When you pick up a prescription, you might see a label that says generic instead of the brand name you recognize. It’s cheaper-often 80% less. But does it work the same? That’s the question millions of people ask every year. The answer isn’t as simple as yes or no. Clinical studies over the last 30 years have dug deep into this, and what they show is both reassuring and nuanced.
What Makes a Generic Drug "Equal"?
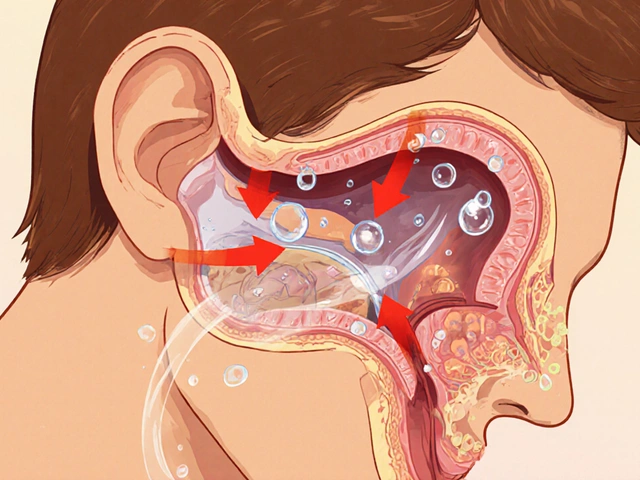
Generic drugs aren’t copies. They’re required by law to contain the exact same active ingredient, in the same strength, and delivered the same way as the brand-name version. The U.S. Food and Drug Administration (FDA) doesn’t just accept claims-they demand proof. Every generic must pass a bioequivalence test. That means in a controlled study with healthy volunteers, the generic must absorb into the bloodstream at the same rate and to the same extent as the brand. The FDA requires the 90% confidence interval for the ratio of absorption (measured by AUC and Cmax) to fall between 80% and 125%. That’s not a wide margin-it’s tight.
For example, if a brand-name pill releases 100mg of a drug into your blood over 8 hours, the generic must deliver between 80mg and 125mg in the same timeframe. This isn’t guesswork. It’s measured with blood tests, statistical models, and repeat trials. Over 2,000 studies reviewed by the FDA between 1996 and 2007 showed no meaningful difference in how generics and brand-name drugs behave in the body.
Real-World Outcomes: Do Generics Save Lives?
Lab results don’t always tell the whole story. What matters is what happens when real patients take these drugs day after day. A major 2020 study published in Scientific Reports looked at nearly all insured Austrians using 17 different drugs for chronic conditions like high blood pressure, diabetes, and heart failure. The results were striking. Patients taking generics had lower death rates in 10 of the 17 drugs and fewer major heart events in 11. After adjusting for age, income, and other health factors, the five-year survival rate for those on generics was 82.7%, compared to 79.8% for those on brand-name versions.
That’s not a fluke. Another study of 3.5 million U.S. patients, published in PLoS ONE in 2019, found no difference in outcomes for common drugs like amlodipine (for high blood pressure), glipizide (for diabetes), and escitalopram (for depression). In fact, for amlodipine, patients on the generic had a 9% lower risk of heart attack or stroke. These aren’t small populations-they’re massive, real-world datasets that mirror what happens in clinics and homes.
When Generics Don’t Work-The Exceptions
But here’s the part most people don’t talk about: sometimes, they don’t work the same. The FDA itself warns that for drugs with a narrow therapeutic index-where even a tiny change in blood level can cause harm or failure-switching between brands and generics needs caution.
Take levothyroxine, the drug for hypothyroidism. A 2023 analysis found that patients switching between different generic manufacturers had inconsistent thyroid hormone levels. One patient on Reddit said: “I tried three different generics for Synthroid. Only one kept my TSH stable.” Pharmacists report similar stories. In epilepsy, switching between generic versions of lamotrigine or levetiracetam has been linked to breakthrough seizures in some patients-even when bioequivalence tests say they’re identical.
A 2013 study documented a patient who kept having symptoms on a generic version of levofloxacin. Switching back to the brand name, Tavanic®, cleared up the infection within days. These cases are rare, but they’re real. They happen because inactive ingredients-fillers, coatings, dyes-can affect how a drug dissolves in the stomach. For most people, that doesn’t matter. For a few, it does.

What Do Patients Actually Experience?
Surveys tell us more than clinical trials. A 2021 Medicare survey found that 68% of seniors using generic heart medications said they noticed no difference in effectiveness. Another 22% reported minor side effects that faded over time. But 10% said they stopped taking the generic because it “didn’t work.”
GoodRx reviews from over 12,000 users show a 4.2 out of 5 rating for generics, with 78% saying they’re just as effective as the brand. But the complaints cluster around specific drugs: thyroid meds, seizure drugs, blood thinners, and antidepressants. These are the ones where even a 5% difference in absorption can matter.
And there’s another factor: perception. If you believe a generic won’t work, you might notice side effects more-or feel worse, even if the drug is identical. This isn’t “all in your head.” Studies show that expectations can change how your body responds to medication. That’s why doctors are encouraged to talk openly about generics, not just assume patients are fine with the switch.
Why Do Pharmacists Automatically Switch?
In the U.S., pharmacists are allowed-and often required-to swap a brand-name drug for a generic unless the doctor writes “dispense as written.” That happens in only 3.2% of prescriptions. Why? Because it saves money. The average generic costs 80-85% less than the brand. In 2022, generics made up 90% of all prescriptions filled in the U.S. but only 23% of total drug spending. That’s $612 billion saved between 2012 and 2021.
The FDA’s Orange Book lists every approved generic and rates them as “A” (therapeutically equivalent) or “B” (possible differences). Most are A-rated. But when a drug has multiple generics from different manufacturers, the FDA doesn’t guarantee that all generics are identical to each other-only that each is equivalent to the original brand.
What Should You Do?
If you’re on a generic drug and feeling fine-keep taking it. The odds are overwhelmingly in favor of it working just as well.
If you’re switching from a brand to a generic and notice new side effects, worsening symptoms, or a loss of effectiveness, talk to your doctor. Don’t assume it’s “just in your head.” Request a switch back to the brand-or try a different generic manufacturer. Some pharmacies let you request a specific generic brand. If you’re on a narrow therapeutic index drug (thyroid, seizure, warfarin, digoxin), ask your doctor to monitor your levels closely after a switch.
Don’t avoid generics because of fear. But don’t ignore your body’s signals either. The science supports generics for most people, most of the time. But medicine isn’t one-size-fits-all. Your experience matters.
What’s Changing Now?
The FDA is stepping up its scrutiny. With the new GDUFA III program (2023-2027), they’re allocating over $1 billion to improve testing for complex generics-like inhalers, patches, and extended-release pills. These are harder to copy. A 2023 study in Epilepsia found a 18% higher chance of seizures after switching between generic versions of levetiracetam. That’s driving new rules. By 2025, the FDA may require more human studies for these complex drugs, not just lab tests.
Manufacturing quality is also under fire. In 2021, a global recall of valsartan (a blood pressure drug) affected multiple generic brands because of cancer-causing impurities. That wasn’t about efficacy-it was about safety. But it shook trust. The FDA now requires stricter oversight of overseas factories, which produce 80% of active ingredients for U.S. generics.
For now, the data is clear: for most drugs, most people, generics work just as well. But the exceptions matter. And knowing when to speak up could make all the difference.









My grandma switched to generic metformin last year and swears it gave her stomach issues. She went back to the brand and boom - no more bloating. I thought it was placebo, but she’s not the only one. My pharmacist said generics are fine for most, but if your body’s picky, it’s picky.
Let’s cut through the corporate fluff. The FDA’s bioequivalence standard of 80-125% is a joke. That’s a 45% window. Imagine if your car’s fuel efficiency could vary by that much between two ‘identical’ models. One gets 30 mpg, the other 43. You’d call it defective. But for drugs? ‘Oh, it’s still within range.’ Meanwhile, patients with epilepsy, thyroid disorders, or heart conditions are playing Russian roulette with their lives because some generic manufacturer used a cheaper coating that delays dissolution by 20 minutes. The system isn’t broken - it’s designed to prioritize profit over precision. And the ‘90% of prescriptions’ stat? That’s not a victory. It’s a indictment of a healthcare system that treats people like cost centers.
Oh wow, a whole article about how generics are ‘mostly fine’ and you didn’t even mention the fact that the FDA doesn’t test for bioequivalence in real patients - only healthy college kids on a 24-hour fast. So your ‘identical’ generic might work perfectly for a 22-year-old with no gut issues, but when your 72-year-old diabetic with gastroparesis takes it? Suddenly your insulin isn’t absorbing. That’s not science. That’s statistical theater. Also, the ‘80% cheaper’ claim ignores that many generics are made in India or China with supply chains that would make a cartographer cry. I’d rather pay more for a drug that doesn’t turn my kidneys into a science experiment.
I’ve been a pharmacist for 18 years. I’ve seen the horror stories - the elderly woman who had a seizure after switching generics, the man whose depression got worse because the filler in the generic changed how fast it hit his system. But I’ve also seen hundreds of patients thrive on generics. The key isn’t to fear them - it’s to monitor. If someone’s on levothyroxine or warfarin, we track levels. If they say, ‘This doesn’t feel right,’ we listen. It’s not about brand loyalty. It’s about patient-centered care. The data says generics work for most. But medicine isn’t about most. It’s about the one who’s suffering.
Look, I get it - you want to save money. But if you’re going to skimp on your meds, at least make sure they’re made in America. Why are we letting China and India pump out half-baked generics that get shipped here with zero real oversight? The FDA inspects maybe 2% of overseas plants. That’s not regulation - that’s negligence. And don’t give me that ‘it’s still FDA-approved’ crap. Approved doesn’t mean safe. It means they didn’t catch the mold in the batch. We’re risking lives to save $20 a month. That’s not frugal. That’s stupid.
generics r fine unless they aint…
It’s funny how we treat medicine like a car part - interchangeable, mass-produced, disposable. But your body isn’t a Honda Civic. It’s a symphony. One wrong note - a different filler, a slightly slower dissolution - and the whole thing falls apart. The system wants us to believe ‘equivalence’ is a mathematical certainty. But biology? It’s messy. It’s personal. And sometimes, the difference between life and death isn’t in the active ingredient… it’s in the coating.
People who say generics are fine are either rich enough to afford brand names or too ignorant to know the difference. My cousin died because her generic warfarin wasn’t absorbed properly. The pharmacy switched her without telling her doctor. No one took responsibility. Now you want me to believe this is just ‘statistical noise’? It’s not noise. It’s negligence wrapped in a corporate PowerPoint.
my doc said if i feel weird on a generic, just ask for the brand. no shame in it. i did that with my antidepressant and it made a world of difference. just talk to your pharmacist - they’re not just the guy who hands you the bottle.
Oh wow, the U.S. is so advanced! Meanwhile, in India, we use generics because we have to - and guess what? We don’t have 10% of patients reporting ‘it didn’t work.’ Maybe it’s because we don’t over-medicalize everything? Maybe it’s because we don’t turn every minor side effect into a conspiracy? The real problem isn’t the generic - it’s the American obsession with ‘perfect’ medicine and the cult of brand loyalty. Also, your FDA? They’re just a PR arm for Big Pharma. You’re being played.
As a Canadian, I can tell you our system is way smarter. We don’t have automatic substitution. If your doc prescribes a brand, you get the brand. If you want a generic, you ask. No one’s pressured. No one’s scared of losing their insurance. And we still save 70% on meds. The U.S. turns healthcare into a gamble. We treat it like… healthcare. 🇨🇦
I used to be terrified of generics after a bad experience with a thyroid med. But my pharmacist sat down with me, explained how to check the manufacturer code, and helped me find one that worked. Now I take a generic every month and feel great. It’s not about the label - it’s about the connection. Talk to your care team. Ask questions. You’re not being ‘difficult.’ You’re being smart. 💛
My mom’s on a generic for blood pressure and she’s been stable for 3 years. She didn’t even know it was generic until I told her. She said, ‘If it keeps me alive and I don’t feel weird, why does it matter?’ Sometimes the best science is just listening to your body - and not letting marketing scare you.
Just saw someone mention the levothyroxine issue - that’s spot on. I’ve had patients go from TSH 2.1 to 8.5 after a generic switch. No change in dose. Just a different manufacturer. We had to go back to the brand. It’s not about cost. It’s about consistency. If your thyroid’s unstable, you’re not just ‘feeling off’ - you’re at risk for heart problems, depression, even stroke. That’s not a ‘minor difference.’ That’s a clinical emergency waiting to happen.