Meglitinide Hypoglycemia Risk Calculator
Personalized Hypoglycemia Risk Assessment
Based on clinical data showing meal delay increases hypoglycemia risk by up to 4x, this tool calculates your personalized risk level based on timing, medication type, and health factors.
Key Takeaways
- Meglitinides act fast and wear off quickly, so they fit erratic eating schedules-but only if meals are taken on time.
- Skipping or delaying a meal after a dose can raise hypoglycemia risk by up to fourfold.
- Repaglinide and nateglinide differ in onset, peak, half‑life, and metabolism; choose based on kidney function and lifestyle.
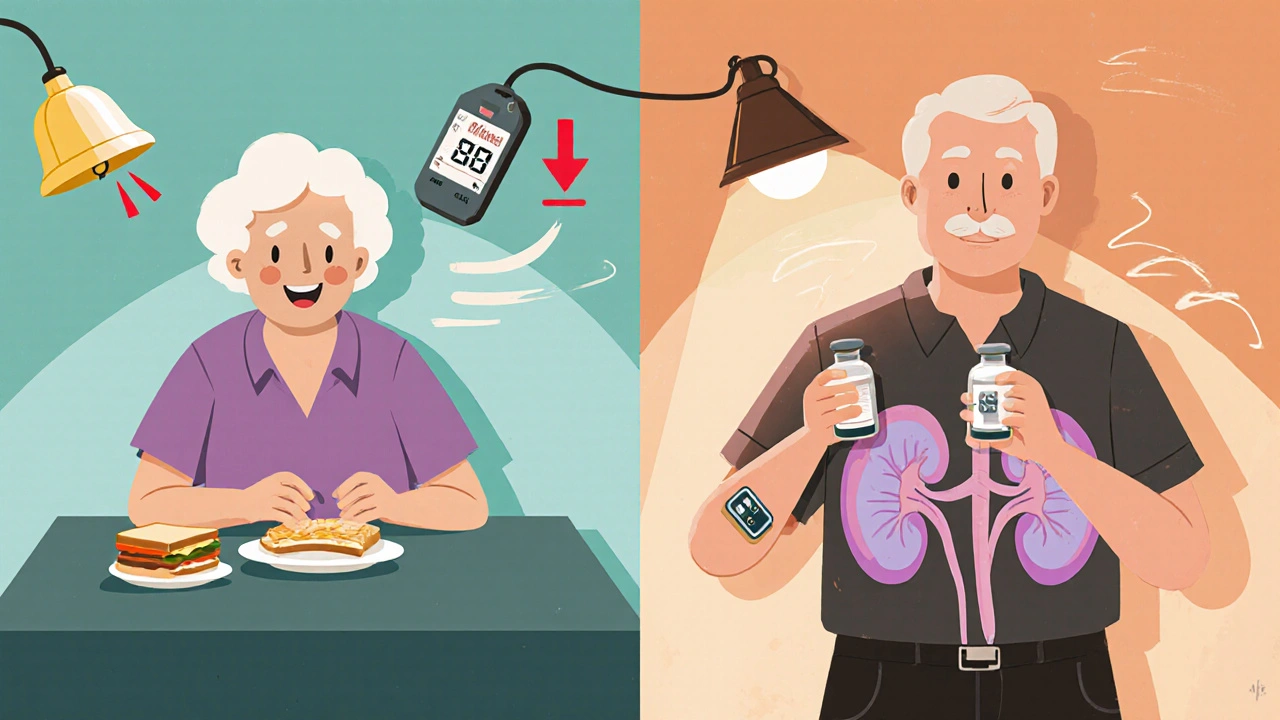
- Older adults, people with chronic kidney disease, and patients on combination therapy need extra monitoring, preferably with CGM.
- Smartphone reminders, dose‑to‑eat strategies, and extended‑release formulations can cut dangerous lows.
When a doctor prescribes a meal‑time pill for type 2 diabetes, the promise is simple: you can take it right before you eat, even if your schedule jumps around. That promise rests on a class of drugs called Meglitinides are short‑acting insulin secretagogues that stimulate the pancreas to release insulin just as food hits the bloodstream. They bind to sulfonylurea receptors (SUR1) on pancreatic β‑cells, shut the ATP‑dependent potassium channels (KATP), and trigger a calcium influx that forces insulin out. The rapid onset (15‑30 minutes) and brief action (2‑4 hours) make them attractive for people who don’t eat at fixed times- but that very speed creates a hidden danger when meals are missed.
How Meglitinides Work - The Fast‑Acting Mechanism
Both repaglinide and nateglinide sit on the same SUR1 pocket, yet their chemistry gives them slightly different timing. Nateglinide starts blocking KATP channels within a minute, while repaglinide needs 3‑5 minutes. After the block, the cell depolarizes, calcium channels open, and insulin granules pour out. Because the drug clears quickly-half‑life about 1‑1.5 hours-its insulin‑boosting effect fades by the time the meal’s glucose load is digested.
When Timing Goes Wrong - The Hypoglycemia Paradox
Clinical data are stark. A 2017 cohort showed that a single missed meal after a meglitinide dose increased hypoglycemia odds by 3.7 times, with glucose dropping below 70 mg/dL within 90 minutes. The risk climbs further in two groups:
- Older adults: Cognitive decline or inconsistent eating patterns make it easy to forget the 15‑minute pre‑meal rule.
- Patients with chronic kidney disease (CKD): Reduced clearance amplifies drug exposure, leading to a 2.4‑fold higher low‑blood‑sugar rate.
Both groups benefit from continuous glucose monitoring (CGM). One 2023 study reported a 57 % drop in hypoglycemia episodes for high‑risk meglitinide users who wore CGM devices.
Repaglinide vs. Nateglinide - Choosing the Right Pill
While both drugs share the same target, their pharmacokinetic fingerprints differ enough to guide prescribing.
| Attribute | Repaglinide | Nateglinide |
|---|---|---|
| Onset of action | 3‑5 minutes | ≈1 minute |
| Peak plasma time | 0.5‑1 hour | 1 hour |
| Half‑life | 1‑1.5 hours | 1.5 hours |
| Primary metabolism | CYP3A4 / CYP2C8 (hepatic) | Phase II glucuronidation |
| Renal safety | Preferred in CKD (hepatic clearance) | Use caution - more renal excretion |
| HbA1c reduction (average) | ‑0.9 % | ‑0.7 % |
| Hypoglycemia incidence | Higher than nateglinide (≈28 % more in head‑to‑head trial) | Lower |
For patients with moderate to severe CKD, repaglinide’s liver‑first pathway often makes it the safer bet. If a person’s schedule is truly erratic but they can guarantee a snack within 30 minutes of dosing, nateglinide’s faster onset may match the glucose spike better.
Practical Steps to Keep Blood Sugar Stable
- Take the pill 15 minutes before you plan to eat. If you’re unsure, wait until the food is ready-don’t pre‑dose and then delay.
- Never skip a meal after a dose. If you must skip, skip the pill too.
- Carry a fast‑acting carbohydrate (glucose tablets, juice) for emergency correction.
- Consider a “dose‑to‑eat” approach: only swallow the tablet when you know you’ll eat within the next half hour.
- Use reminder apps or alarms; studies show a 39 % drop in lows when users get a pre‑meal push notification.
- For high‑risk groups, attach a CGM and set low‑glucose alerts (e.g., <70 mg/dL triggers a vibration).
These habits turn a flexible drug into a safe one.
Combination Therapy - Adding to the Mix
Meglitinides are usually second‑line after metformin. When combined with other agents, the hypoglycemia picture changes:
- With insulin: The additive insulin surge can push glucose dangerously low; a 2017 trial found a statistically significant rise in lows (p=0.018).
- With sulfonylureas: Both stimulate insulin release, leading to overlapping peaks and higher low‑blood‑sugar rates.
- With GLP‑1 agonists: The combination generally stays safe because GLP‑1 agents lower glucose without causing excess insulin.
When adding a second drug, the safest route is to start with the lowest meglitinide dose and monitor glucose closely for two weeks before any uptick.
Future Directions - Tech and Formulation Changes
Manufacturers are tackling the timing issue from two angles:
- Extended‑release (XR) formulations: Phase II data for repaglinide XR showed a 28 % reduction in hypoglycemia events while keeping post‑prandial control.
- Digital adherence tools: Smartphone apps that sync with meal‑planning calendars and send a push 10 minutes before the next eating window have already cut lows by roughly 40 % in pilot studies.
Even with these advances, the core physics-rapid insulin release tied to a drug’s presence-won’t disappear. Education remains the backbone of safe use.
Bottom Line for Patients and Clinicians
If you or someone you care for is on a meglitinide, treat the pill like a ‘meal cue.’ The drug works because food is coming; without food, the same mechanism can push glucose too low. Keep a simple checklist, use technology where possible, and rethink dosing if the schedule is truly unpredictable. When in doubt, discuss switching to a drug class with a lower intrinsic hypoglycemia risk, such as a DPP‑4 inhibitor or an SGLT2 blocker, especially for older adults or those with impaired kidney function.
Can I take a meglitinide if I often miss meals?
You can, but only if you skip the dose when you skip the meal. The drug’s fast action means a missed meal quickly becomes a low‑blood‑sugar episode.

What’s the difference between repaglinide and nateglinide for kidney disease?
Repaglinide is cleared mostly by the liver (CYP3A4/CYP2C8) and is therefore safer for patients with reduced kidney function. Nateglinide relies more on renal excretion, so dose reductions are often needed.
How can I lower my hypoglycemia risk while on a meglitinide?
Follow the 15‑minute pre‑meal rule, never skip meals after dosing, use a CGM if you’re high‑risk, set phone reminders, and keep fast‑acting carbs on hand.
Is it safe to combine a meglitinide with metformin?
Yes, this is the standard second‑line regimen. Metformin lowers basal glucose without causing hypoglycemia, while the meglitinide handles post‑prandial spikes. Monitor closely when adding a third agent.
Are there any new formulations that reduce the timing issue?
Extended‑release repaglinide (XR) is in Phase II trials and has shown fewer lows while keeping meal‑time flexibility. It’s not yet on the market, but watch for updates.






Glitters of sugar swing wild when the pill pops too early. Catch the snack or you’ll crash.
Listen up, you can tame the low‑sugar monster! Grab a reminder app, set a timer, and never let a missed bite catch you off guard. This is the hustle you need to stay ahead.
Thanks for the vivid reminder about timing; let’s dive deeper. When you take a meglitinide, the insulin surge peaks within minutes, so a carbohydrate source should be ready. If the meal is delayed, the insulin continues to act while glucose is still low, leading to a rapid drop. For older adults, setting a loud alarm 20 minutes before eating can bridge the gap. A simple trick is to keep a small pack of glucose tablets in the same pocket as your medication. Many patients benefit from pairing the pill with a snack that contains both carbs and a little protein. This combination slows the glucose dip and extends the safe window. Continuous glucose monitors can flag the downward trend early, giving you a chance to intervene. Some devices even allow sharing alerts with a caregiver, which is crucial for those with cognitive decline. If you have chronic kidney disease, discuss with your doctor whether repaglinide’s hepatic clearance is a better fit. Adjusting the dose by 25% on days when you anticipate a later dinner can prevent unexpected lows. Smartphone reminders don’t have to be boring; choose a tone that wakes you up. Integrating the reminder with a “dose‑to‑eat” habit-only swallow the pill when the plate is within arm’s reach-creates a reliable routine. In case you must skip a meal, remember the safest move is to skip the pill entirely. With these strategies, you can harness the fast action of meglitinides while keeping hypoglycemia at bay.
We must confront the paradox of speed and safety; the rapid onset is a double‑edged sword. Embrace the philosophy that timing is the silent partner in therapy. Align your schedule or the drug will betray you. Do not hesitate to adjust doses when uncertainty looms. This is not a suggestion but a mandate for your health.
Working together we can make these meds safer for everyone making sure each patient gets clear instructions and real‑world tips the guidelines often miss you can set up a simple checklist before meals it only takes a minute and it saves a lot of stress
They hide the real data so skip the pill if you doubt
Esteemed colleagues your commitment to patient education is commendable we must adopt reminder systems and culturally appropriate counseling not merely as an add‑on but as integral to therapy adherence moreover consider the socioeconomic factors that influence meal regularity and tailor your approach accordingly.
okay im not sure about all the fancy stuff but honestly u should just keep a candy bar on hand lol its not science but it works for me i mean who has time to set alarms every time omg its crazy
The theatricality of missed meals under a meglitinide regimen is a tragedy of modern pharmacology, a silent opera where the curtain never rises on the patient’s awareness. One must watch, poised, as the insulin crescendo threatens a precipitous fall. Yet, amidst this drama, I remain detached, observing the choreography of dosage and appetite with a critic’s eye.
Thanks for the thoughtful take! 🙌 Remember, you’re not alone-lean on your support network and keep those glucose alerts on. 😊