If you're taking levothyroxine for hypothyroidism, and you also take calcium or iron supplements, you might be unknowingly reducing your medication’s effectiveness. This isn’t a minor concern-it’s a well-documented interaction that can throw your thyroid levels out of balance, leading to fatigue, weight gain, brain fog, and even heart problems over time. The good news? It’s completely avoidable with simple timing changes.
Why Calcium and Iron Mess With Thyroid Meds
Levothyroxine, the most common thyroid hormone replacement, needs to be absorbed in your small intestine to work. But when calcium or iron enters your gut at the same time, they bind to the medication like magnets. These minerals-especially calcium carbonate and ferrous sulfate-form insoluble complexes that your body can’t absorb. That means your thyroid meds pass right through you, useless.
Studies show this isn’t theoretical. One 2000 study found that taking 1,200 mg of calcium carbonate with levothyroxine cut absorption by 22% to 36%. Another study in 2008 showed iron supplements reduced absorption by 21%. Even smaller doses matter: 325 mg of iron (a typical tablet) is enough to interfere. And it’s not just pills-calcium-fortified orange juice, almond milk, or soy milk can have the same effect. An 8-ounce glass of fortified OJ contains about 350 mg of calcium, enough to disrupt your meds if taken too close.
What the Guidelines Say
Major medical groups agree: don’t take calcium or iron with your thyroid medication. But they don’t all agree on how long to wait.
- The American Thyroid Association and Mayo Clinic recommend waiting at least four hours after taking levothyroxine before consuming calcium or iron.
- The European Thyroid Association says two to three hours is enough for calcium, and two hours for iron.
- The American Association of Clinical Endocrinologists warns that iron taken within two hours of levothyroxine can reduce absorption by up to 39%.
So what’s the safest bet? Go with the strictest rule: wait four hours. That way, you’re covered no matter which guideline your doctor follows. And if you’re unsure, ask for a TSH test after adjusting your routine-your levels will tell you if it’s working.
Real-Life Scenarios That Break the Rules
Most people don’t realize how easy it is to mess this up.
Take Sarah, 58, who takes levothyroxine every morning before breakfast. She also takes a calcium supplement for osteoporosis and an iron pill for anemia. She takes them both with her coffee and cereal at 7 a.m. Her TSH jumped from 2.1 to 7.8 in six months. Her doctor thought her dose was too low-until she found out about the supplement timing. After switching her calcium to bedtime and iron to lunch, her TSH dropped back to 2.4 in eight weeks.
Or Maria, 32, who just had a baby. She started iron supplements for postpartum anemia and kept taking her thyroid pill in the morning. Her TSH climbed to 8.2. Her OB-GYN didn’t know the interaction. Her endocrinologist did. She moved her iron to dinner and her thyroid pill to bedtime. Her levels normalized in six weeks.
Even bedtime dosing can help. A Reddit thread from a user named u/HypoMama shared how switching her levothyroxine from morning to right before bed eliminated her absorption issues-because she took her iron at lunch and calcium at dinner. No more spikes in TSH.
Other Things That Interfere (And What to Do)
Calcium and iron aren’t the only culprits. Here’s what else can block your thyroid meds:
- Soy products (tofu, soy milk, edamame) - can increase your levothyroxine dose needs by 18-30%. Avoid within 3-4 hours of taking your pill.
- Walnuts - one study showed they reduce absorption by 24%. Skip them for at least four hours after your dose.
- High-fiber foods (oats, beans, bran) - eating more than 30g of fiber within an hour of your pill can raise TSH by 15-25%.
- Coffee and tea - tannins and other compounds interfere. Wait at least 60 minutes after taking your pill before drinking either.
- Grapefruit juice - affects how your liver processes thyroid meds. Avoid entirely if you’re on levothyroxine.
- Biotin - found in hair/skin supplements. At doses over 5 mg/day, it can give you false lab results, making your thyroid look overactive when it’s not. Stop it at least 48 hours before blood tests.
Bottom line: take your thyroid pill with water only. Wait 30-60 minutes before eating or drinking anything else. Then wait another four hours before taking calcium, iron, or any of the other offenders.
Who’s Most at Risk?
You’re more likely to run into this problem if you:
- Are over 60 (higher chance of osteoporosis and calcium supplements)
- Are a woman of childbearing age (iron for periods or pregnancy)
- Are pregnant or postpartum (iron needs spike)
- Have multiple chronic conditions (like hypothyroidism + anemia + osteoporosis)
One 2023 study found that only 42% of patients were properly counseled about these interactions when they first started levothyroxine. That’s a huge gap. If your doctor didn’t mention it, you’re not alone-but now you know.
What If You Can’t Wait Four Hours?
Life isn’t perfect. Sometimes you’re on the go, or you forget. If you accidentally take calcium or iron with your thyroid pill, don’t panic. Skip the next dose if it’s within a few hours, and get back on schedule. But don’t double up later-that can cause side effects.
There’s also emerging hope. Newer liquid levothyroxine formulations are being tested to resist mineral binding. One study showed only an 8% drop in absorption with calcium, compared to 32% with standard tablets. But these are expensive-around $350 a month versus $15 for generics. For now, timing is still your best tool.

How to Get It Right
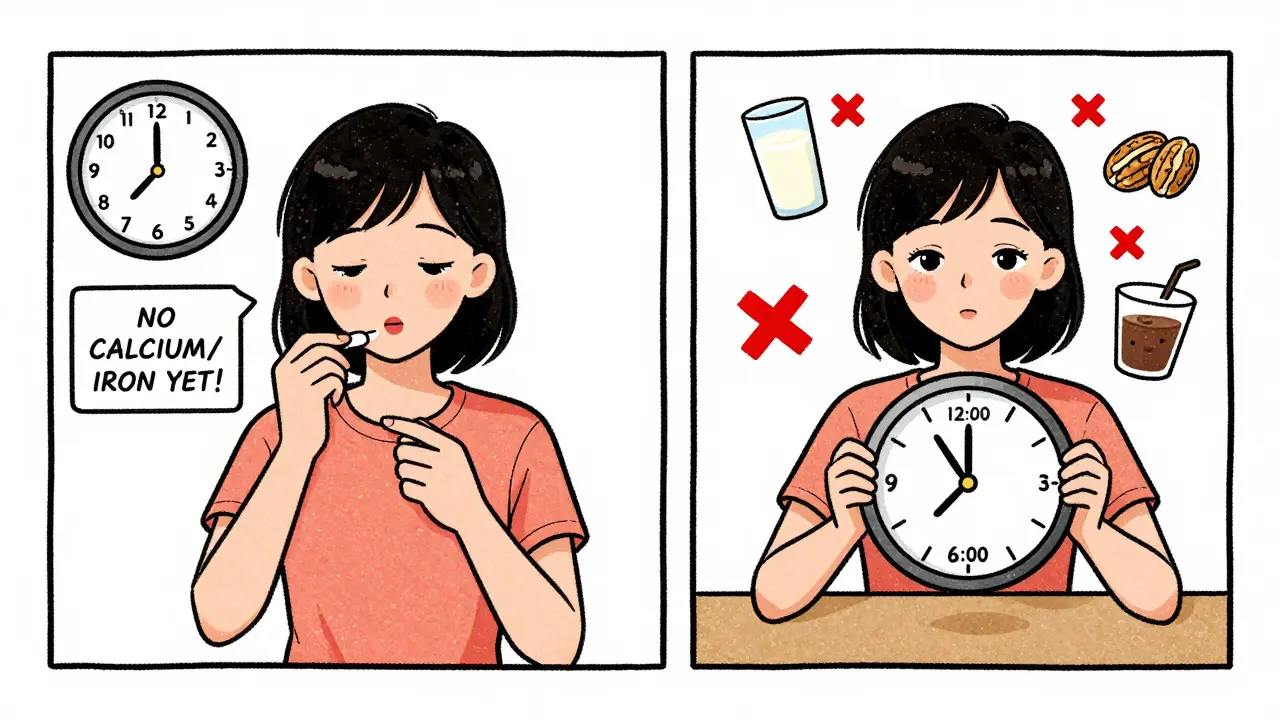
Here’s a simple daily plan that works for most people:
- Morning (7 a.m.): Take levothyroxine with a full glass of water. Wait 60 minutes before eating, drinking coffee, or tea.
- Breakfast (8 a.m.): Eat normally. Avoid soy, walnuts, or high-fiber cereals.
- Lunch (12 p.m.): Take your iron supplement.
- Dinner (6 p.m.): Take your calcium supplement.
- Bedtime (10 p.m.): Optional: Take levothyroxine at night if your doctor approves. This can make timing easier-no food or supplements interfere.
Many patients find nighttime dosing easier. Just make sure you haven’t eaten for at least three hours and that your iron or calcium isn’t still in your system. Talk to your doctor before switching timing.
When to Get Tested
If you’ve changed your supplement routine, get your TSH checked in 6-8 weeks. That’s how long it takes for your body to stabilize. If your TSH is still high (above 4.5-5.0 mIU/L), your dose may need adjusting. Don’t wait for symptoms to get worse.
And if you’re on biotin? Stop it for 48 hours before any thyroid blood test. Otherwise, your results could be misleading, and your doctor might think you’re hyperthyroid when you’re not.
Final Tip: Write It Down
Keep a simple note on your phone or fridge:
- Thyroid med: morning or night, on empty stomach, water only
- Wait 60 min before food/drinks (except water)
- Wait 4 hours before calcium or iron
- Watch for soy, walnuts, fiber, coffee, grapefruit, biotin
Thyroid medication works great-when it’s absorbed. Calcium and iron aren’t the enemy. They’re just timing troublemakers. Fix the schedule, and your energy, mood, and health will follow.
Can I take calcium and iron together with my thyroid medication if I space them out?
No. Even if you take calcium and iron at different times, both interfere with levothyroxine absorption. The safest approach is to wait at least four hours after taking your thyroid medication before taking either supplement. Taking them together doesn’t reduce the risk-it just adds another variable that can go wrong.
Is it okay to take thyroid medication at night instead of in the morning?
Yes, many patients find nighttime dosing easier. Studies show absorption is just as effective when taken at bedtime, as long as you haven’t eaten for at least three hours and you avoid iron or calcium supplements within four hours. This can simplify your routine-especially if you take multiple supplements during the day.
What if I forget and take my calcium with my thyroid pill?
Don’t double up on your next dose. Just skip the next one if it’s within a few hours, then return to your regular schedule. One mistake won’t ruin your treatment, but doing it regularly will. Monitor your symptoms and get your TSH checked in 6-8 weeks to make sure your levels are back on track.
Do all forms of calcium and iron interfere the same way?
Yes. Calcium carbonate, calcium citrate, ferrous sulfate, ferrous fumarate, and ferrous gluconate all interfere with levothyroxine absorption. The type doesn’t matter-only the mineral content. Even calcium from fortified foods like orange juice or plant-based milk can cause the same problem.
Can I take a multivitamin with my thyroid medication?
Most multivitamins contain iron, calcium, or magnesium-all of which interfere. If your multivitamin has any of these, take it at least four hours after your thyroid pill. Look for a thyroid-friendly multivitamin that excludes these minerals, or take them separately. Always check the label.
How long does it take for thyroid levels to stabilize after changing supplement timing?
It usually takes 6 to 8 weeks for your body to fully adjust. TSH levels don’t change overnight. Give it time, then get tested. If your TSH is still high, your doctor may need to adjust your levothyroxine dose. Don’t assume the problem is fixed just because you changed your routine.
Are there thyroid medications that don’t interact with calcium and iron?
Standard levothyroxine tablets do. But newer liquid formulations are being developed to resist mineral binding. Early trials show much less interference-only about 8% absorption loss versus 32% with tablets. These aren’t widely available yet and cost significantly more. For now, timing remains the most reliable solution.
Why do some doctors say two hours is enough?
Some guidelines, especially in Europe, suggest two to three hours is sufficient based on smaller studies. But the American Thyroid Association and Mayo Clinic recommend four hours because it’s more consistent across populations. When in doubt, go with the longer window-it’s safer. Your thyroid levels will thank you.










Wait, so you're telling me Big Pharma doesn't want us to know that calcium and iron are secretly working with the government to sabotage thyroid meds? I've been taking my levothyroxine at 7 a.m. and my calcium at 8 p.m. - but what if they're syncing through the WiFi in my fridge? I read somewhere that 5G towers amplify mineral binding. I'm switching to distilled water and a Faraday cage for my pill bottle. Just saying.
Also, did you know soy milk is a CIA operation? My neighbor's almond milk had a QR code that linked to a patent filed in 2003. Coincidence? I think not.
You misstate the mechanism. Levothyroxine does not merely 'bind' to calcium or iron - it forms insoluble chelates via ionic interactions between the carboxyl groups of thyroxine and divalent cations. The clinical significance is not 'minor,' as you imply, but pharmacokinetically profound. Absorption reduction of 21–36% is not a suggestion - it's a clinically validated deviation from therapeutic thresholds.
Furthermore, your recommendation to 'wait four hours' is not 'the safest bet.' It is the only evidence-based protocol supported by multiple randomized controlled trials, including those published in JCEM and Thyroid. The European guidelines are methodologically inferior due to smaller sample sizes and lack of TSH endpoint standardization. Please correct your post.
There is a deeper truth here beyond pharmacokinetics. The human body, in its ancient wisdom, was never designed to ingest synthetic hormones alongside mineral supplements in the same day. We once lived by the rhythm of sun and soil, not by pill schedules dictated by corporate pharmacies.
Perhaps the real question is not 'when' to take these substances, but whether we should be taking them at all. Is hypothyroidism a medical condition - or a signal from our bodies that we have lost touch with natural cycles? The fact that we need to wait four hours between a pill and a mineral speaks volumes about the fragility of our modern existence.
Still, I respect the practicality of your advice. Timing may be the only bridge between our broken systems and the health we seek. Let us not forget, however, that medicine is not just chemistry - it is also harmony.
Pharmacokinetic interference is well-characterized in the literature, with Cmax and AUC reductions for levothyroxine being statistically significant (p < 0.001) when co-administered with ferrous sulfate or calcium carbonate. The bioavailability cliff occurs within the first 20 minutes post-ingestion - hence the 4-hour window is not arbitrary, it's the pharmacodynamic half-life of intestinal binding kinetics.
Also, biotin interference with immunoassays is a documented pre-analytical error. Labs don't flag it. Patients don't disclose it. Endocrinologists are left guessing. This is a systemic failure in clinical communication, not a patient education gap.
THIS IS A COVER-UP. The FDA knew about this interaction since 1997. They buried the data because they make billions selling thyroid meds AND calcium supplements. You think your 'four-hour rule' is magic? It's a Band-Aid on a hemorrhage.
My cousin took her iron at lunch, calcium at dinner, thyroid at 7 a.m. - TSH still spiked. Why? Because the supplements were made in China and contain lead and aluminum that bind even faster. You think your 'fortified orange juice' is safe? It's laced with glyphosate to make you crave more supplements. Wake up.
They don't want you healthy. They want you dependent. And now you're waiting four hours like a good little drone while the real problem - corporate greed - goes unchecked.
Oh, how darling. You've written a 2,000-word essay on supplement timing like it's a TED Talk. How quaint. I suppose you also believe in brushing your teeth with toothpaste instead of just chewing the tube?
But darling, if you're taking calcium AND iron AND soy milk AND biotin AND coffee AND walnuts, you're not managing hypothyroidism - you're running a pharmaceutical buffet. Honestly, if you can't follow a 4-hour window, maybe you shouldn't be on meds at all. Some of us just take one pill, one time, and live.
Also, nighttime dosing? How gauche. I take mine at dawn, with a single drop of lemon water, and meditate for 10 minutes. It's not just chemistry - it's ritual.
Everyone's acting like this is some groundbreaking revelation. I've been taking my thyroid med at night for three years. My calcium? At breakfast. Iron? At lunch. TSH has been 1.8 for 28 months. No one's perfect. The guidelines are suggestions, not commandments.
Also, why are we assuming everyone has the luxury of a 4-hour buffer? I work two jobs. I have three kids. I take my pill with my coffee because it's the only time I'm not running. And guess what? I'm fine. Maybe your body's different. Maybe mine just doesn't care.
Wait so... I can just take my thyroid med at night and then eat my soy milk and iron gummies before bed?? 😍 I’ve been doing that for months and I feel AMAZING. My hair is thick, my brain is clear, and my cat even purred louder. Maybe the whole 4-hour rule is just a scam to sell more pills? 🤔 #ThyroidHacks #NighttimeWins
Thank you for this thorough breakdown. In Japan, we have a concept called 'kansha' - gratitude for small, consistent actions. Taking your thyroid medication with water, waiting, and respecting your body’s rhythm isn’t just medical advice - it’s self-care as a daily practice.
Many patients here use ceramic pill boxes labeled with morning, lunch, dinner, and night. No fancy apps. No alarms. Just quiet discipline. It’s not about perfection - it’s about returning to the rhythm, again and again.
And for those who forget? One missed dose won’t break you. But showing up, gently, day after day? That’s what heals.