a medication for a chronic condition like gastroparesis or migraines, low-dose tricyclic antidepressants like nortriptyline might help. But not always. One major trial showed nortriptyline didn’t work better than a placebo for idiopathic gastroparesis. So, it’s not a universal fix.
Keep a symptom diary. Write down what you ate, what meds you took, when you felt sick, and what helped. Bring it to your next appointment. It gives your doctor a real picture-not just your memory.
What’s New in 2026
The field of anti-nausea treatment is evolving. In 2023, the FDA approved rolapitant for children as young as two, expanding options for young cancer patients. Newer drugs like HTL0022261 are in trials, aiming to be as effective as ondansetron but without the heart rhythm risks.
Hospitals are also using apps to track nausea. About 42% of top cancer centers now use digital tools where patients log symptoms daily. These apps alert doctors when nausea spikes, letting them adjust treatment faster. Some even use AI to predict when nausea is likely based on your history and meds.
Behavioral therapy is gaining ground too. For anticipatory nausea-where you feel sick just thinking about your next chemo session-cognitive behavioral therapy (CBT) is now recommended by major cancer societies. It helps retrain your brain to not associate treatment with sickness.
When to Call Your Doctor
Not all nausea needs emergency care. But call your provider if:
- You haven’t kept down any fluids for 12 hours
- You’re vomiting blood or material that looks like coffee grounds
- You have severe abdominal pain, fever, or dizziness
- You’re confused, dizzy, or your heart is racing
- Your nausea lasts more than 48 hours after starting a new drug
These could signal something more serious than a side effect.
Bottom Line: You Don’t Have to Suffer
Nausea from medication isn’t something you just have to live with. There are clear, science-backed ways to prevent it, reduce it, and even stop it. Start with food, ginger, and timing. If that’s not enough, talk to your doctor about the right antiemetic. Don’t skip your meds out of fear. Don’t guess what works. Use the tools available-and don’t be afraid to ask for help. Your treatment should work, not make you feel worse.










Been on antibiotics for a sinus infection and ginger candies saved my life. I was about to quit until I started chewing those little spicy bits every 2 hours. No more heaving into the toilet. Also, taking it with a spoonful of peanut butter? Chef’s kiss. Don’t overthink it.
bro i took my ibuprofen on an empty stomach and thought i was gonna die. then i ate a banana and suddenly my stomach was chill. why does no one tell you this??
I’m a nurse and I’ve seen so many patients stop their chemo meds because they couldn’t handle the nausea. But honestly? The combo of ondansetron + dexamethasone before treatment? Game changer. And ginger tea with a splash of lemon? Still my go-to after rounds. Don’t suffer in silence-your doc wants to help.
Of course the article mentions ‘fresh air’ like it’s some mystical cure. Meanwhile, I’m sitting in a hospital room with no windows, on 7 different meds, and the only thing keeping me alive is a $280 pill they call ‘Varubi.’ Thanks for the wellness tips, but my nausea isn’t a Pinterest board.
Okay but real talk-why is it that every time I take my SSRI in the morning I feel like I’m going to vomit up my soul, but if I take it at 10pm? Zero issues. I didn’t even know timing mattered until my pharmacist pulled me aside and said ‘have you tried not taking it before breakfast?’ Like, why is this not on the label? Also, I started using a symptom tracker app and it’s weirdly empowering. My doctor now sends me memes when my nausea logs drop. We’re a team.
THEY’RE HIDING THE TRUTH. Ginger doesn’t work because it’s natural-it works because the FDA banned the real cure. Big Pharma doesn’t want you to know that vitamin B6 and magnesium can stop nausea cold. They profit off your vomiting. Read the studies. The ones they don’t want you to see. I’ve been on 12 meds and none of them helped until I stopped trusting doctors. I’m not sick-I’m being poisoned.
Y’all are so brave for sharing this. I’ve been on chemo for 18 months and I used to cry every time I saw my pill bottle. But now? I have a little ritual: ginger candy, deep breaths, and my dog licking my hand while I lie on the floor. It’s not magic, but it’s mine. And if you’re reading this and feeling like you can’t do it? You’re already doing it. Just by being here. You’re stronger than you think. Keep going. You’ve got this. 💪🌸
As an American taxpayer, I refuse to subsidize $300 anti-nausea drugs when a $2 ginger tea would suffice. This is why healthcare is broken. Stop enabling pharmaceutical greed. Take the pill. Suck it up. Your ancestors didn’t have Zofran.
The efficacy of ginger in reducing chemotherapy-induced nausea has been demonstrated in multiple meta-analyses, with a pooled relative risk reduction of approximately 0.72 (95% CI: 0.61–0.85). However, heterogeneity across studies remains high, particularly regarding dosage, formulation, and patient comorbidities. Further, the mechanism of action remains incompletely characterized. While anecdotal reports are compelling, clinical guidelines should prioritize pharmacologic interventions with established pharmacokinetic profiles.
Wait-so you’re telling me I shouldn’t skip my meds just because I feel like garbage? But what if the meds are the problem? What if the whole system is rigged? What if my nausea is my body screaming that this isn’t right? I’m not ‘noncompliant’-I’m intuitive. And you’re just a robot who reads clinical guidelines. I’ll take my chances with kombucha and crystals. At least I’m not poisoning myself with ‘evidence-based’ nonsense.