Heart failure isn’t a single event-it’s a journey. It starts long before symptoms appear, and it doesn’t end with a diagnosis. Managing it well means understanding where you are, what treatments actually work, and how to live fully despite the condition. The latest guidelines from the American Heart Association and American College of Cardiology (2023) have rewritten the rules. This isn’t just about taking pills anymore. It’s about precision, timing, and personalization.
Stages of Heart Failure: Know Where You Stand
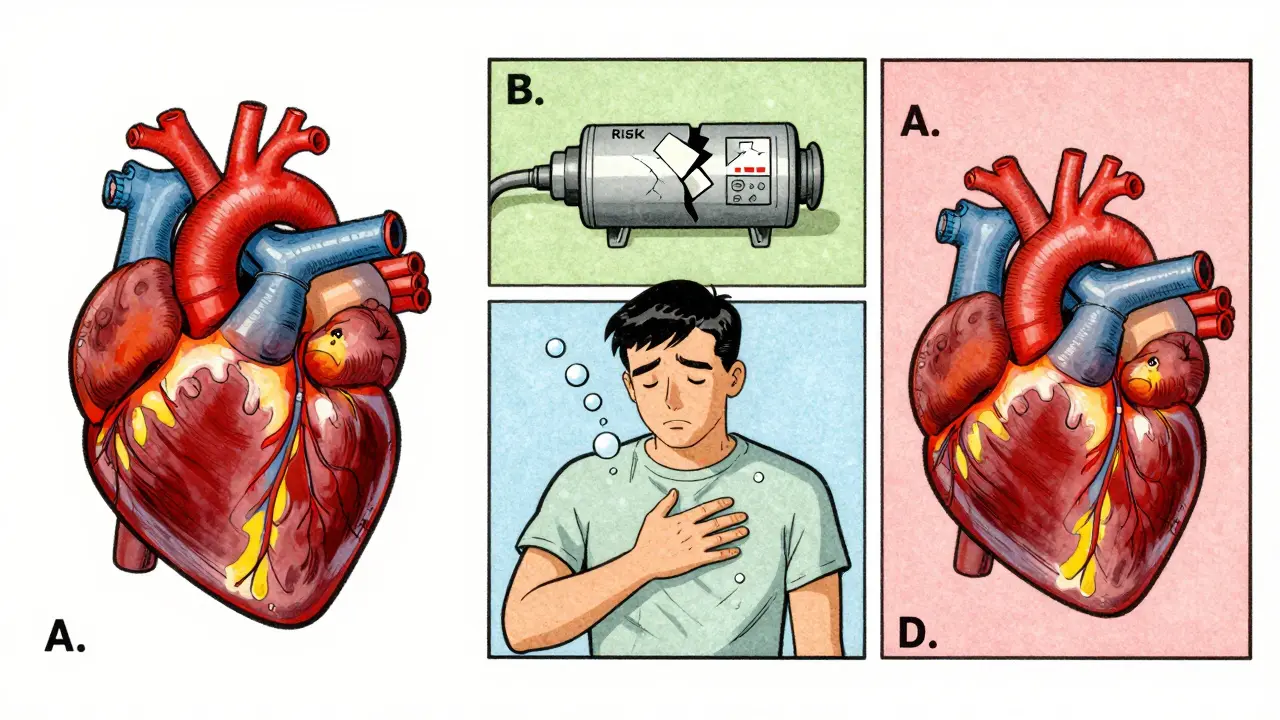
Heart failure is broken into four stages, not by how bad you feel, but by what’s happening inside your heart. Stage A means you’re at risk-maybe you have high blood pressure, diabetes, or a family history-but your heart still looks normal on scans. Stage B is when there’s structural damage: a weakened pump, thickened walls, or past heart attacks-but no shortness of breath or swelling yet. Stage C is where most people get diagnosed: the heart is damaged, and symptoms like fatigue or fluid buildup show up. Stage D is advanced: your body struggles even at rest, and you may need devices or transplants.What matters most is catching it early. A 2024 study found that 68% of people in Stage B never received treatment, even though starting an ACE inhibitor at this stage cuts the risk of progressing to full heart failure by nearly 50%. If you’ve had a heart attack or have a reduced ejection fraction, don’t wait for symptoms. Talk to your doctor about starting therapy now.
Heart Failure Types: It’s Not One Disease
Not all heart failure is the same. The key difference is how well your heart squeezes. That’s measured by ejection fraction (EF)-the percentage of blood pumped out with each beat.- HFrEF (reduced EF): EF ≤40%. The heart is weak and can’t pump hard enough. This used to be the only type with clear treatments.
- HFmrEF (mildly reduced EF): EF 41-49%. A gray zone, but now treated like HFrEF because therapies work here too.
- HFpEF (preserved EF): EF ≥50%. The heart squeezes fine but is stiff, like a worn-out balloon. For decades, doctors had almost nothing to offer.
Until 2021, HFpEF management meant diuretics and hoping for the best. Then came SGLT2 inhibitors-drugs originally made for diabetes. The EMPEROR-PRESERVED and DELIVER trials changed everything. Empagliflozin and dapagliflozin cut hospitalizations by 20% in HFpEF patients. That’s not a small win. It’s the first real breakthrough in decades.
The Quadruple Therapy Revolution for HFrEF
If you have HFrEF, the goal is simple: four drugs, all at target doses. This isn’t optional. It’s the new standard-and it saves lives.- ARNI (sacubitril/valsartan): Replaces ACE inhibitors or ARBs. It reduces death by 20% compared to older drugs. Target dose: 97/103 mg twice daily.
- Beta-blockers: Only specific ones work: carvedilol, metoprolol succinate, or bisoprolol. They slow the heart, reduce strain, and cut mortality. Target: 25 mg twice daily for carvedilol.
- MRA (mineralocorticoid receptor antagonist): Spironolactone or eplerenone. They fight fluid retention and scarring. Target: 25 mg daily.
- SGLT2 inhibitor: Dapagliflozin or empagliflozin. Even if you don’t have diabetes, these reduce hospitalizations and death. Target: 10 mg daily.
Each drug has a number needed to treat (NNT). For ARNI, you need to treat 12 people for 3 years to prevent one death. For beta-blockers, it’s 17. That means, on average, every 17th person you treat will live longer because of them. These aren’t guesses-they’re proven.
Yet, only 39% of eligible patients get all four within a year. Why? Many doctors are slow to start. Others fear low blood pressure or kidney changes. But here’s the truth: severe low blood pressure (under 90 mmHg) affects just 1.8% of heart failure patients. Most doctors overestimate this risk by five times. The bigger barrier? Complexity. Managing eight pills a day is exhausting.
Monitoring: When Tech Becomes Your Ally
The CardioMEMS HF System is a tiny sensor implanted in the lung artery. It wirelessly sends pressure readings to your doctor. If pressure rises, your meds can be adjusted before you feel swollen or winded.The MONITOR-HF trial (2025) confirmed what earlier studies hinted at: patients using CardioMEMS had 28% fewer hospitalizations and better quality of life. One Reddit user wrote: “I went from three hospital trips a year to zero in 18 months.” That’s not luck. That’s data-driven care.
But it’s not for everyone. It’s for Stage C and D patients who keep bouncing back to the hospital. If you’re not getting better with meds alone, ask if this is an option. Medicare covers it, and the cost-around $21,000 for the device-is offset by avoiding ER visits.
Living Well: Beyond the Pills
Treatment isn’t just about drugs. It’s about daily habits.- Salt under 2,000 mg/day: Most people eat 3,500 mg. Cutting it reduces fluid buildup and lowers blood pressure.
- Weight checks daily: Gain 2 lbs in a day? That’s fluid. Call your doctor.
- Exercise-even light: A 10-minute walk every day cuts hospital risk by 22%. You don’t need to run.
- Get vaccinated: Flu and pneumonia hit heart failure patients harder. Get them yearly.
- Sleep apnea screening: Half of heart failure patients have it. Treating it improves EF by 10%.
One patient in Bristol told me: “I started walking after dinner. No gym. Just 15 minutes. I sleep better. I don’t wake up gasping anymore.” Simple. Effective. Undervalued.

Barriers and Inequalities
Not everyone gets the same care. Black patients are 37% less likely to receive guideline-recommended therapy. They also have 28% higher death rates-even after adjusting for income, insurance, or location. Why? Systemic gaps: fewer specialists in their neighborhoods, less follow-up, implicit bias in prescribing.The ACC’s “HF in a Box” toolkit helps. It gives clinics checklists, patient education sheets in 17 languages, and decision trees. Clinics using it saw a 27% jump in quadruple therapy use. This isn’t magic. It’s structure.
Medication adherence is another hurdle. The average HFrEF patient takes 7.3 pills a day. One caregiver on HeartFailureMatters.org said: “My husband has eight heart meds. I set alarms. I use a pill organizer. Still, we miss doses.” Simplifying regimens-like switching to combination pills-can help.
What’s Next?
Research is moving fast. Scientists are studying CHIP-clonal hematopoiesis, a blood condition in 15-20% of older adults-that doubles heart failure risk. A trial called INTERCEPT-HF is testing whether blocking inflammation with canakinumab helps. Another trial, TARGET-HF, is testing personalized blood pressure targets. One size doesn’t fit all.Meanwhile, SGLT2 inhibitors are the fastest-growing heart failure drug class. Farxiga (dapagliflozin) now leads the HFpEF market. The global heart failure drug market will hit $25 billion by 2029. But money doesn’t cure. Access does.
Heart failure isn’t a death sentence. It’s a condition you can live with-well-if you have the right tools. The science is here. The drugs work. The monitoring exists. What’s missing is the push to use them.
Can heart failure be reversed?
In some cases, yes-especially if caught early. Stage A and B patients who start ACE inhibitors or ARNIs can prevent progression. Even in Stage C, some patients see their ejection fraction improve by 10-15% with quadruple therapy. It’s not a cure, but it can turn a weakening heart into a stable one.
Do I need to stop all my other medications?
No. But some may need adjusting. For example, NSAIDs like ibuprofen can worsen fluid retention and kidney function. Always review all meds-prescription, OTC, and supplements-with your cardiologist. Some diabetes drugs, like metformin, are safe. Others, like certain calcium channel blockers, may need replacement.
Why do I need to take four drugs if I feel fine?
Heart failure often feels quiet until it’s advanced. These drugs don’t just treat symptoms-they slow the disease. SGLT2 inhibitors and ARNIs don’t make you feel better right away. But over 2-3 years, they cut your risk of dying or being hospitalized by nearly half. Feeling fine now means the treatment is working.
Is heart failure hereditary?
Not directly, but risk factors can be. If close relatives had heart failure before age 60, your risk increases. Genetic conditions like familial cardiomyopathy exist but are rare. More commonly, inherited traits like high blood pressure, diabetes, or high cholesterol run in families. That’s why screening matters-even if you feel fine.
Can I drink alcohol with heart failure?
Moderation is key. One drink a day (12 oz beer, 5 oz wine) is generally safe for most. But alcohol weakens the heart muscle over time. If your EF is below 30%, or you have arrhythmias, avoid it. Many patients report feeling better after quitting-even if they didn’t think alcohol was the issue.
What if I can’t afford these medications?
SGLT2 inhibitors and ARNIs can be expensive, but assistance programs exist. AstraZeneca and Boehringer Ingelheim offer patient support with copay cards and free drug programs for eligible low-income patients. Ask your pharmacist or cardiologist. Generic alternatives aren’t available yet, but switching to lower-cost beta-blockers or MRAs can help reduce overall cost.








So let me get this straight-we’ve got drugs that can cut hospitalizations by 20% for HFpEF, but only 39% of people get all four meds? 😒
Meanwhile, my uncle’s doctor still prescribes him a diuretic and says "just cut the salt." No wonder people keep bouncing back. This isn’t medical care. It’s a game of telephone where the message gets lost somewhere between the guideline and the prescription pad.
quadruple therapy?? like, 8 pills a day?? bro i take 3 pills for my anxiety and i forget half the time. imagine having to remember 4 different meds that all sound like sci-fi drugs. i’m not a robot. also who the hell has a pill organizer that can handle 8 different colors??
As someone who’s been living with HFrEF for 5 years, I can say this: the ARNI + SGLT2 combo changed my life. I went from barely making it up the stairs to walking 3 miles daily. No gym, no fancy gear-just consistency.
But here’s the thing nobody talks about: the side effects. My potassium spiked on spironolactone, and I had to get IV fluids once. My doc didn’t warn me. I almost quit. If you’re starting this, ask for a lab schedule. Monitor. Don’t just trust the script.
Also-yes, the cost is brutal. I got dapagliflozin for $5/month through a patient assistance program. Ask your pharmacist. Seriously. They’re not just there to hand you the bottle.
Love this breakdown. I’ve been telling everyone I know with hypertension to get an echo if they’ve had a heart attack-even if they feel fine. Stage B is where you can still turn things around.
Also, the CardioMEMS thing? My mom got one last year. She’s had zero hospital visits since. Before? Twice a year. It’s not magic, but it’s the closest thing we’ve got to a crystal ball for heart failure. Worth every penny if you’re a frequent flyer to the ER.
Just wanted to say… I’m a caregiver for my wife, and I cried reading this. We’ve been struggling for 2 years. Missed doses. Confusing instructions. Doctor visits where we left with more questions than answers.
But now? We’ve got the four-drug plan. We use a pillbox with alarms. We weigh her every morning. We walk after dinner-just 15 minutes. She’s sleeping through the night for the first time in years.
I know it sounds simple. But sometimes, simple is the hardest thing to stick to. Thank you for making this real. Not just stats. Real people.
Also-yes, salt is HARD. We used to eat canned soup like it was water. Now? We make broth from scratch. It’s a lifestyle change. But worth it.
OMG YES 🙌 I’ve been telling my doc for months that we need to switch from lisinopril to ARNI. He said "it’s too expensive." I showed him the patient assistance program link. He just shrugged. Now I’m switching docs. This isn’t about money-it’s about survival. We have the tools. Why aren’t we using them?? 💔
Wait… so SGLT2 inhibitors were made for DIABETES?? And now they’re saving hearts?? Hmm… I smell a pharmaceutical conspiracy. Why didn’t they just make a "heart drug" from the start? Why use a diabetes drug and then market it as a miracle? Did Big Pharma know this would work all along and just sat on it? I think they did. I think they’re milking this. Also-why is this only covered by Medicare? What about people under 65?? 🤔
My dad’s EF went from 28% to 42% in 14 months. All four drugs. No magic. Just daily discipline.
He still watches TV. Still eats pizza. Still naps. But he walks. Every day. 10 minutes. That’s it.
From India, I just want to say: we don’t have access to most of these drugs here. ARNI? Costly. CardioMEMS? Not available. Even basic beta-blockers are hard to get in rural clinics.
But we do have salt. We do have walking. We do have family. My cousin with HFpEF walks 30 mins after sunset. No meds. Just air, rhythm, and hope.
Science is great. But humanity? That’s what keeps people alive.
Ugh. Another "just walk more" article. Like that’s gonna fix a broken heart. Have you SEEN how many people are on these meds? They’re exhausted. Their kidneys are failing. Their blood pressure is in the toilet. This isn’t empowerment-it’s guilt-tripping with a medical license.
While I appreciate the comprehensive nature of this overview, I must respectfully note that the emotional and socioeconomic dimensions of heart failure management remain underemphasized. The disparity in care delivery is not merely a clinical oversight-it is a systemic failure rooted in historical inequities. A policy-oriented response, not merely a pharmacological one, is required to ensure equitable access.
So if I’m Stage B and my EF is 55%, do I even need to start anything? My doc says "keep an eye on it." But this article says 68% of Stage B folks get nothing. Should I push harder? Or am I overreacting?
They’re lying to you. They’re all lying. SGLT2 inhibitors? They were tested on people who already had diabetes. They didn’t test on the poor. On the Black. On the uninsured. They’re pushing this because it’s profitable. And now they want you to take FOUR drugs? That’s not medicine. That’s a pyramid scheme with a stethoscope.
My cousin died because they gave him the wrong combo. They didn’t check his potassium. They didn’t listen. Now I don’t trust ANY doctor. Don’t trust them. Ask for the raw data. Demand the trials. Don’t let them treat you like a number.
Been living with HFpEF for 7 years. I was told "there’s nothing we can do" until 2022. Then my cardiologist said "try dapagliflozin." I was skeptical. I didn’t have diabetes. I didn’t think it’d do anything.
Three months in, I could carry groceries without stopping. Six months, I started gardening again. Two years later, my EF went from 51% to 58%. No surgery. No device. Just a pill that was originally for diabetics.
So yeah. Science is weird. But sometimes, it works. And when it does? You don’t question it. You just live.
Also-I still drink one beer a night. My doc said fine. I’m not giving up everything. I’m giving up the fear.