Opioid Hyperalgesia vs Tolerance Diagnostic Tool
This tool helps clinicians identify whether worsening pain in patients on long-term opioids is due to opioid-induced hyperalgesia or true tolerance. Based on the article's key clinical clues, this decision support tool calculates the probability of each condition.
Select all symptoms that apply to the patient:
Enter positive percentage if pain increased, negative if decreased. Example: Dose increased 20% and pain increased 30% = +20, +30
When patients on long‑term opioids report that their pain is getting worse instead of better, the usual first guess is “the disease is progressing.” But sometimes the culprit is a paradoxical reaction called opioid hyperalgesia. Distinguishing this from true opioid tolerance can spare patients from unnecessary dose hikes and improve outcomes. Below are the essential clues you can use at the bedside.
Understanding Opioid‑Induced Hyperalgesia
Opioid-induced hyperalgesia is a condition where prolonged opioid exposure actually heightens pain sensitivity. First described in the late‑20th century, the phenomenon gained clinical attention in the 2000s after laboratory studies repeatedly showed that certain opioids can activate pain‑facilitating pathways.
Key neurobiological players include the NMDA receptor, spinal dynorphin release, and glial cell activation. While these mechanisms are well‑documented in animal models, translating them to bedside practice remains tricky.
What Is Opioid Tolerance?
Opioid tolerance refers to a reduced response to the analgesic effects of opioids after repeated dosing. Unlike hyperalgesia, tolerance affects all opioid actions-pain relief, respiratory depression, euphoria. Clinically, tolerance shows up as a need for higher doses to achieve the same pain control.
Why the Confusion Matters
Both conditions can coexist, yet their management diverges. Mistaking hyperalgesia for tolerance often leads to dose escalation, which can worsen the pain loop. Recognizing the right pattern saves patients from higher opioid loads and reduces the risk of addiction, respiratory depression, and other side effects.
Clinical Clues that Point to Hyperalgesia
- Pain worsens despite dose increases.
- New pain areas appear-pain spreads beyond the original site.
- Qualitative change in pain (e.g., switching from dull ache to burning or shooting sensations).
- Development of allodynia-light touch triggers pain.
- Pain intensifies during stable dosing rather than during tapering, indicating independence from withdrawal.
Documenting pain location and quality at each visit-using pain drawings or digital mapping-helps spot these trends.
How to Test for Hyperalgesia
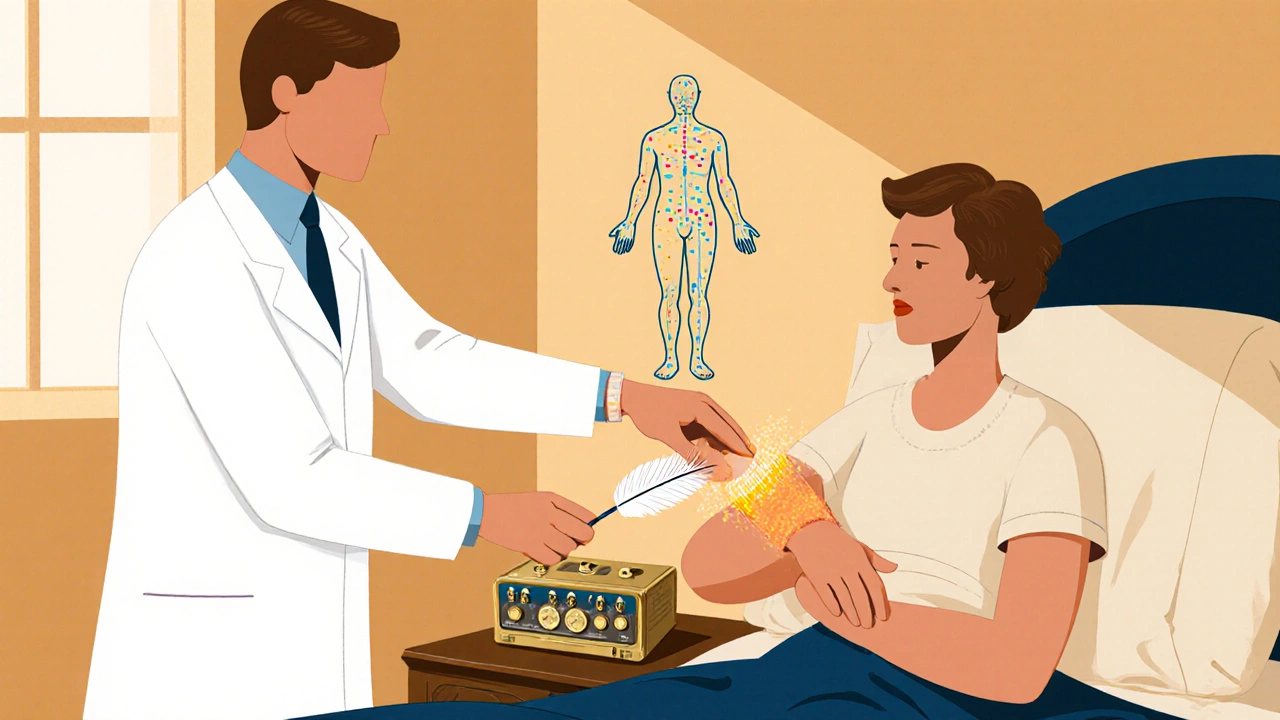
Quantitative sensory testing (Quantitative sensory testing or QST) is the most objective bedside tool. It measures thresholds for thermal, mechanical, and pressure stimuli before and after opioid dosing. A drop in threshold (i.e., increased sensitivity) after a dose suggests hyperalgesia.
In practice, combine QST with simple bedside checks: ask the patient to rate pain from a light feather touch or a warm pack applied to a non‑painful area.
Comparison Table: Hyperalgesia vs Tolerance
| Feature | Opioid‑induced hyperalgesia | Opioid tolerance |
|---|---|---|
| Primary mechanism | NMDA‑receptor activation, glial sensitization | Receptor down‑regulation, desensitization |
| Pain pattern | Worsening pain, spread to new sites, allodynia | Same pain distribution, intensity unchanged |
| Dose‑response | Higher doses increase pain | Higher doses restore analgesia |
| Typical management | Reduce dose, rotate opioid, add NMDA antagonist (e.g., ketamine) | Increase dose, consider opioid rotation |
| Diagnostic tools | QST, pain drawings, dose‑pain correlation | Clinical response to dose escalation |
Management Strategies Tailored to the Diagnosis
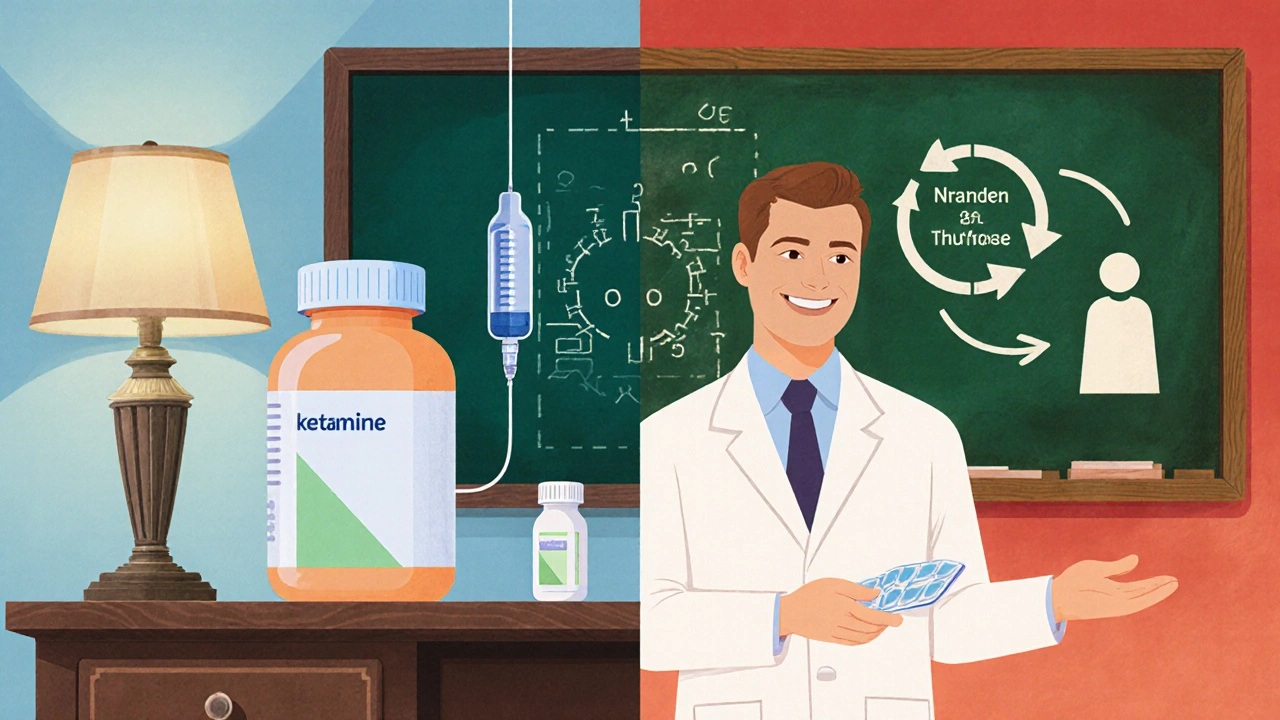
If hyperalgesia is suspected, the first step is often to lower the opioid dose or switch to a drug with lower NMDA activity (e.g., buprenorphine). Adding an NMDA antagonist such as ketamine at sub‑anesthetic levels can blunt the enhanced pain response.
For tolerance, the usual approach is dose escalation or rotating to a different opioid to reset the dose‑response curve. In many cases, both mechanisms coexist, and a combined strategy-moderate dose reduction plus rotation-yields the best result.
Guideline and Regulatory Context
The Medsafe 2021 update warned that opioids are not recommended for chronic non‑cancer pain because of safety concerns, including the risk of hyperalgesia. International bodies such as the FDA and EMA echo the same caution, urging clinicians to monitor pain trajectories closely.
The Stanford trial NCT00246532, though no longer recruiting, laid out a systematic method for teasing apart dose‑dependent hyperalgesia from tolerance across different pain modalities. Its design highlighted the need for gender‑ and ethnicity‑specific analysis-an area still under‑explored in routine practice.
The National Institute on Drug Abuse (NIDA) classifies both phenomena as barriers to effective pain control and calls for more research into biomarkers that could predict who will develop hyperalgesia.
Practical Tips for Busy Clinicians
- Chart pain location and quality at each visit-use a simple body outline.
- Track dose‑pain relationships; plot dose on the X‑axis, pain score on the Y‑axis.
- If pain escalates despite a stable or increasing dose, consider a trial reduction of 20‑30%.
- Introduce a short course of low‑dose ketamine or switch to a partial agonist (e.g., buprenorphine) when reduction alone fails.
- When in doubt, order a QST panel or refer to a pain specialist trained in sensory testing.
Future Directions
Researchers are hunting for genetic markers that predict susceptibility to hyperalgesia, and several pilot studies are testing serum cytokine panels as real‑time biomarkers. By 2030, routine screening for opioid‑induced hyperalgesia may become part of standard pain clinic intake, driven by evolving guidelines and the growing body of evidence from trials like the Stanford study.
How can I tell if a patient’s pain is worsening because of hyperalgesia or disease progression?
Look for pain that spreads to new areas, appears after dose increases, or changes quality (e.g., from throbbing to burning). Document the dose‑pain curve; if higher doses correlate with higher scores, hyperalgesia is likely.
Is quantitative sensory testing practical in a primary‑care setting?
Basic QST can be done with handheld thermal probes or pressure algometers. Even a simple tactile test (light brush on the forearm) can reveal allodynia, which is a red flag for hyperalgesia.
What role does ketamine play in treating opioid‑induced hyperalgesia?
At sub‑anesthetic doses (0.1‑0.5 mg/kg/hr), ketamine blocks NMDA receptors, dampening the neural sensitization that drives hyperalgesia. It’s often used as a short bridge while opioids are tapered.
Can opioid rotation resolve hyperalgesia?
Switching to an opioid with less NMDA activity (e.g., tapentadol or buprenorphine) can reduce hyperalgesic signaling while maintaining analgesia, especially when combined with dose reduction.
What do current guidelines say about long‑term opioid use for chronic pain?
Bodies like Medsafe, the FDA, and the American Pain Society now advise against routine opioids for chronic non‑cancer pain, highlighting risks such as tolerance, dependence, and hyperalgesia. Non‑opioid multimodal strategies are recommended first.







Opioid hyperalgesia feels like the body turning the painkillers against you.
When the dose goes up and the pain spreads, it's a red flag.
Keep a simple pain map and watch for burning or shooting sensations.
Acting early can spare the patient from a needless dose hike.
Ah, the clinical dance of hyperalgesia versus tolerance-truly a nuanced tableau, replete with paradoxes, and yet, the evidence remains stark; higher doses may exacerbate pain, whereas true tolerance restores relief, provided the physician remains vigilant, otherwise the patient merely spirals.
Documenting every dose‑pain datum is crucial.
Moreover, by integrating regular QST checks-like a light brush along the forearm-you create a dynamic picture that captures subtle shifts in sensory thresholds; this, combined with a disciplined pain drawing protocol, enables clinicians to differentiate opioid‑induced hyperalgesia from mere disease progression, thereby informing precise therapeutic adjustments without resorting to blind dose escalation, which often fuels the very phenomenon we aim to avoid.
While the article lists many points, the practical takeaway is thin; most clinicians will ignore the QST requirement and continue escalating opioids, perpetuating hyperalgesia. A more aggressive education effort is needed.
One must consider that opioid receptors are not static entities they undergo complex regulation which includes down‑regulation desensitization and also a paradoxical up‑regulation of pronociceptive pathways such as NMDA activation glial sensitization and dynorphin release this multifactorial process explains why some patients develop heightened pain sensitivity despite increasing doses a careful longitudinal assessment that maps pain quality location and dose response over time is therefore indispensable in order to separate true disease progression from a pharmacologically induced hyperalgesic state
Hyperalgesia means more pain despite more opioids.
Hey folks 😊 i think a quick light‑touch test can reveal allodynia – just swipe a soft feather on the arm and ask the patient to rate it, it’s simple and often reveals hyperalgesia early 😅
Oh great, another reminder that more opioids can sometimes make the pain worse.
The irony of opioid‑induced hyperalgesia is that the very drugs prescribed to soothe hurt end up amplifying it.
Physicians love to chase the next higher dose as if it were a magic bullet.
What they fail to realize is that NMDA receptors get excited, glial cells start screaming, and the nervous system throws a tantrum.
Meanwhile the patient sits there, reporting a burning sensation that wasn’t there before.
You could argue that this is just disease progression, but the dose‑pain correlation tells another story.
If you plot dose on the x‑axis and pain score on the y‑axis and see an upward slope, congratulations, you’ve found hyperalgesia.
The proper response, contrary to popular practice, is to step back, not to step up.
Reducing the opioid by 20‑30% often restores a sense of balance in the central pain pathways.
Adding a low‑dose NMDA antagonist such as ketamine can silence the rogue receptors.
Opioid rotation to a drug with lower NMDA activity, like buprenorphine, is another elegant maneuver.
All of these strategies avoid the reckless escalation that fuels addiction and respiratory depression.
Yet some clinicians persist in dose escalation, apparently convinced that bigger is always better.
This mindset is not only outdated, it is dangerous for the patient and wasteful for the healthcare system.
So let’s stop treating hyperalgesia with more opioids and start treating it with smarter, evidence‑based tactics.
From a clinical standpoint, differentiating opioid‑induced hyperalgesia from tolerance is paramount to optimizing patient outcomes.
The literature underscores that hyperalgesia manifests as a paradoxical increase in pain intensity despite dose escalation, whereas tolerance reflects a diminished analgesic response necessitating higher doses.
Accordingly, a systematic approach should begin with meticulous documentation of pain quality, distribution, and temporal relation to dosing.
Employing quantitative sensory testing, even in a simplified form, provides objective corroboration of sensory dysregulation.
Should the data reveal a lowering of pain thresholds concomitant with opioid administration, a therapeutic trial of dose reduction is warranted.
Concurrent consideration of an NMDA antagonist, such as low‑dose ketamine, may attenuate central sensitization.
Opioid rotation to agents with reduced NMDA affinity, notably buprenorphine, offers an additional avenue to mitigate hyperalgesic phenomena.
It is imperative that clinicians communicate these strategies to patients with clarity, ensuring informed consent and shared decision‑making.
Ultimately, vigilant monitoring and prompt adjustment of the opioid regimen can prevent the escalation of hyperalgesia and preserve analgesic efficacy.
Patriotic doctors should protect our citizens from needless opioid escalation 🇺🇸💪 Hyperalgesia is a clear sign that the system is failing, and we must act decisively, not waste time with vague tolerances 😤.
Consider the paradox: a substance meant to silence pain can become the very voice of suffering.
When the dosage climbs and the flame of pain grows brighter, we are confronted with a philosophical dilemma-do we surrender to escalation or seek equilibrium?
The answer lies in humility before neurobiology, embracing strategies that lower the dose, rotate the agent, and perhaps introduce a modest NMDA blockade.
🌟
Dear colleague, your thorough outline of hyperalgesia versus tolerance is commendable.
The emphasis on pain mapping and dose‑pain curves aligns with best‑practice guidelines.
Incorporating a brief bedside tactile assessment can further enrich the diagnostic toolkit.
I encourage continued education on NMDA antagonists, as they offer a valuable adjunct.
Together we can improve patient care.
🙏
Yo fam, gotta talk about the pharmacodyn mic stuff – when you up the µg/kg dose and the nociceptor firing spikes, you’re lookin at allodynia up‑regulin.
The NMDA portal gets lit, glial cells go cray, so you need a rotate to buprenorphin or add ketamine low‑dose.
Don't just blast the morphine, that's a surefire way to push the sens.
Keep tabs on the QST scores, they’re the real KPI for pain mod.
Your table perfectly summarizes the key differences, but I’d add that patient education is equally vital.
When patients understand that higher opioid doses might worsen pain, they’re more likely to consent to dose reductions or rotations.
Also, consider integrating non‑pharmacologic modalities-physical therapy, CBT-to complement the pharmacologic strategy.
This multimodal approach can help break the cycle of hyperalgesia.
Hyperalgesia is simply opioid‑induced pain amplification; tolerance is reduced analgesia.