Gout Medication Comparison Tool
Select Your Medication
Allopurinol
Purine-type xanthine oxidase inhibitor
Febuxostat
Non-purine xanthine oxidase inhibitor
Probenecid
Uricosuric agent
Pegloticase
IV enzyme for refractory gout
Lesinurad
Uricosuric agent with xanthine oxidase inhibitor
Medication Details
Select a medication from the list to view its details
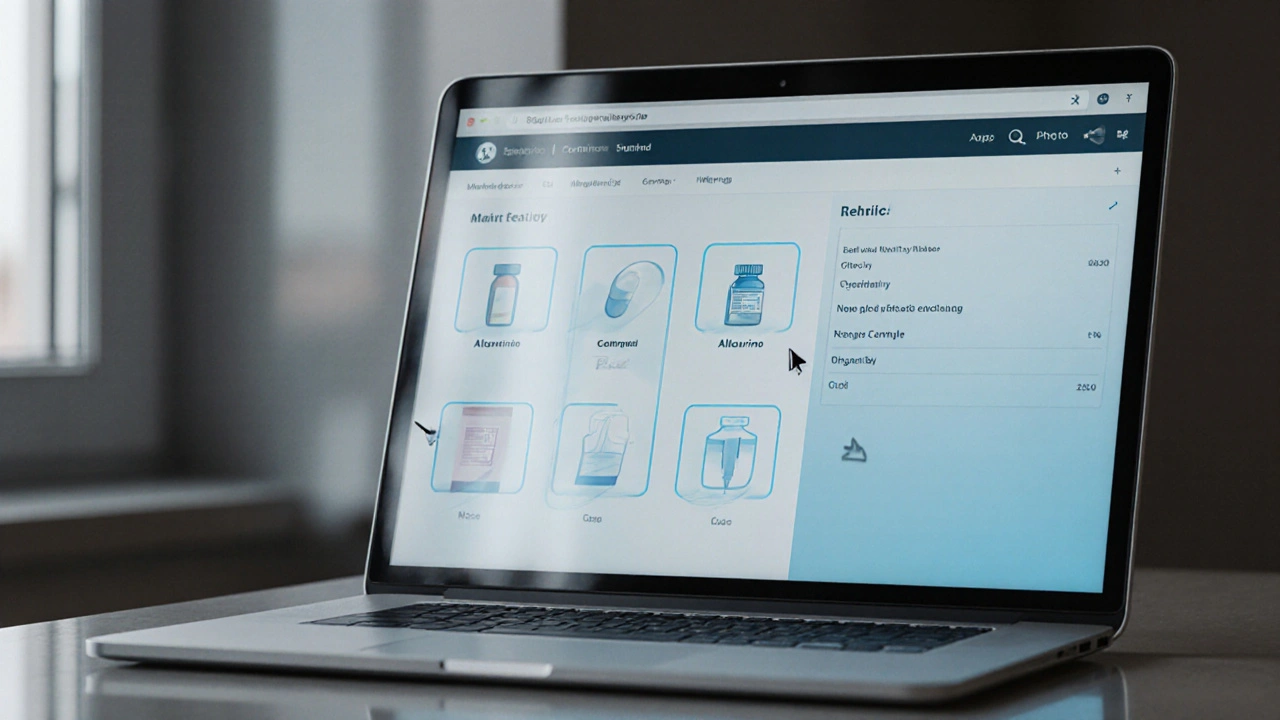
Comparison Table
| Feature | Allopurinol | Febuxostat | Probenecid | Pegloticase | Lesinurad |
|---|---|---|---|---|---|
| Drug Class | Purine xanthine oxidase inhibitor | Non-purine xanthine oxidase inhibitor | Uricosuric agent | Enzyme replacement therapy | Uricosuric agent |
| Typical Dose | 100-400 mg daily | 40-80 mg daily | 500-1000 mg daily | 8 mg IV every 2 weeks | 400 mg daily |
| Cost | Low (generic) | Moderate | Low (generic) | Very High | Moderate |
| Kidney Function | Requires dose adjustment | Minimal adjustment needed | Good function required | Not applicable | Good function required |
| Side Effects | Rash, liver enzymes | Liver toxicity, cardiovascular risk | Stomach upset, kidney stones | Allergic reactions, infusion reactions | Kidney stones, urinary tract infections |
| Special Considerations | Long-established, well-studied | Alternative if allopurinol fails | Best for good kidney function | For refractory gout only | Combination therapy option |
TL;DR
- Allopurinol works for most gout patients but needs dose adjustment in kidney disease.
- Febuxostat is a non‑purine xanthine oxidase inhibitor, useful when allopurinol isn’t tolerated.
- Probenecid increases uric acid excretion; best for patients with good kidney function.
- Pegloticase is an IV enzyme for refractory gout; high cost and infusion reactions limit use.
- Lesinurad adds uricosuric power to xanthine oxidase inhibitors but raises kidney‑stone risk.
Gout flares are painful, but the right medication can keep uric acid under control for the long haul. If you’ve been prescribed allopurinol alternatives, you’re probably wondering how they stack up. This guide walks through the chemistry, dosing, side‑effects, and real‑world considerations for the most common gout drugs, so you can match the treatment to your health profile.
What is gout and why do we need uric‑lowering drugs?
Gout is an inflammatory arthritis triggered by high levels of uric acid in the blood (hyperuricemia). When urate crystals deposit in joints, they spark sudden, throbbing pain. Keeping serum urate below 6mg/dL (or Hyperuricemia a condition where blood uric acid exceeds normal limits, often above 7mg/dL) reduces flare frequency and prevents joint damage.
Two main drug classes lower uric acid:
- Xanthine oxidase inhibitors medications that block the enzyme that produces uric acid (e.g., Allopurinol, Febuxostat).
- Uricosuric agents drugs that increase kidney excretion of uric acid (e.g., Probenecid, Lesinurad).
Choosing the right class depends on kidney health, other medicines, and how your body reacts.
Allopurinol - the classic workhorse
Allopurinol a purine‑type xanthine oxidase inhibitor approved for gout and hyperuricemia has been on the market since the 1960s. It reduces uric‑acid production by blocking the enzyme xanthine oxidase.
Typical dose: start 100mg daily, increase by 100mg every 2-4weeks up to 300mg (or 400mg in select cases) based on serum urate and renal function.
Key advantages:
- Low cost (generic price ~£0.10 per tablet in the UK).
- Well‑studied safety profile with decades of data.
- Effective for most patients when titrated properly.
Common side effects:
- Skin rash (rare but can progress to Stevens‑Johnson syndrome).
- Transient liver enzyme rise.
- Gout flare during dose escalation (prevent with prophylactic colchicine or NSAIDs).
Allopurinol is cleared by the kidneys, so Renal impairment reduced kidney function measured by eGFR, impacting drug elimination requires dose reduction. In patients with eGFR<30mL/min, a starting dose of 50mg daily is typical.
Febuxostat - the non‑purine alternative
Febuxostat a non‑purine selective xanthine oxidase inhibitor approved for gout and hyperuricemia was introduced in the early 2000s. It works similarly to Allopurinol but does not need renal dose adjustment.
Typical dose: 40mg once daily; increase to 80mg if target urate not reached after 2weeks.
Advantages:
- Effective even in moderate‑to‑severe renal dysfunction (eGFR<30mL/min).
- Lower incidence of rash compared with high‑dose Allopurinol.
- Predictable pharmacokinetics - less titration required.
Safety notes:
- FDA boxed warning for increased cardiovascular mortality (observed in high‑risk patients).
- Possible liver enzyme elevation - monitor ALT/AST.
- May cause nausea or mild allergic rash.
Cost is higher than Allopurinol (brand price ~£0.50‑£0.80 per tablet), but many UK NHS formularies list it as a second‑line option when Allopurinol cannot be used.

Probenecid - the classic uricosuric
Probenecid a uricosuric agent that blocks renal tubular reabsorption of uric acid, increasing its excretion has been used for decades, especially in patients who cannot tolerate xanthine oxidase inhibitors.
Typical dose: 250mg twice daily; may increase to 1g twice daily.
When it shines:
- Patients with normal kidney function (eGFR>60mL/min).
- Those who already have low serum urate but need a boost.
Limitations:
- Ineffective in renal impairment because it relies on tubular function.
- Increases risk of calcium‑oxalate kidney stones.
- Drug interactions with penicillins, NSAIDs, and antivirals.
Side effects include GI upset, rash, and rarely, hemolysis in G6PD‑deficient patients.
Pegloticase - the IV enzyme for refractory gout
Pegloticase a recombinant uricase enzyme given intravenously to metabolize uric acid into allantoin is reserved for chronic gout that fails to respond to oral agents.
Dosing: 8mg IV infusion every 2 weeks.
Pros:
- Rapid urate reduction (often <6mg/dL within days).
- Effective in patients with severe renal disease.
Cons:
- High price (≈£30,000 per year in the UK).
- Infusion reactions in up to 30% of patients - requires pre‑medication and monitoring.
- Development of anti‑drug antibodies reduces efficacy over time.
Because of cost and safety concerns, Pegloticase is used only after trial of xanthine oxidase inhibitors and uricosurics.
Lesinurad - the uricosuric add‑on
Lesinurad a selective inhibitor of the uric acid transporter URAT1, used in combination with a xanthine oxidase inhibitor was approved in 2015.
Typical dose: 200mg once daily together with Allopurinol or Febuxostat.
Why add it?
- Boosts uric‑acid excretion when XO inhibition alone isn’t enough.
- Helps patients on maximum tolerated XO inhibitor dose reach target urate.
Cautions:
- Increases risk of nephrolithiasis - ensure adequate hydration.
- Contraindicated in eGFR<30mL/min.
- May cause mild hepatic enzyme rise.
Cost is moderate (£0.30-£0.45 per tablet) and most UK NHS trusts cover it when combined with standard therapy.
Side‑by‑side comparison
| Drug | Class | Mechanism | Typical Dose | Renal Adjustment Needed? | Major Safety Concerns | Cost (UK, per month) |
|---|---|---|---|---|---|---|
| Allopurinol | Xanthine oxidase inhibitor | Blocks uric‑acid production | 100-300mg daily (up to 400mg) | Yes - reduce if eGFR<30mL/min | Rash, Stevens‑Johnson, hypersensitivity | ~£3 |
| Febuxostat | Xanthine oxidase inhibitor | Selectively inhibits XO without renal dose change | 40mg daily, can increase to 80mg | No | Cardiovascular risk, liver enzyme rise | ~£30 |
| Probenecid | Uricosuric | Inhibits renal reabsorption of uric acid | 250mg twice daily (up to 1g twice daily) | Yes - ineffective if eGFR<30mL/min | Kidney stones, drug interactions | ~£12 |
| Pegloticase | Uricase enzyme | Converts uric acid to allantoin | 8mg IV every 2 weeks | No | Infusion reactions, antibodies, high cost | ~£30,000 |
| Lesinurad | Uricosuric (add‑on) | Blocks URAT1 transporter, ↑ excretion | 200mg daily with XO inhibitor | Yes - avoid if eGFR<30mL/min | Kidney stones, liver enzymes | ~£15 |
How to pick the right drug for you
Consider these factors before settling on a regimen:
- Kidney function: If eGFR<30mL/min, Febuxostat or Pegloticase are safer bets than Allopurinol or Probenecid.
- Cardiovascular history: Patients with recent heart disease should discuss Febuxostat’s risk versus Allopurinol’s lower cardiovascular profile.
- Previous drug reactions: A history of rash with Allopurinol pushes you toward Febuxostat or a uricosuric if kidneys are healthy.
- Cost & insurance coverage: Generic Allopurinol remains the most affordable; Pegloticase may require special approval.
- Need for rapid control: Pegloticase achieves fast urate reduction, useful before surgery or in severe tophi cases.
Always combine the chosen drug with lifestyle changes - low‑purine diet, weight loss, limiting alcohol, and staying hydrated. For most people, a low dose of colchicine during the first 3 months of therapy helps prevent flares caused by shifting uric‑acid levels.
Frequently Asked Questions
Can I switch from Allopurinol to Febuxostat safely?
Yes, most clinicians taper Allopurinol over 1-2 weeks while introducing Febuxostat at 40mg daily. Monitor urate levels and watch for any new cardiac symptoms, especially if you have existing heart disease.
Why did my doctor add Lesinurad to my Allopurinol?
Your urate level may have plateaued at the maximum dose of Allopurinol. Lesinurad boosts uric‑acid excretion, helping you hit the <6mg/dL target without raising the Allopurinol dose.
Is Probenecid still useful in 2025?
It’s valuable for patients with normal kidney function who cannot tolerate XO inhibitors. However, its stone‑forming risk means doctors prescribe plenty of water and sometimes a low‑dose thiazide to reduce calcium oxalate precipitation.
What should I watch for while on Pegloticase?
Infusion reactions (redness, itching, shortness of breath) can appear during the first few doses. Premedicate with antihistamines and steroids, and have a nurse monitor you for at least 30minutes after each infusion. Also, labs should be checked for anti‑drug antibodies if urate levels rise unexpectedly.
Do lifestyle changes really matter when I’m on medication?
Absolutely. Even a 5‑kg weight loss can lower serum urate by 0.5mg/dL. Reducing red‑meat portions, limiting beer, and drinking at least 2L of water daily cut flare risk by up to 30%.
Choosing a gout medicine isn’t a one‑size‑fits‑all decision. By weighing kidney health, cardiovascular risk, cost, and how fast you need urate control, you can land on the regimen that keeps you pain‑free and moving.








Allopurinol stays the go‑to for most gout patients.
It’s true, the drug’s long track record gives it a safety edge, but the newer xanthine oxidase inhibitors can be useful when kidneys limit dose escalation.
From a pharmacodynamic perspective, allopurinol’s inhibition constant (Ki) demonstrates competitive inhibition, yet the dose‑response curve plateaus in patients with reduced GFR, necessitating an alternative mechanistic pathway.
oh wow, so basically if your kidneys are “meh” you might need to switch to febuxostat or a uricosuric like probenecid – but watch out for stone‑forming side effects.
One must acknowledge that febuxostat, while chemically elegant, carries a non‑trivial cardiovascular risk profile that the discerning clinician cannot ignore.
Indeed, the cardiovascular signal observed in the CARES trial invites a nuanced risk‑benefit analysis, especially for patients with pre‑existing heart disease.
In clinical practice, the cost disparity between generic allopurinol and branded febuxostat often dictates initial therapy selection.
Honestly, it’s a shame that insurance policies force patients into cheaper meds even when the premium options might prevent future joint damage.
Probenecid remains viable for patients with preserved renal function, albeit the risk of nephrolithiasis warrants monitoring.
Regular urine alkalinisation can mitigate stone formation, making probenecid a safer choice when paired with dietary advice.
Sure, just add “watch out for kidney stones” to the label and call it a day.
While the warning is necessary, patient education on hydration and urine pH can substantially reduce that risk.
Pegloticase offers a lifeline for refractory gout, delivering rapid urate reduction through enzymatic conversion. It’s administered bi‑weekly via IV, which can be logistically challenging for some patients. The high price tag often restricts usage to those with severe disease unresponsive to oral agents. Infusion reactions, ranging from mild flushing to anaphylaxis, demand pre‑medication and close monitoring. Anti‑drug antibodies may develop, reducing efficacy over time. Insurance prior‑authorization is typically required and can delay therapy initiation. Nonetheless, for desperate cases, the benefit can outweigh the burdens. Proper patient selection is key.
The clinical utility of pegloticase must be examined through a multidimensional lens that encompasses pharmacoeconomics, immunogenic potential, and patient-centered outcomes. First, the drug’s mechanism of action-recombinant uricase-circumvents the human deficiency that predisposes to hyperuricemia, thereby achieving serum urate levels well below the therapeutic threshold of six milligrams per deciliter. Second, the financial implications are nontrivial; a bi‑weekly infusion can accrue costs exceeding tens of thousands of dollars annually, pressuring both health systems and individual patients. Third, immunogenicity presents a formidable obstacle, as the formation of anti‑pegloticase antibodies correlates with an increased incidence of infusion‑related adverse events and a precipitous loss of urate‑lowering efficacy. Fourth, the requisite pre‑infusion prophylaxis, often comprising antihistamines and corticosteroids, adds layers of complexity to the treatment regimen. Fifth, monitoring protocols mandate serial measurements of serum urate and gout flare frequency to gauge therapeutic response. Sixth, the risk‑benefit calculus must weigh the profound relief of refractory gout against the potential for anaphylactic reactions, which, although rare, demand immediate medical intervention. Seventh, the patient’s quality of life may improve dramatically, as pain resolution facilitates resumed mobility and functional independence. Eighth, shared decision‑making is indispensable; clinicians should elucidate both the therapeutic promise and the logistical burdens inherent to pegloticase therapy. Ninth, ongoing clinical trials continue to explore subcutaneous formulations that may alleviate infusion‑related constraints. Tenth, health‑policy frameworks should strive to streamline authorization pathways to prevent undue treatment delays. Eleventh, interdisciplinary coordination among rheumatologists, pharmacists, and infusion centers optimizes safety and adherence. Twelfth, patient education regarding signs of hypersensitivity can empower early detection and mitigation of severe reactions. Thirteenth, insurance coverage variability necessitates proactive advocacy on behalf of the patient. Fourteenth, long‑term data on renal outcomes remain limited, highlighting an area for future research. Fifteenth, comparative effectiveness studies juxtaposing pegloticase with emerging oral agents will refine therapeutic hierarchies. Finally, the synthesis of these considerations underscores that pegloticase remains a potent, albeit resource‑intensive, option reserved for a select cohort of individuals who have exhausted conventional modalities.
For most folks, starting with allopurinol and titrating upward while using colchicine prophylaxis works well.
The incremental dose‑adjustment algorithm should be guided by periodic serum urate assessments, thereby ensuring optimal therapeutic thresholds are achieved.
Lesinurad, when combined with a xanthine oxidase inhibitor, offers synergistic urate reduction but mandates vigilant surveillance for nephrolithiasis, particularly in patients with borderline renal function.
So the take‑away is: pair lesinurad with allopurinol or febuxostat, stay hydrated, and keep an eye on kidney labs.