Avandia vs. Type 2 Diabetes Drugs Comparison Tool
Drug Comparison Results
Select a drug and your health condition to see detailed comparison information.
Key Attributes of Avandia
- Class: Thiazolidinedione
- HbA1c Drop: 0.8–1.2%
- Weight Impact: +2–4 kg
- Cardiovascular Risk: High
- Cost (UK): ~£30/month
- Side Effects: Fluid retention, bone fractures
Why Avandia Is Still Used
Despite safety concerns, Avandia can still be effective for patients who have tried multiple other therapies and cannot tolerate them.
It is particularly useful in patients with severe insulin resistance or those needing rapid glycemic control.
When you or a loved one need to control blood sugar, the list of prescription options can feel endless. Avandia (generic name Rosiglitazone is a thiazolidinedione (TZD) that improves insulin sensitivity by activating the PPARγ receptor) was once a go‑to choice for many clinicians, but safety concerns and newer drugs have reshaped the market. This article lines up Avavndia against the most common alternatives, so you can see where each one shines and where it falls short.
Key Takeaways
- Avandia lowers HbA1c by 0.8‑1.2% but carries a higher risk of heart failure and fluid retention.
- Pioglitazone offers similar efficacy with a slightly better cardiovascular safety profile, though it can cause weight gain.
- Metformin remains the first‑line therapy for most patients because of its low cost, weight‑neutral effect, and proven reduction in cardiovascular events.
- SGLT2 inhibitors (e.g., Empagliflozin) and GLP‑1 agonists (e.g., Liraglutide) provide extra benefits like weight loss and heart‑failure protection, but they are pricier.
- Choosing the right drug depends on your kidney function, heart health, cost considerations, and personal preferences.
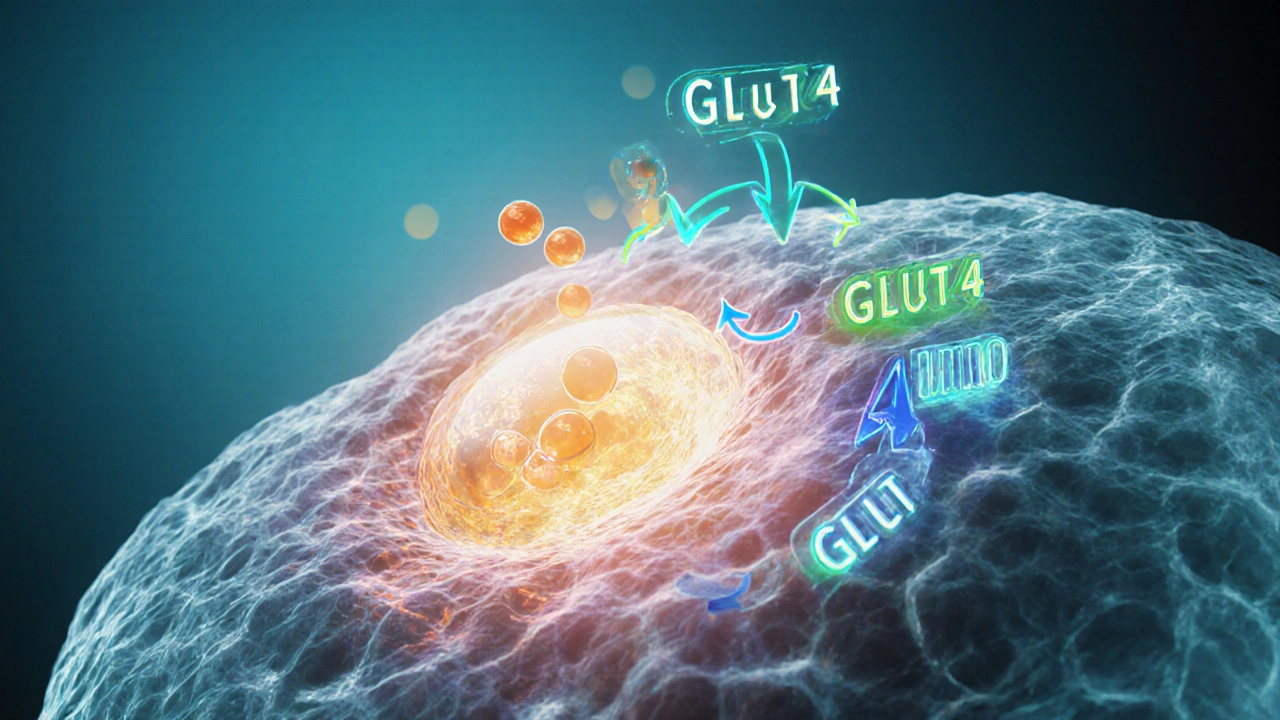
How Avandia Works
Rosiglitazone acts on the peroxisome proliferator‑activated receptor gamma (PPARγ), a nuclear receptor that tells fat cells to store more fatty acids and become more responsive to insulin. By making peripheral tissues more insulin‑sensitive, the drug helps lower fasting glucose without stimulating the pancreas to produce more insulin.
Typical dosing starts at 4mg once daily, with a possible increase to 8mg. The drug is taken with or without food, and steady‑state concentrations are reached within 2‑3 weeks.
Safety Profile and Controversies
In 2007 the Food and Drug Administration (FDA) issued a boxed warning after meta‑analyses suggested a 2‑3‑fold rise in myocardial infarction risk. The agency later required a risk‑evaluation and mitigation strategy (REMS) and limited the drug’s use to patients who could not achieve control with other agents.
Common side effects include:
- Fluid retention leading to edema
- Weight gain (average 2‑4kg)
- Increased risk of bone fractures in women
Because of the cardiovascular risk profile, clinicians often reserve Avandia for patients with robust cardiac monitoring or for those who have failed multiple other agents.
Major Alternatives on the Market
Below is a quick snapshot of the most widely prescribed alternatives.
- Pioglitazone another thiazolidinedione that shares the PPARγ mechanism but has a slightly lower heart‑failure signal.
- Metformin biguanide that decreases hepatic glucose production and improves peripheral insulin sensitivity; first‑line per ADA guidelines.
- Empagliflozin SGLT2 inhibitor that forces glucose out through the urine, also lowers blood pressure and reduces heart‑failure hospitalization.
- Sitagliptin DPP‑4 inhibitor that prolongs incretin action, modest HbA1c reduction with low hypoglycemia risk.
- Liraglutide GLP‑1 receptor agonist injected daily; promotes weight loss and carries proven cardiovascular benefit.
Side‑by‑Side Comparison Table
| Drug | Class | Typical HbA1c drop | Weight impact | Cardiovascular safety | Cost (UK, £/month) | Common concerns |
|---|---|---|---|---|---|---|
| Avandia (Rosiglitazone) | Thiazolidinedione | 0.8‑1.2% | +2‑4kg | ↑ heart‑failure, ↑ MI risk | ~£30 | Fluid retention, bone fractures |
| Pioglitazone | Thiazolidinedione | 0.7‑1.1% | +1‑3kg | Neutral to slight ↑ CV risk | ~£25 | Bladder cancer warning (long‑term) |
| Metformin | Biguanide | 0.6‑1.0% | Weight‑neutral or ↓ | ↓ CV events (large outcome trials) | ~£5‑10 | GI upset, rare lactic acidosis |
| Empagliflozin | SGLT2 inhibitor | 0.5‑0.8% | ↓ 1‑3kg | ↓ HF hospitalization, ↓ CV death | ~£70 | UTIs, genital infections, ketoacidosis |
| Sitagliptin | DPP‑4 inhibitor | 0.5‑0.7% | Weight‑neutral | Neutral CV risk | ~£60 | Pancreatitis (rare) |
| Liraglutide | GLP‑1 agonist | 0.8‑1.4% | ↓ 2‑5kg | ↓ CV events, ↓ stroke | ~£120 | Injection site reactions, nausea |
Choosing the Right Agent for You
When you sit down with your clinician, ask about three practical factors:
- Heart health: If you have a history of heart failure or coronary disease, Avandia’s cardiovascular warnings usually push it down the list. Empagliflozin or Liraglutide may be safer bets.
- Kidney function: Metformin is contraindicated when eGFR <30mL/min/1.73m², while SGLT2 inhibitors lose efficacy below eGFR 45. Pioglitazone and DPP‑4 inhibitors are generally safe down to 30.
- Cost and access: Generic Metformin and Pioglitazone are cheap on the NHS. Newer agents often require special formularies or private insurance.
For many patients, a combination works best. A common regimen is Metformin + a GLP‑1 agonist for strong glucose control plus weight loss, adding a low‑dose TZD only if HbA1c remains stubbornly high.
Common Pitfalls and How to Avoid Them
- Ignoring fluid retention: If you notice swelling in the ankles after starting Avandia, call your doctor right away. Reducing sodium intake and adding a diuretic can help, but often the drug is dropped.
- Skipping renal monitoring: SGLT2 inhibitors need a baseline eGFR check. Failure to monitor can lead to unexpected ketoacidosis.
- Assuming “one‑size‑fits‑all”: The same drug class can behave differently across ethnicities. For instance, Asian patients often experience more GI upset on Metformin and may need a slow titration.
- Overlooking drug interactions: Avandia can increase plasma levels of CYP2C8 substrates like paclitaxel. Always review your full medication list.
Frequently Asked Questions
Is Avandia still prescribed in the UK?
Yes, but only under strict NHS guidelines. It’s typically a third‑line option after metformin, a sulfonylurea, or an SGLT2 inhibitor, and the prescriber must document why alternatives aren’t suitable.
How does the heart‑failure risk of Avandia compare to Pioglitazone?
Both drugs can cause fluid retention, but large post‑marketing studies show Pioglitazone has a slightly lower incidence of hospitalised heart failure (about 0.8% vs. 1.2% for Avandia). The difference is modest, yet clinically relevant for patients with existing cardiac issues.
Can I switch from Avandia to Metformin?
Switching is possible, but you’ll need a wash‑out period of 48‑72hours to avoid overlapping side effects. Your doctor will usually start Metformin at a low dose (500mg) and titrate up while monitoring blood glucose.
What monitoring is required while on Avandia?
Baseline and quarterly liver function tests, fasting lipid panel, and an echocardiogram if you have a history of heart disease. Also check for weight gain and edema at every visit.
Are there any patient groups that should avoid Avandia completely?
Pregnant or breastfeeding women, patients with NYHA class III/IV heart failure, and anyone who has had a recent myocardial infarction should not use Avandia. In such cases, clinicians prefer Metformin combined with a GLP‑1 agonist or SGLT2 inhibitor.
Bottom Line
Avandia can still be useful, but its cardiac safety signals make it a niche choice. Most patients achieve comparable or better glucose control with cheaper, safer drugs like Metformin, Pioglitazone, or the newer SGLT2/GLP‑1 classes. Always weigh heart health, kidney function, and budget before settling on a regimen.










One must recognize that the pharmaceutical hierarchy perpetuates a grotesque illusion of choice, and Avavndia's revival is nothing short of academic hubris!
When assessing the comparative data, it’s useful to keep the patient’s individual context front‑and‑center. The tables outline efficacy, but the nuanced side‑effect profiles-especially fluid retention-require clinicians to weigh risks against lifestyle priorities. Moreover, cost considerations can dramatically shift the therapeutic hierarchy, especially for those without comprehensive insurance coverage.
Choosing a glucose‑lowering agent is less about chasing the flashiest headline and more about constructing a sustainable partnership between drug, doctor, and patient; each medication carries its own story of benefits and trade‑offs. Avandia, with its pronounced insulin‑sensitising power, can indeed bring a respectable HbA1c drop of up to 1.2 %, which is valuable for individuals wrestling with severe insulin resistance. Yet this potency arrives bundled with a propensity for fluid retention, modest weight gain, and a heightened signal for heart‑failure events that cannot be ignored. In contrast, metformin delivers a modest reduction-often around 0.8 %-while actively shedding pounds or at least not adding to the scale, and it enjoys a well‑documented record of lowering cardiovascular mortality. SGLT2 inhibitors such as empagliflozin not only trim sugars but also shave off a few kilograms and dramatically cut the risk of hospitalization for heart failure, albeit at a steeper price tag that many health systems still grapple with. GLP‑1 agonists, exemplified by liraglutide, weave together weight loss, glycaemic control, and cardiovascular protection, though their injectable nature and cost can be barriers for some patients. Pioglitazone mirrors Avandia’s mechanism but treads more lightly on the cardiovascular risk graph, though it carries a long‑term bladder‑cancer warning that necessitates vigilant monitoring. When kidney function declines, metformin’s traditional contraindication emerges, steering clinicians toward agents like SGLT2 inhibitors or cautious dose adjustments. For those whose primary concern is weight, DPP‑4 inhibitors such as sitagliptin sit in a neutral zone, neither promoting loss nor gain, and they bear a low hypoglycaemia risk. Ultimately, the “best” drug is the one that aligns with the patient’s comorbidities, financial reality, and personal preferences, and this alignment often requires iterative conversations and occasional medication swaps. It is also worth noting that lifestyle interventions-dietary tweaks, regular physical activity, and weight management-remain the cornerstone upon which any pharmacologic regimen builds its efficacy. Therefore, clinicians should present the comparative data as a menu, not a mandate, empowering patients to make informed choices. By doing so, we nurture adherence, mitigate adverse events, and enhance overall quality of life for those navigating the chronic journey of type 2 diabetes.
The so‑called “menu” approach is a soft‑sell veneer that masks the harsh truth: pushing a drug like Avandia onto a vulnerable patient under the guise of choice is nothing but reckless hubris. You gloss over the “modest weight gain” as if it were a trivial side‑effect, ignoring the real‑world increase in heart‑failure admissions that follows. The data you parade are cherry‑picked, and the emphasis on “iterative conversations” feels like a polite way to excuse a fundamentally unsafe prescription practice. In short, glorifying a molecule with a known high cardiovascular risk is a disservice and an ethical breach.
lol u think u r all smart but r u really? evryone knows drem meds are just big pharma tricks. why r we even talkin bout avandia when we could just eat salad? just sayin.
From a pharmacological perspective, the adverse event profile of rosiglitazone is dominated by its propensity for peripheral edema, which stems from PPARγ‑mediated fluid retention in adipose tissue. This mechanism not only predisposes patients to congestive heart failure but also complicates the management of comorbid hypertension. Moreover, the drug’s influence on bone turnover has been associated with an increased incidence of fractures in post‑menopausal women, necessitating vigilant bone health monitoring. When evaluating therapeutic alternatives, clinicians should weigh these risks against the modest glycaemic benefit and consider agents with proven cardiovascular safety, such as metformin or SGLT2 inhibitors, especially in patients with existing cardiac disease.
Ever think about how each pill is like a small promise we make to ourselves? You pick a drug, you hope it’ll be the key that unlocks better health, but the real key might be the daily habit of moving your body and watching what you put on your plate. The data in the table is useful, but don’t let it blind you to the simple truth: consistency beats flash.
What they don’t tell you in those pretty charts is that the “high‑risk” label on Avandia was a PR spin orchestrated by rival pharma giants desperate to protect their market share. The so‑called “FDA boxed warning” was whispered into existence after a covert lobbying push, and the real numbers on heart attacks are nowhere near the dramatic headlines. Don’t be fooled-dig deeper, question the source, and you’ll see the story is far more nuanced.
🙂 It’s easy to get swept up in the drama of competing narratives, but at the end of the day we’re all trying to keep people alive and thriving. Each medication has its place, and the best outcomes usually come from a collaborative approach where clinicians, patients, and families all have a voice. Let’s focus on shared goals rather than factional battles.
i mean, real talk, if u got metformin u already got the gold standard. avandia is just a backup for the stubborn ones who cant handle the cheap stuff. no need to hype it up.
I hear the concerns about heart risk and weight gain, and I also understand how frustrating it can be when simpler options aren’t enough. Finding the right balance is a personal journey, and it’s okay to feel unsure.
Hey folks, let’s keep the conversation lively! If anyone has personal stories about switching from a TZD to an SGLT2 inhibitor, share them – the real‑world experiences can really help us all make smarter choices.