Managing allergies during pregnancy isn’t just about sneezing and itchy eyes-it’s about making smart choices that protect both you and your baby. Around 1 in 3 pregnant people deal with allergic rhinitis, hives, or asthma flare-ups, and many worry: Can I take my allergy meds while pregnant? The answer isn’t simple. Some medications are safe. Others carry risks. And timing matters-what’s okay in week 20 might not be safe in week 6.
First Trimester: The Most Sensitive Window
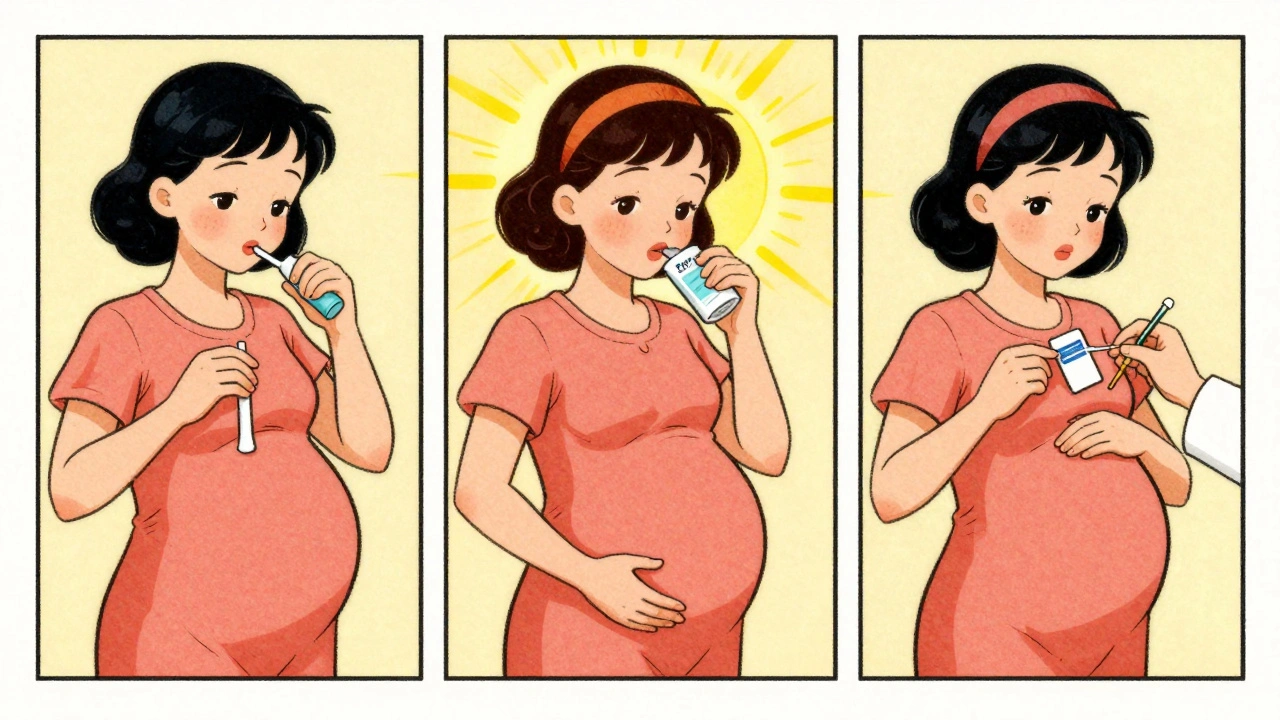
The first 12 weeks of pregnancy are when your baby’s organs are forming. That’s why doctors recommend avoiding all non-essential medications during this time-even if they seem harmless. If you’re struggling with allergies, start with non-drug options. Try saline nasal sprays or rinses (neti pots are fine if used with distilled water). Use HEPA filters in your bedroom. Keep windows closed during high pollen seasons. Wash bedding weekly in hot water to cut down on dust mites.
If symptoms are severe and you need something stronger, your best bet is budesonide (Rhinocort). It’s the only nasal steroid with the most solid safety data across hundreds of pregnancies. Fluticasone (Flonase Sensimist, Flonase Allergy Relief) and mometasone (Nasonex) are also considered low-risk, but budesonide has the most research backing it. Avoid Nasacort (triamcinolone)-it doesn’t have enough data to be recommended.
Oral Antihistamines: First-Gen vs. Second-Gen
When nasal sprays aren’t enough, antihistamines come into play. There are two main types, and they’re very different in how they behave during pregnancy.
First-generation antihistamines like diphenhydramine (Benadryl) and chlorpheniramine (Chlor-Trimeton) have been used for decades. Studies tracking over 200,000 pregnancies found no increase in birth defects with these drugs. They work well. But they cause drowsiness-sometimes so much that people can’t drive or function normally. If you’re okay with that trade-off, they’re a reliable choice. Dosing is typically 25-50 mg every 4-6 hours as needed.
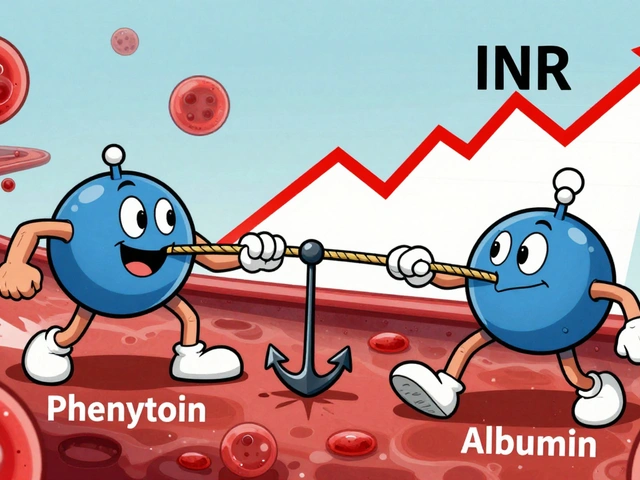
Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) are non-sedating. That’s a big plus. But their safety data isn’t as extensive. Still, multiple studies show no increased risk of birth defects. Cetirizine and loratadine are both classified as Pregnancy Category B-meaning animal studies show no risk, and human data is reassuring. Fexofenadine is Category C, meaning animal studies showed some risk, but human data is limited. Despite that, most allergists still consider it safe after the first trimester. Dose is 10 mg once daily for all three.
Watch out for combo products. Claritin-D, Zyrtec-D, and Allegra-D contain pseudoephedrine. That’s a red flag. Avoid them entirely.
Decongestants: The Big No in Early Pregnancy
Pseudoephedrine (Sudafed) and phenylephrine are the most common oral decongestants. And they’re risky-especially in the first trimester. A 2009 study found that using pseudoephedrine in early pregnancy was linked to a 2.4 times higher chance of gastroschisis, a rare abdominal wall defect in newborns. That’s why most experts say: skip it in the first 12 weeks.
After the first trimester, things change. Mayo Clinic updated its guidelines in December 2023 to say that if you have severe congestion and no other options, you can use pseudoephedrine at 30-60 mg every 4-6 hours, not exceeding 240 mg in 24 hours. But only if you don’t have high blood pressure. Even then, it’s a last resort. Phenylephrine has even less safety data and is not recommended.
Nasal decongestant sprays like Afrin (oxymetazoline) are sometimes used for short bursts-no more than 3 days. But they’re not ideal. They can cause rebound congestion and have not been studied well in pregnancy. Better to stick with saline sprays.

What About Allergy Shots?
If you were already getting allergy immunotherapy (shots) before you got pregnant, you can usually keep going. Studies show no increased risk to the baby. But if you’re thinking about starting shots now? Don’t. That’s a new exposure, and the immune system changes during pregnancy. Starting therapy during pregnancy could lead to stronger reactions, and the benefits don’t outweigh the unknowns.
Asthma and Allergies: Don’t Ignore the Lungs
About 8% of pregnant people have asthma. Untreated asthma is more dangerous to the baby than most asthma medications. Inhaled corticosteroids like budesonide, fluticasone, and mometasone are safe throughout pregnancy. They go straight to your lungs with minimal absorption into your bloodstream. Oral steroids like prednisone should only be used if absolutely necessary and for the shortest time possible. Always treat asthma aggressively during pregnancy-it’s not just about comfort. Low oxygen levels in mom = low oxygen levels in baby.
What to Avoid Completely
Some medications have clear red flags:
- Nasacort (triamcinolone) - Not enough safety data. Avoid.
- Pseudoephedrine in the first trimester - Linked to gastroschisis.
- Phenylephrine - Poor data, no proven safety.
- Any “-D” product - That means it has a decongestant.
- Sustained-release or extended-release antihistamines - These release the drug slowly, which increases exposure. Stick to immediate-release.
Real-Life Scenarios: What Works in Practice
Here’s how this looks for real people:
- Sarah, 28, 8 weeks pregnant - Has seasonal allergies. Uses saline rinses twice daily and Rhinocort nasal spray. No meds beyond that. Symptoms are mild but manageable.
- Maria, 32, 16 weeks pregnant - Has year-round allergies and hives. Took Claritin before pregnancy. Switched to cetirizine (Zyrtec) 10 mg daily. No drowsiness. Symptoms under control.
- Leah, 35, 22 weeks pregnant - Developed severe nasal congestion. Tried saline, then Rhinocort. Still blocked. Used pseudoephedrine 60 mg once daily for 4 days, under her OB’s guidance. No side effects. Congestion cleared.
The pattern? Start low. Use local treatments first. If you need more, pick the medication with the most evidence. And always talk to your doctor or allergist before starting or stopping anything.
What’s Changing in 2025?
The FDA stopped using the old A, B, C, D, X labels in 2018. Now, drug labels include detailed narratives about risks, benefits, and animal vs. human data. But many doctors and websites still use the old system. That’s why you’ll see conflicting info online. The most current guidance comes from the American Academy of Allergy, Asthma & Immunology (AAAAI) 2023 update, which confirms that first-gen antihistamines still have the strongest safety record, while second-gen options like loratadine and cetirizine are now considered first-line due to better tolerability.
The NIH is running a big study called the Pregnancy Exposure Registry. Since 2018, over 15,000 pregnant women have enrolled to track what happens when they take allergy meds. Early results are expected in late 2024. That will likely lead to updated guidelines in 2025.
Bottom Line: What to Do Today
If you’re pregnant and fighting allergies:
- Try non-drug options first: saline rinses, air filters, allergen avoidance.
- If you need medication in the first trimester, use budesonide nasal spray or chlorpheniramine/diphenhydramine if sedation isn’t a problem.
- After the first trimester, cetirizine or loratadine are safe, effective, and non-sedating.
- Avoid all decongestants (oral or nasal) unless your doctor says it’s necessary-and even then, use the lowest dose for the shortest time.
- Never take anything labeled “-D” or “multi-symptom.”
- If you have asthma, keep using your inhaled steroid. Don’t stop.
Your symptoms matter. Your baby’s safety matters more. But you don’t have to suffer. With the right choices, you can breathe easy-without risking your pregnancy.
Can I take Benadryl while pregnant?
Yes, diphenhydramine (Benadryl) is considered safe during pregnancy, especially after the first trimester. Decades of data show no increased risk of birth defects. But it causes strong drowsiness, so it’s best used at night or when you don’t need to drive or operate machinery. Stick to the regular immediate-release form, not extended-release.
Is Zyrtec safe in the first trimester?
Cetirizine (Zyrtec) is generally considered safe after the first trimester. While animal studies show no harm and human data is reassuring, most doctors prefer to avoid it in the first 12 weeks unless symptoms are severe. First-generation antihistamines like chlorpheniramine have more extensive safety data in early pregnancy. If you need an antihistamine in week 6, your doctor might recommend that instead.
Can I use Flonase while pregnant?
Yes, Flonase Sensimist (fluticasone furoate) and Flonase Allergy Relief (fluticasone propionate) are considered safe during pregnancy. But Rhinocort (budesonide) is preferred because it has the most robust safety data. All nasal corticosteroids are much safer than oral decongestants. Use the lowest effective dose.
Why is pseudoephedrine dangerous in early pregnancy?
Pseudoephedrine has been linked to a rare but serious birth defect called gastroschisis, where the baby’s intestines develop outside the abdomen. A 2009 study found a 2.4-fold increase in risk when taken during the first trimester. It can also raise blood pressure, which is risky for pregnant women with preeclampsia or hypertension. Avoid it in the first 12 weeks. After that, use only under medical supervision.
Are allergy shots safe during pregnancy?
If you were already getting allergy shots before becoming pregnant, you can usually continue them at the same dose. Stopping suddenly could cause a flare-up. But you should not start allergy shots during pregnancy. The immune system changes, and the risk of a severe reaction is higher. Always discuss this with your allergist.
What’s the safest antihistamine for pregnancy?
For the first trimester, chlorpheniramine or diphenhydramine are the safest based on long-term data. After the first trimester, cetirizine (Zyrtec) and loratadine (Claritin) are preferred because they’re non-sedating and have strong safety records. Fexofenadine (Allegra) is also an option but has less human data. Always choose single-ingredient products without decongestants.









Saline rinses saved my life in the first trimester. No drowsiness, no worries. Just water and a neti pot. Do it.
Let me be perfectly clear: using Benadryl during pregnancy is not just irresponsible-it’s a dangerous gamble with a child’s life. There are safer alternatives, and if you’re choosing sedating antihistamines because you’re too lazy to try saline sprays, you shouldn’t be a parent. The data may say ‘no birth defects,’ but that doesn’t mean it’s ethical.
Important to note that the AAAAI 2023 update explicitly elevates cetirizine and loratadine to first-line status due to their favorable pharmacokinetics and extensive human cohort data-especially in the second and third trimesters. Budesonide remains the gold standard for nasal steroids, but fluticasone is non-inferior in real-world practice. Also, avoid any product with ‘-D’-pseudoephedrine’s vasoconstrictive effects on placental vasculature are well-documented. And yes, asthma control is non-negotiable; uncontrolled maternal hypoxia poses a far greater fetal risk than inhaled corticosteroids.
When i think about pregnancy and meds i think about the balance between human need and cosmic order. The body is not a machine to be fixed with pills, it is a sacred vessel. To take a chemical is to interfere with nature’s rhythm. Yet we live in a world of convenience, where even sneezing is seen as a problem to be solved. Is it not wiser to sit with discomfort, to breathe through it, to let the body adapt? Perhaps the allergy is not the enemy but a messenger. We have forgotten how to listen. The neti pot is a tool, yes, but the soul needs silence more than spray.
If you’re still using diphenhydramine in 2025, you haven’t read the literature. Zyrtec and Claritin are not just ‘safe’-they’re superior. The fact that people still reach for Benadryl like it’s 1998 is why medicine has such a bad reputation. Also, please stop calling Flonase ‘safe’-it’s not FDA-approved for pregnancy, it’s just not proven harmful. Big difference. And if you’re on allergy shots, congrats-you’re basically doing a clinical trial on your unborn child.
Oh great. Another ‘here’s how to medicate your baby’ guide. Let’s not forget that every drug you take is a tiny poison. And ‘safe’ doesn’t mean ‘risk-free.’ It means ‘we haven’t caught the damage yet.’ Did you know 40% of birth defects are idiopathic? Maybe we’re just not looking hard enough. And why is pseudoephedrine the villain but not the 100 other chemicals in your shampoo or toothpaste? Hypocrisy. Also, ‘non-sedating’ antihistamines? Try taking them for a week and then tell me you’re not foggy. You’re just too tired to notice.
I appreciate how this post acknowledges the tension between medical guidelines and lived experience. Sarah’s saline rinses, Maria’s Zyrtec, Leah’s short-term pseudoephedrine-these aren’t just case studies, they’re acts of courage. The real takeaway isn’t the drug names, it’s that every pregnant person deserves agency, not dogma. We don’t need a checklist-we need compassionate, individualized care. And yes, the FDA’s new labeling system is better, but it’s useless if doctors still quote ‘Category B’ like it’s scripture.
OMG I JUST TOOK ZYRTEC AT 9 WEEKS AND I’M SO SCARED 😭 BUT MY NOSE ISN’T RUNNING ANYMORE 😌 SO I’M GOING TO KEEP DOING IT 🙏 I’M TELLING MY OB TOMORROW BUT I’M SO ANXIOUS 😭😭😭
Saline rinses work wonders and dont forget to wash your pillowcase every week if you have dust mite allergies. Also if you have asthma dont stop your inhaler even if you feel fine. Low oxygen is silent and deadly. Budesonide is the one to use if you need a steroid. Avoid anything with D in the name. Simple.
bro i got pregnant last year and was on claritin for years so i just kept taking it. no issues. my kid is 1 now and runs like a cheetah. also i used rhinocort like it was water. no drowsiness, no drama. the real villain? stress. if you’re freaking out about meds, you’re probably doing more harm than the Zyrtec. breathe. trust your doc. and if you’re scared? talk to an allergist, not reddit.
...and yet, despite all this ‘evidence,’ the fact remains that the Pregnancy Exposure Registry has only enrolled 15,000 women-which is statistically insignificant when you consider the 4 million births per year in the U.S. alone. We’re making policy decisions based on underpowered studies, anecdotal reports, and outdated animal data. And you call this ‘science’? The real danger isn’t pseudoephedrine-it’s the illusion of certainty. You think you’re protecting your baby? You’re just playing Russian roulette with a loaded gun labeled ‘FDA-Approved.’