Nebulizers vs. Inhalers: Which One Actually Works Better?
If you or someone you care for uses respiratory medication, you’ve probably faced this choice: nebulizer or inhaler? Both deliver drugs straight to the lungs, but they’re not the same. One takes 15 minutes. The other takes 2. One is bulky and noisy. The other fits in your pocket. And yet, many people still believe the nebulizer is stronger-because they can see the mist.
The truth? For most people, the inhaler with a spacer is just as effective, faster, cheaper, and safer. But that doesn’t mean nebulizers are outdated. They still have a critical role-especially for kids, older adults, or during a serious flare-up. Let’s cut through the myths and show you exactly when each device makes sense.
How Nebulizers Work (And Why People Still Use Them)
A nebulizer turns liquid medicine into a fine mist you breathe in through a mask or mouthpiece. It’s powered by a small air compressor that pushes air through a cup holding the medication. The mist is made of particles sized between 1 and 5 microns-just right to reach deep into the lungs.
Why do people stick with nebulizers? Because they don’t require timing or coordination. You don’t have to press a button and breathe in at the same time. You just sit still, breathe normally, and let the machine do the work. That’s why hospitals use them during asthma attacks. That’s why parents of toddlers use them at home. A 2-year-old can’t coordinate an inhaler. A 78-year-old with shaky hands might struggle too.
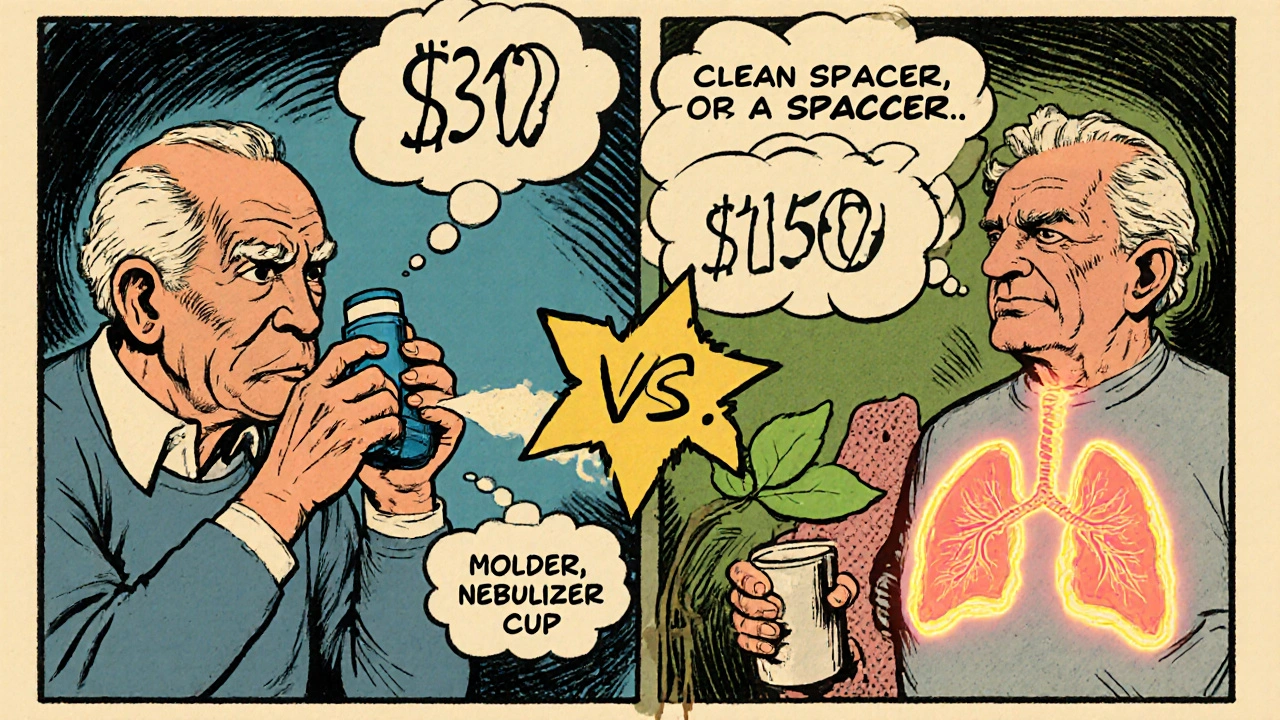
But here’s the catch: conventional nebulizers waste a lot of medicine. Studies show 60-70% of the dose gets lost during exhalation. That’s why some newer models have one-way valves-they save 30-40% more medication by only releasing mist when you inhale. Still, even the best nebulizer takes 5 to 15 minutes per treatment. And if you don’t clean it? Mold can grow in the cup. Inhaling mold spores isn’t just gross-it can trigger infections, especially in people with weak immune systems.
How Inhalers with Spacers Work (And Why Doctors Prefer Them)
An inhaler (MDI) is a small canister that sprays a puff of medicine when you press it. Alone, it’s tricky to use right. Most people press the inhaler and breathe in too late-or too early. That sends the medicine straight into the throat, not the lungs. That’s why 70-80% of adults use them incorrectly.
Enter the spacer. It’s a plastic tube with a chamber that holds the puff after you press the inhaler. You breathe in slowly from the spacer. No timing needed. The spacer catches the medicine, gives it time to settle, and lets you inhale it properly. Studies show this boosts lung delivery from 10-20% to 70-80%. It also cuts throat deposits from 80% down to 20-30%, which means fewer side effects like hoarseness or oral thrush.
A treatment with an inhaler and spacer takes 2 to 5 minutes. That’s less than half the time of a nebulizer. And it’s silent, portable, and costs way less. A basic nebulizer system runs $100-$200. An inhaler and spacer? $30-$50. Plus, you can carry them anywhere. No power outlet needed. No bulky machine. Just pop it in your bag and go.

What the Evidence Really Says
Let’s look at real data, not opinions.
A 2022 study of 99 patients, 103 doctors, and 650 nurses found that 60% of patients thought nebulizers worked better. But only 11% of doctors agreed. Nurses were split-nearly half still believed nebulizers were more effective, even though they saw the evidence.
Here’s what the science actually shows:
- Patients using inhalers with spacers improved their breathing 35% faster than those using nebulizers during asthma attacks.
- They spent 50 minutes less in the emergency room.
- They needed 40% less albuterol-less medication, same results.
- Relapse rates after two weeks were 16% lower with spacers.
And yet, patients still prefer nebulizers. Why? Because they feel like they’re getting more. They see the mist. They hear the machine. It feels like something’s happening. With an inhaler and spacer, you press a button, wait a few seconds, and breathe. It’s quiet. It’s simple. That doesn’t feel as dramatic-even though it works better.
Who Should Use What?
It’s not about which device is “better.” It’s about which one works for you.
Use a nebulizer if:
- You’re caring for a child under 5 years old
- Someone has trouble coordinating breathing and pressing a button (elderly, Parkinson’s, severe fatigue)
- You’re having a serious asthma or COPD flare-up and need high-dose treatment quickly
- You’re in a hospital or clinic setting where staff can manage the equipment
Use an inhaler with a spacer if:
- You’re an adult or child over 5 who can breathe slowly and steadily
- You want to treat symptoms at home, work, or on the go
- You’re tired of cleaning a messy machine every week
- You want to save money and reduce medication waste
And here’s a key point: children over 5 can use inhalers with spacers just fine. Many parents assume their kids need nebulizers-but with the right spacer and technique, most kids can manage it. The American Thoracic Society says spacer use improves success rates from 20% to over 90% in kids.
Cost, Maintenance, and Real-World Use
Cost isn’t just the upfront price. It’s the time, the cleaning, the wasted medicine, the trips to the ER.
Nebulizers need daily cleaning: wash the cup and mouthpiece with warm soapy water. Once a week, disinfect with a 1:3 vinegar-water solution. Skip this, and you risk mold, bacteria, or fungal growth. That’s not just inconvenient-it’s dangerous for people with lung conditions.
Inhalers need almost no maintenance. Prime them before first use (4-6 test sprays). Check the mouthpiece for blockages every few weeks. That’s it.
And let’s talk about the environment. Old inhalers used CFCs-chemicals that damaged the ozone layer. By 2009, the FDA banned them. Today, all inhalers use HFA propellants, which are safe for the planet. Nebulizers don’t use propellants, so they’re greener in that sense-but they use electricity. And if you’re using a compressor daily, that adds up.
The Future of Respiratory Delivery
Technology is changing fast. Smart inhalers now track when you use them and send reminders to your phone. One system, Propeller Health, showed a 58% drop in rescue inhaler use just by helping people stick to their plan.
Meanwhile, newer nebulizers are getting smarter too-breath-actuated models that cut waste and deliver more medicine to the lungs. But they’re still expensive, still bulky, still need power.
The trend? More people are switching to inhalers with spacers. In 2022, inhalers made up 65% of the global respiratory device market. Nebulizers? Just 25%. Why? Because evidence wins. When people see the data-faster relief, less medicine, lower cost-they change their minds.
What to Do Next
If you’re using a nebulizer and it works for you-keep using it. But ask your doctor this: Could I switch to an inhaler with a spacer? Bring your device to your next appointment. Ask them to watch you use it. If you’re a parent, ask if your child can learn to use a spacer. Most can.
Don’t let tradition or perception dictate your care. The goal isn’t to use the most dramatic device. It’s to get the right dose, into the right place, with the least effort and risk.
For most people, that’s an inhaler with a spacer. For others-kids, the elderly, or those in crisis-it’s still the nebulizer. But now you know the difference. And that’s the first step to better breathing.
Can I use a nebulizer and inhaler together?
Yes, but not usually at the same time. Some people use a nebulizer for daily maintenance if they can’t coordinate an inhaler, then switch to an inhaler with a spacer for quick relief. Others use a nebulizer during flare-ups and an inhaler for everyday use. Talk to your doctor about creating a plan that fits your needs. Never mix medications unless instructed.
Do I need a prescription for a nebulizer or inhaler spacer?
You need a prescription for the medication inside both devices. The nebulizer machine and spacer themselves are usually available over the counter, but insurance often requires a prescription to cover them. Check with your provider or pharmacy. Some Medicare and private plans cover nebulizers if you have a documented need, like COPD or severe asthma.
Are nebulizers better for COPD than inhalers?
No. Global guidelines (GINA and GOLD) say inhalers with spacers work just as well as nebulizers for COPD, even during flare-ups. Nebulizers are only preferred if the person can’t coordinate an inhaler or needs very high doses during a hospital visit. For daily management, inhalers are more practical, less expensive, and just as effective.
Why do hospitals still use nebulizers if inhalers are better?
Hospitals use nebulizers because they’re reliable during emergencies. Staff can deliver high doses quickly without relying on patient technique. In a crisis, a patient might be too breathless to coordinate an inhaler-even with a spacer. Nebulizers ensure consistent delivery under stress. But for most patients after stabilization, they’re switched to inhalers with spacers before discharge.
How do I know if I’m using my inhaler correctly?
Watch for these signs: if you taste the medicine in your throat, if your voice gets hoarse after use, or if you get oral thrush, you’re likely not getting the dose into your lungs. Ask your pharmacist to watch you use it. Or record yourself using it with your phone. Many clinics offer free technique checks. If you’re using a spacer, make sure you’re breathing in slowly over 3-5 seconds after pressing the inhaler. That’s the key.
Can I reuse a spacer?
Yes. Most spacers are designed for long-term use. Clean them monthly with warm water and mild soap. Don’t scrub the inside-this can create static that holds medicine. Just rinse and air-dry. Replace if it cracks, becomes cloudy, or doesn’t seal properly. Some spacers have valves that wear out-check the manufacturer’s guidelines.








I’ve been using an inhaler with a spacer for years and never looked back. The first time I actually did it right-slow breath, no rush-it felt like my lungs finally remembered how to work. No more throat gunk. No more cleaning a moldy nebulizer every week. Just pop it in my coat pocket and go. Simple wins.
Okay but let’s be real-nebulizers are the OGs. The mist, the hum, the drama of it all? It’s not just medical, it’s ritual. And for people with severe COPD, that 15-minute session isn’t just treatment-it’s a reset. You sit there, breathe, and for once, your body isn’t fighting you. That’s not placebo, that’s psychosomatic relief. And sometimes that’s half the battle.
Also, the 60-70% waste stat? Yeah, but newer breath-actuated nebs cut that to under 20%. They’re not dinosaurs, they’re evolving. Stop acting like tech = better.
Everyone’s so obsessed with inhalers but no one talks about how hard it is to hold one steady if you’ve got tremors from Parkinson’s or just plain old age
My grandma tried the spacer thing and she just kept missing the puff. It’s not about being lazy it’s about physical capability
Wow. Just… wow. You people are still arguing about this? The data is literally in the post. 35% faster relief. 50 minutes less ER time. 40% less albuterol. And yet-some of you still cling to the nebulizer like it’s a warm blanket from 1998. The science isn’t opinion. It’s physics. And you’re losing.
Also-mold in nebulizers? That’s not a ‘risk.’ That’s a biohazard. You’re basically inhaling a swamp. Congrats.
Bro. Inhalers are for people who can read. Like, seriously. My cousin’s 70-year-old uncle tried using one and ended up spraying half the dose on his shirt. The nebulizer? He just sat there watching TV while it did its thing. No brainpower needed. You wanna save money? Fine. But don’t pretend convenience is the same as capability.
Also-‘smart inhalers’? That’s just a fancy way of saying your meds now track you. Cool. Now my doctor knows when I’m lying about using them. Thanks for the surveillance.
My mom’s been on a nebulizer for 12 years and honestly? She’d never switch. Not because she doesn’t know better-but because she’s terrified of doing it wrong. And honestly? That fear is real. Even if the spacer works better, if you’re scared you’re gonna mess up and end up in the ER again… you stick with what feels safe.
Maybe the real win isn’t the device-it’s giving people the training, the support, the confidence to switch. Not just telling them ‘you’re doing it wrong.’
I used to think nebulizers were the only way until I saw my 8-year-old use a spacer like a PRO. She didn’t even need help. She just pressed it, breathed slow, and was back to drawing unicorns in 90 seconds. I cried. Not because I was emotional-but because I realized I’d been wasting time, money, and cleaning up a machine that was basically a noisy toaster for medicine
Also-why do hospitals still use them? Because they’re lazy. Staff don’t wanna teach. They just plug in the nebulizer and walk away. But guess what? We can do better. We just have to care enough to try.
There’s a deeper question here that no one’s asking: why do we equate visibility with efficacy? We trust what we can see-the mist, the noise, the machine whirring. But medicine doesn’t care about theater. It cares about alveolar deposition. And the spacer delivers more of the drug to the right place, with less systemic side effects. We’ve outsourced our trust to spectacle.
It’s not just about asthma. It’s about how we perceive control. The nebulizer gives the illusion of active intervention. The spacer demands quiet cooperation. One feels like a hero. The other feels like surrender. But surrender to science is still victory.
And let’s not forget the environmental math. Nebulizers run on electricity. Inhalers use HFA propellants-non-ozone-depleting, yes, but still greenhouse gases. The real winner? The breath-actuated nebulizer, if it’s powered by solar or battery. But no one talks about that. Because convenience is easier to sell than sustainability.
We’re not just choosing devices. We’re choosing philosophies of care. One is spectacle. One is precision. One is tradition. One is evidence. And the question isn’t which one works better-it’s which one we’re willing to believe.
Just got my first spacer from the pharmacy today and I’m already hooked 😊 No more throat scratch, no more waiting 15 minutes while my kid naps. I used to think nebulizers were ‘stronger’-turns out I was just using them wrong. Thanks for the post, it literally changed my routine. You guys are the real MVPs 💪