DOAC vs Warfarin Decision Calculator
When you need a blood thinner, the choice between a direct oral anticoagulant (DOAC) and warfarin isn’t just about which pill to take-it’s about your daily life, your risk of bleeding, and whether you can stick with the treatment long-term. For millions of people with atrial fibrillation or a history of blood clots, this decision shapes everything from diet to doctor visits to peace of mind.
How DOACs and Warfarin Work Differently
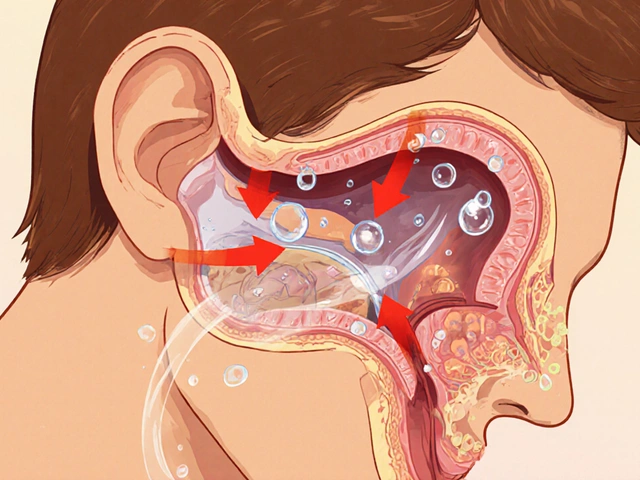
Warfarin has been around since the 1950s. It works by blocking vitamin K, which your body needs to make clotting proteins. That means your blood thins-but it also means your diet matters. Eating a big plate of spinach or kale one day and none the next can throw your INR levels off. You need regular blood tests, sometimes weekly, to make sure you’re in the safe range.
DOACs like apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa), and edoxaban (Savaysa) work differently. Instead of messing with vitamin K, they lock onto specific clotting factors-either factor Xa or thrombin-directly. That’s why you don’t need constant blood tests. You take the same dose every day, no matter what you eat. It’s simpler. But that simplicity comes with trade-offs.
Bleeding Risk: The Biggest Difference
The biggest advantage of DOACs over warfarin? Lower risk of serious bleeding. A 2024 meta-analysis of over 100,000 patients found DOACs cut major bleeding by 30% compared to warfarin. That’s not a small difference-it’s life-changing.
One of the scariest complications of warfarin is intracranial hemorrhage-a bleed in the brain. DOACs reduce that risk by 50-60%. That’s why neurologists and cardiologists now prefer DOACs for most patients with atrial fibrillation. In fact, the American Heart Association’s 2023 guidelines say DOACs are the first choice unless there’s a specific reason not to use them.
But not all DOACs are the same. Apixaban has the lowest bleeding rate among them-just 1.9 events per 100 person-years. Rivaroxaban? Higher. Around 2.8 events per 100 person-years. Warfarin sits in the middle at 2.4. If you’re older, have kidney issues, or have had stomach bleeding before, apixaban is often the safest pick.
What About Gastrointestinal Bleeding?
Stomach bleeds are a real concern with blood thinners. DOACs, especially rivaroxaban, carry a slightly higher risk than warfarin in this area. A 2024 JACC study showed rivaroxaban users had a 35% higher chance of GI bleeding than apixaban users. If you’ve had ulcers or gastritis in the past, your doctor might avoid rivaroxaban entirely.
Warfarin doesn’t escape this risk either. But the key difference? With warfarin, you can adjust your dose based on INR results. With DOACs, if you’re bleeding, you can’t just lower the pill. You have to wait for it to clear your system-or use a reversal agent.
Reversal Agents: What Happens When Things Go Wrong?
If you bleed badly on warfarin, doctors can give you vitamin K or a concentrate of clotting factors. It works, and it’s been used for decades.
For DOACs, we have targeted reversal drugs-but only for some. Idarucizumab (Praxbind) reverses dabigatran. Andexanet alfa (Andexxa) reverses factor Xa inhibitors like apixaban and rivaroxaban. These drugs are expensive, hard to get in rural hospitals, and not always available on weekends.
That’s a hidden risk. If you’re on a DOAC and live far from a big hospital, you might not get fast reversal if you have a major bleed. Warfarin users don’t have that problem.

Monitoring and Daily Life
Warfarin demands attention. You need regular INR tests. If your number is too low, you risk a clot. Too high, and you bleed. Many patients report feeling anxious between tests. One patient on a support forum said, “My INR was out of range 40% of the time in the first year-even with weekly blood draws.”
DOACs? You take your pill, and that’s it. No fasting. No diet restrictions. No weekly finger pricks. A 2023 survey of over 1,200 patients found 78% of DOAC users said their quality of life improved. Only 42% of warfarin users felt the same. Freedom from monitoring is a huge psychological win.
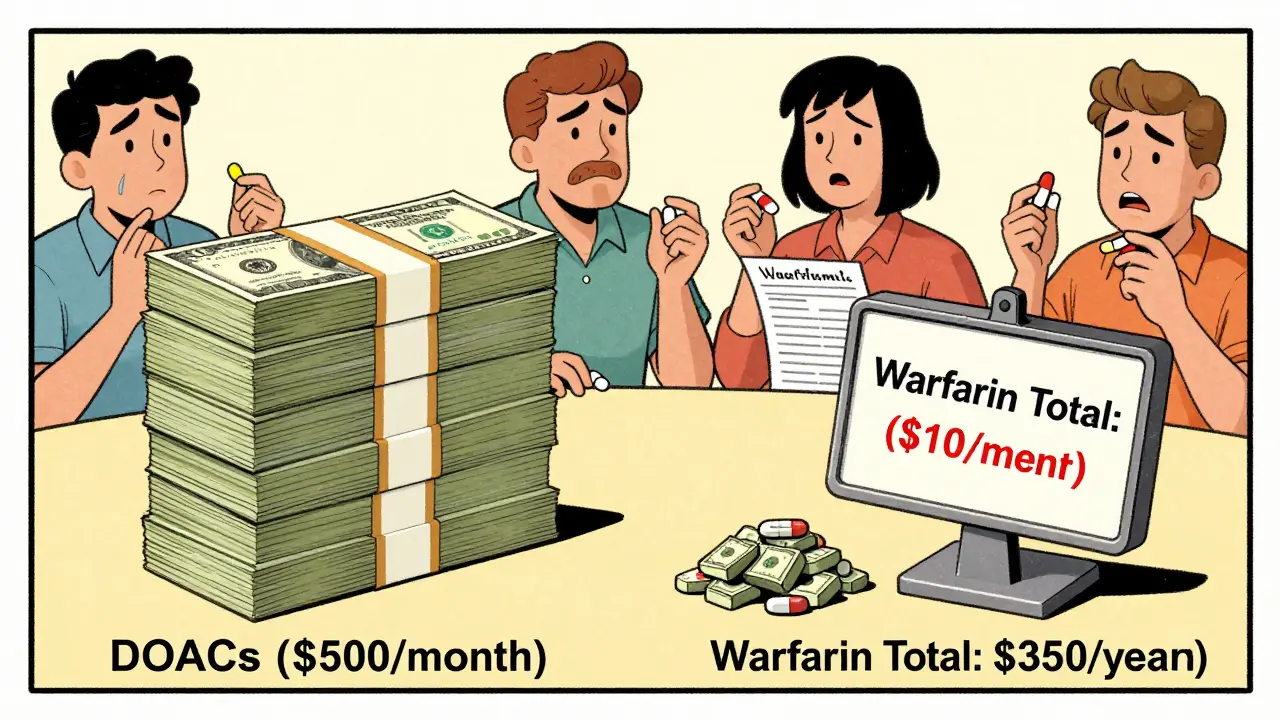
Cost: The Hidden Hurdle
Warfarin costs $4 to $10 a month. Generic, easy to get, covered by almost every plan.
DOACs? Without insurance, they’re $450 to $600 a month. Even with Medicare Part D or private insurance, your copay might be $30 to $100. That’s a burden. On Reddit’s r/bloodthinners, 63% of posts mentioned cost as a major stressor. Some patients skip doses to make the pill last longer. That’s dangerous.
But here’s the twist: when you add up the cost of warfarin monitoring-blood tests, doctor visits, lab fees, time off work-it can hit $350 a year. That’s the break-even point. If you’re getting more than 13 INR tests a year, DOACs become cheaper. For many, they already are.
Who Should Still Use Warfarin?
DOACs aren’t for everyone. If you have a mechanical heart valve, DOACs are dangerous. They can cause clots on the valve. Warfarin is the only approved option.
Same goes for antiphospholipid syndrome. People with this autoimmune condition have a 2.8 times higher risk of clots on DOACs compared to warfarin, according to the 2021 American Society of Hematology guidelines. Warfarin still wins here.
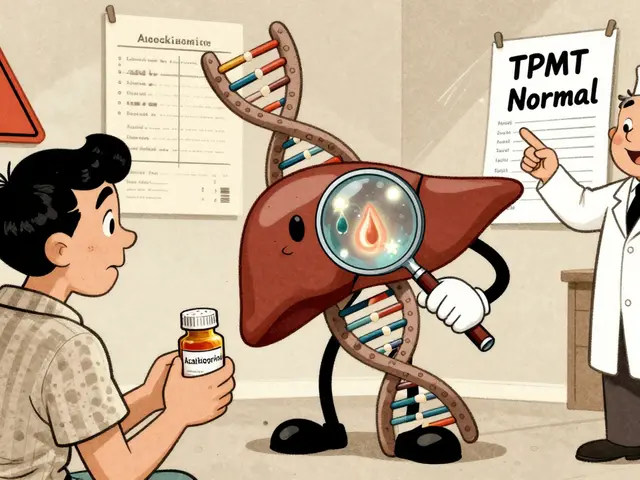
Severe kidney failure? Most DOACs aren’t safe if your creatinine clearance is below 15-30 mL/min. Apixaban can be used down to 15, but others can’t. If your kidneys are failing, warfarin might be your only choice.
Real-World Pitfalls
Doctors don’t always get it right. A 2022 audit found 18% of DOAC prescriptions were wrong-usually because the patient’s kidney function wasn’t checked. Dosing errors are common in older adults. One 82-year-old with reduced kidney function was given full-dose rivaroxaban. She ended up in the ER with a GI bleed.
Another problem? Missing doses. DOACs leave your system fast-within 12 to 24 hours. Skip a dose of rivaroxaban, and your protection drops quickly. Warfarin lingers longer. That’s why adherence matters more with DOACs.
What’s Next?
Generic apixaban hits the market in 2026. Rivaroxaban will follow in 2027. That could slash costs by 80%. That’s huge for patients who’ve been paying $80 a month.
Researchers are also testing new reversal agents like ciraparantag-a single drug that could reverse all anticoagulants, DOACs and warfarin alike. That could change the game.
And now, doctors use a simple 5-point score to pick the best DOAC: age over 75, kidney problems, past bleeding, taking aspirin or NSAIDs, or being female. Three or more points? Apixaban is the go-to.
Bottom Line: Which One Is Right for You?
If you’re young, healthy, have no kidney issues, and can afford the copay, DOACs are almost always the better choice. Lower bleeding risk, no diet changes, no weekly blood tests. Apixaban is the safest DOAC.
If you have a mechanical valve, antiphospholipid syndrome, or very bad kidney disease, stick with warfarin. It’s still the gold standard there.
If cost is a barrier, talk to your doctor about patient assistance programs. Many drugmakers offer free or discounted DOACs for low-income patients. And don’t forget-warfarin’s monitoring costs add up. What seems cheap upfront might not be.
There’s no one-size-fits-all. But for most people today, DOACs offer more safety, more freedom, and better outcomes. The data doesn’t lie. The question is: which version of your life do you want to live?








DOACs are a game-changer for folks like me who hate needles and blood tests. No more weekly finger pricks, no more worrying if I ate too much kale. I’ve been on apixaban for two years and honestly, it’s the first time I’ve ever felt like my medication didn’t control my life.
ok but have yall read the 2025 FDA warning about DOACs and kidney failure?? they’re slowly pulling rivaroxaban off the market in europe bc of the GI bleed stats and no one’s talking about it??
DOACs are a Big Pharma scam. 🤫 They’re pushing them because they’re more profitable. Warfarin’s been around for 70 years and works fine. The ‘lower bleeding risk’ is just a marketing lie. The reversal agents? Totally overpriced. They want you dependent on $600 pills and emergency hospital trips. 🧠💊
Just wanna say thank you for this post. I was on warfarin for 5 years and it was brutal. I cried during my 3rd INR test because I was so tired of being scared. Switching to apixaban felt like getting my life back. 💪❤️
There’s a deeper philosophical layer here that most people miss. The choice between DOACs and warfarin isn’t just medical-it’s existential. Warfarin forces you into a rhythm of vigilance, of surrender to the body’s unpredictability. DOACs offer the illusion of control: take a pill, forget it, live. But is forgetting safer than remembering? Or are we just outsourcing anxiety to the pharmaceutical industry? The real question isn’t which drug is better-it’s which version of human vulnerability we’re willing to accept.
People keep saying DOACs are safer, but they ignore the fact that warfarin has a 70-year safety record and a known reversal protocol. DOACs? Half of rural ERs don’t have Andexxa. You think you’re getting freedom? You’re getting a time bomb with a 12-hour expiration date. If you’re young and healthy, sure. But if you’re 78 and live in Nebraska? You’re gambling.
The data presented is robust and aligns with current clinical guidelines. Apixaban’s bleeding profile remains superior across multiple cohorts. However, adherence remains a critical factor, particularly in elderly populations with polypharmacy. Cost-benefit analyses must incorporate both direct and indirect healthcare utilization metrics.
DOACs are just expensive placebo pills wrapped in hype. The FDA is corrupt. The studies are funded by drug companies. My uncle died on warfarin because his INR was off-so now they want us all on these mysterious chemicals? No thank you.
One cannot help but observe the ontological tension inherent in this therapeutic dichotomy: warfarin, the ancient oracle of coagulation, demanding ritualistic sacrifice in the form of blood draws and dietary discipline; versus the DOACs, sleek, silent, and algorithmic, promising liberation through abstraction. Are we trading the burden of vigilance for the burden of obsolescence? The pill does not remember. The body does. And in that silence lies both salvation and peril.
India should ban these DOACs. They’re made in America to exploit poor people. Warfarin is cheap, proven, and our own doctors know how to use it. Why do we need fancy pills that cost more than a month’s salary? This is medical colonialism.
As someone who’s counseled hundreds of patients on anticoagulants, I’ve seen the quiet relief on a 70-year-old’s face when they realize they don’t need to plan their life around a blood test. Apixaban isn’t just a drug-it’s a quiet act of dignity. And yes, cost is brutal. But patient assistance programs exist. Ask your pharmacist. You’d be surprised how many don’t know they qualify.
Generic apixaban in 2026. Finally. Took long enough.