Ever wonder why doctors keep talking about "bad" cholesterol when you’re already worried about your kidneys? The connection isn’t a coincidence; research over the past decade shows that low-density lipoprotein (LDL) can speed up kidney damage and make chronic kidney disease (CKD) harder to control. This article breaks down the science, shares real‑world data, and gives practical steps you can take right now.
TL;DR
- High LDL levels accelerate CKD progression by promoting atherosclerosis in renal vessels.
- Inflammation and oxidative stress link cholesterol spikes to glomerular injury.
- Statins, plant‑based diets, and regular exercise lower LDL and modestly slow kidney function loss.
- Track eGFR and proteinuria every 6‑12 months if you have high LDL or CKD risk factors.
- Talk to your clinician about personalized lipid targets; typical LDL goal for CKD patients is < 70mg/dL.
What Is Low‑Density Lipoprotein?
Low‑Density Lipoprotein is a lipoprotein particle that carries cholesterol from the liver to peripheral tissues. When levels rise above the optimal range (generally <100mg/dL for healthy adults), LDL tends to deposit cholesterol on arterial walls, forming plaque. This process, called atherosclerosis, narrows blood vessels and reduces blood flow. While most people associate LDL with heart attacks, the same clogging can happen in the tiny arteries that feed the kidneys.
Understanding Chronic Kidney Disease
Chronic Kidney Disease is a gradual loss of kidney function over months or years, usually measured by the glomerular filtration rate (GFR). A GFR below 60mL/min/1.73m² for three months or more signals CKD. The disease is staged from 1 (mild) to 5 (kidney failure). Common triggers include diabetes, hypertension, and-importantly-dyslipidemia.
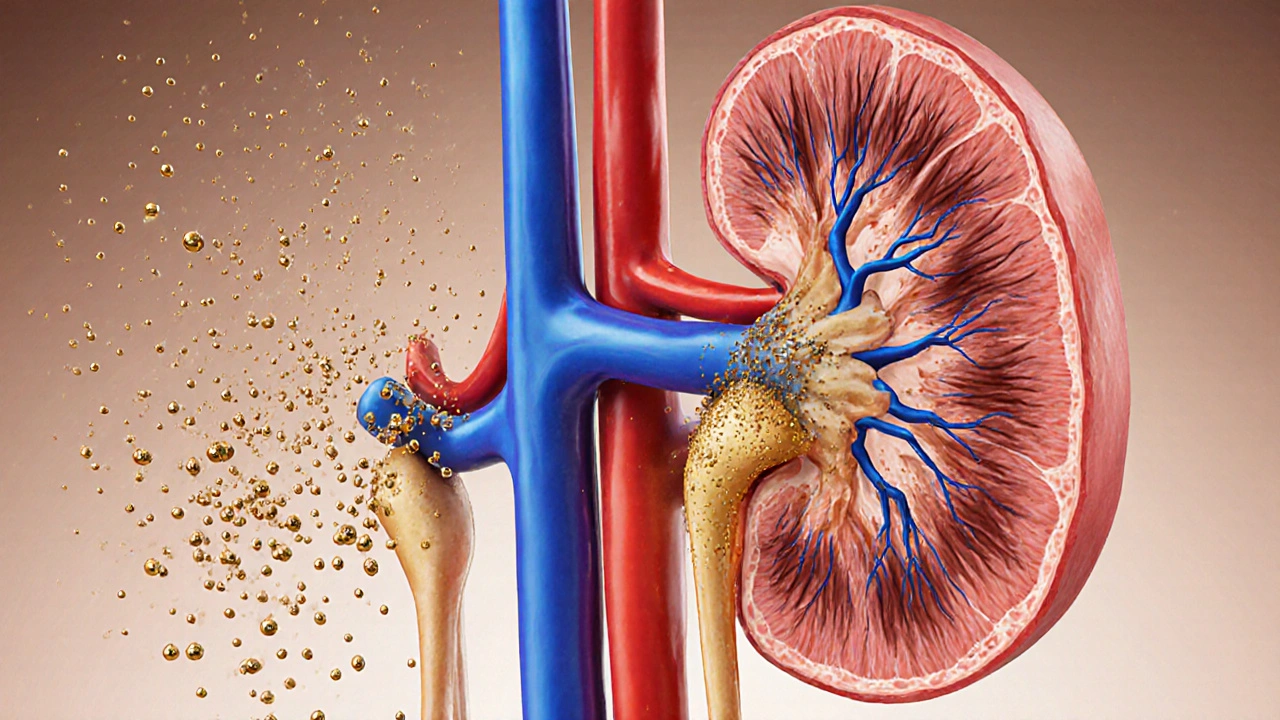
How LDL Hurts the Kidneys
Three biological pathways link high LDL to kidney damage:
- Atherosclerotic narrowing of renal arteries: Plaque buildup reduces perfusion pressure, forcing the glomeruli to work harder and eventually scar.
- Inflammation and oxidative stress: Oxidized LDL particles trigger immune cells to release cytokines (e.g., IL‑6, TNF‑α). Those messengers promote fibrosis in kidney tissue.
- Direct toxicity to podocytes: Podocytes are the tiny cells that keep protein from leaking into urine. Laboratory studies show that oxidized LDL damages podocyte structure, leading to proteinuria.
When you combine these mechanisms with hypertension, the kidneys face a double whammy: high pressure and poor blood supply. That’s why patients with high LDL often see faster declines in eGFR.

Clinical Evidence at a Glance
Large cohort studies from the United States, Europe, and Asia have quantified the risk:
| LDL (mg/dL) | Annual eGFR Decline | Relative Risk of ESRD |
|---|---|---|
| <70 | 1.2mL/min | 1.0 (reference) |
| 70‑100 | 2.3mL/min | 1.4 |
| 100‑130 | 3.6mL/min | 2.0 |
| >130 | 5.1mL/min | 3.1 |
These numbers come from the Chronic Kidney Disease Prognosis Consortium (2022) and confirm a dose‑response relationship: the higher the LDL, the steeper the drop in kidney function.
Managing LDL to Protect Your Kidneys
Lowering LDL isn’t just about heart health; it can literally buy you years of kidney function.
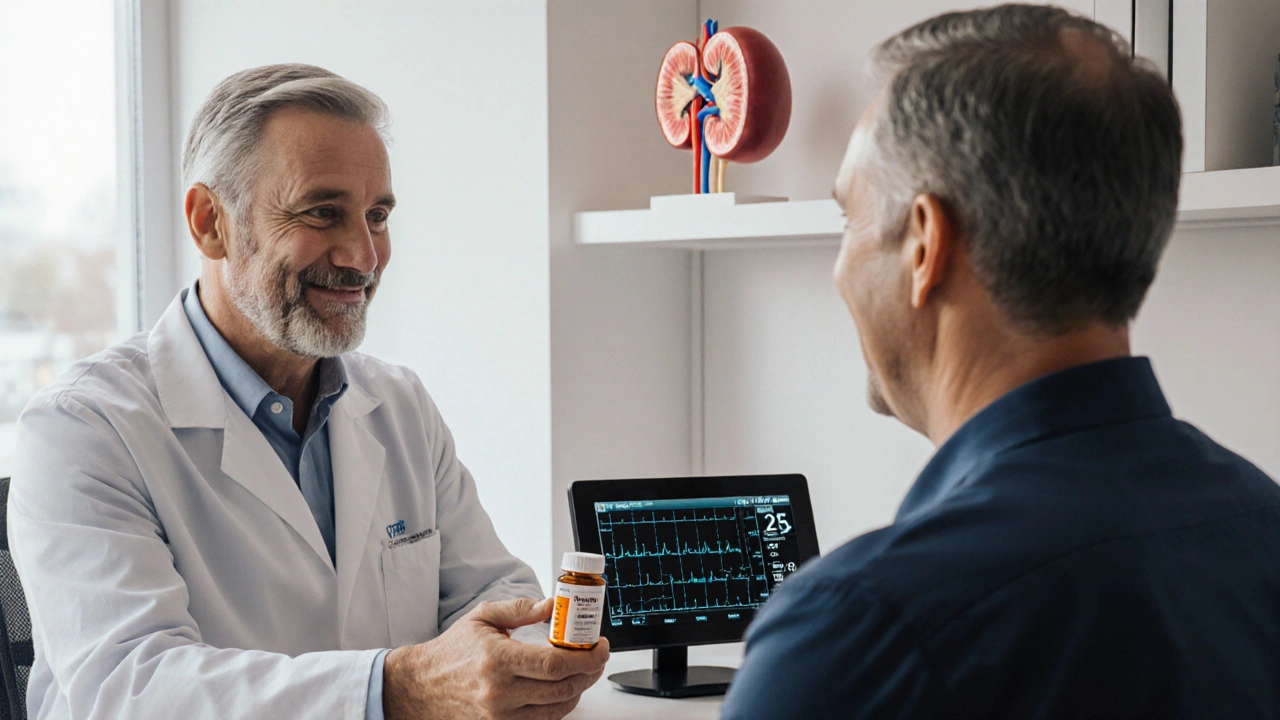
Statins: The First‑Line Weapon
Statins inhibit HMG‑CoA reductase, the enzyme that drives cholesterol synthesis in the liver. In CKD patients, moderate‑intensity statins reduce LDL by 30‑50% and have been shown to slow eGFR decline by ~0.5mL/min per year. Common choices include atorvastatin, rosuvastatin, and pravastatin. For stage 3 CKD, guidelines recommend a target LDL below 70mg/dL.
Lifestyle Tweaks That Matter
- Plant‑based diet: Replacing red meat with legumes, nuts, and whole grains can cut LDL by up to 15%.
- Soluble fiber: Oats, barley, and psyllium bind cholesterol in the gut, reducing absorption.
- Regular aerobic activity: 150 minutes per week of moderate exercise improves HDL and lowers LDL.
- Smoking cessation: Smoking oxidizes LDL, making it more harmful; quitting reduces oxidative stress within weeks.
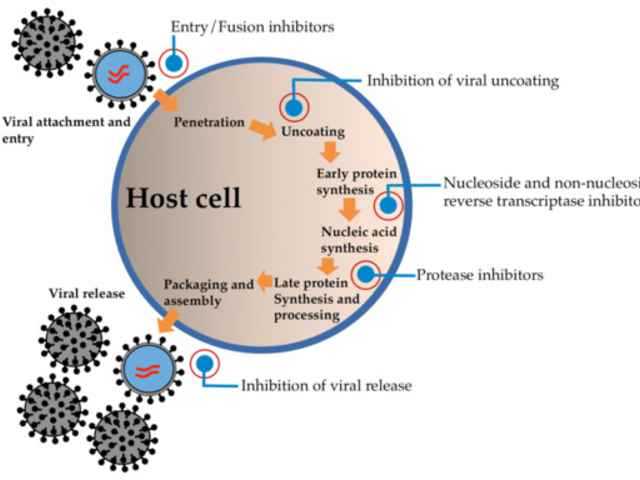
When Statins Aren’t Enough
Some patients reach a plateau despite max‑dose statins. Adding a PCSK9 inhibitor (e.g., evolocumab) can drive LDL into the single‑digit range, but cost and insurance coverage are real barriers. For CKD stages 4‑5, the safety profile of PCSK9 inhibitors is still being evaluated, so discuss risks with your nephrologist.
Monitoring Kidney Health While Treating Lipids
Two key markers tell you whether the LDL‑killing plan is helping the kidneys:
- Estimated GFR (eGFR) measures how well the kidneys filter blood. Track it every 6-12 months; a slowing decline signals success.
- Proteinuria (albumin‑to‑creatinine ratio) reflects podocyte damage. Lower values after LDL reduction suggest less inflammation.
Ask your clinician to set personalized targets: e.g., keep eGFR loss under 2mL/min per year and maintain proteinuria below 30mg/g.
Key Takeaways
- High LDL accelerates CKD by clogging renal vessels, sparking inflammation, and hurting podocytes.
- Statins are the cornerstone; aim for LDL<70mg/dL in most CKD patients.
- Lifestyle changes amplify medication benefits and support overall kidney health.
- Regular eGFR and proteinuria checks let you see progress early.
Frequently Asked Questions
Can low LDL levels harm the kidneys?
Very low LDL (below 30mg/dL) is rare and usually only seen with aggressive PCSK9 therapy. Current evidence shows no direct kidney injury from low LDL; the main concern is muscle‑related side effects from high‑dose statins, which are manageable.
Do cholesterol‑lowering foods work for CKD patients?
Yes. Studies in the Kidney Disease Outcomes Quality Initiative (2021) found that a Mediterranean‑style diet lowered LDL by ~12% and slowed eGFR decline by 0.3mL/min per year compared with a standard low‑sodium diet.
Is it safe to combine statins with blood‑pressure meds for kidney disease?
Generally, yes. The most common interaction is between statins and certain calcium‑channel blockers, which can raise statin levels. Your doctor can adjust dosages or pick a statin with a lower interaction risk, such as pravastatin.
How often should I get my lipid panel if I have CKD?
Guidelines suggest every 3‑6 months while you’re adjusting therapy, then annually once LDL stays within target and kidney function is stable.
Can I use over‑the‑counter supplements to lower LDL?
Plant sterols, soluble fiber powders, and omega‑3 fish oil can modestly reduce LDL (5‑10%). They’re safe for most CKD patients, but always check with your nephrologist, especially if you’re on blood thinners.







It is heartening to see the burgeoning body of evidence linking LDL to renal decline; patients should therefore consider periodc lipid monitoring as part of their CKD managment plan.
We stand at the crossroads where cholesterol becomes a prophecy of renal fate the arteries of the kidney whisper of impending doom yet the doctor’s clipboard remains mute
From a pathophysiological standpoint, the atherogenic lipid profile precipitates endothelial dysfunction via oxidized LDL-mediated ROS cascades, thereby exacerbating glomerulosclerosis-clearly a textbook illustration of why we should have anticipated this all along, right?
The relationship between LDL and CKD is not a mere coincidence but a mechanistic interaction that has been elucidated over the past decade.
Elevated LDL particles infiltrate the renal vasculature, promoting intimal thickening and atherosclerotic plaque formation within the arcuate arteries.
This vascular remodeling reduces perfusion pressure, leading to ischemic injury of the nephron.
Simultaneously, oxidized LDL triggers inflammatory signaling pathways, notably NF-κB activation, which amplifies cytokine release.
The resulting pro‑inflammatory milieu accelerates podocyte apoptosis and mesangial expansion.
Clinical data from large cohort studies demonstrate that patients with LDL > 130 mg/dL experience a statistically significant faster decline in eGFR compared to those with optimal lipid levels.
Moreover, interventional trials with high‑intensity statins have shown modest but reproducible reductions in the rate of kidney function loss.
It is important to note that statins also possess pleiotropic effects, such as improving endothelial nitric oxide bioavailability, which further protects renal microcirculation.
Dietary modifications, especially a shift toward plant‑based fats, have been shown to lower LDL concentrations by up to 20 % within three months.
Regular aerobic exercise augments HDL synthesis and enhances LDL receptor activity, thereby facilitating the clearance of circulating LDL particles.
For patients with pre‑existing CKD, individualized lipid targets-often aiming for LDL < 70 mg/dL-are recommended to mitigate progression.
Monitoring should include serial eGFR assessments and quantitative proteinuria measurement every six to twelve months.
Patient education is crucial; many individuals are unaware that cholesterol management directly impacts renal outcomes.
Clinicians should engage in shared decision‑making, discussing the risk‑benefit profile of statin therapy in the context of potential side effects.
Ultimately, a multidisciplinary approach that integrates nephrology, cardiology, and nutrition expertise yields the best prognostic trajectory.
By addressing LDL proactively, we not only curb cardiovascular morbidity but also preserve kidney function for years to come.
It’s astonishing how often people dismiss cholesterol as irrelevant to kidney health while simultaneously ignoring the most basic lipid guidelines; perhaps a refresher course on primary prevention is overdue.
Thanks for laying it all out so clearly 😄.
I’ve been struggling to understand how my diet impacts my labs, and this really bridges that gap.
It’s encouraging to see that even small lifestyle tweaks, like adding a daily walk or swapping butter for olive oil, can make a measurable difference in LDL and, by extension, kidney health.
The science can feel overwhelming, but breaking it down into actionable steps makes it feel doable.
I’ll definitely be setting reminders to check my eGFR and proteinuria as you suggested.
Keep the evidence‑based tips coming! 🙏
Balancing lipid control with kidney preservation is a nuanced challenge, but the evidence suggests that a moderate statin dose paired with lifestyle changes offers a pragmatic path forward for most patients.
Oh wow, so you’re telling me we can just “balance” this giant health crisis with a pill and a salad? That’s the most dramatic oversimplification ever!
Statins are just a band‑aid for the real problem…
Let’s be real, tackling LDL is a marathon, not a sprint, and every step you take-whether it’s a 20‑minute jog or swapping out fries for a quinoa bowl-adds up to a healthier kidney future. You’ve got this!
Totally agree, just remember to stay consistent and maybe set a weekly reminder so the habit sticks. Grammar check: “you’ve got this” is perfect motivation.
While the literature unequivocally demonstrates a causal link between elevated LDL and renal deterioration, it is, of course, far more expedient to ignore the data and continue prescribing high‑fat diets to the unsuspecting populace.
It is both heartbreaking and infuriating to witness patients suffer preventable kidney damage simply because the significance of LDL management is downplayed.
Don’t be fooled-the “studies” linking cholesterol to kidney disease are part of a larger agenda to push pharmaceutical profit, all while big agribusiness hides the truth about natural lipid regulation.
For anyone starting out, a practical first step is to schedule a lipid panel, then work with your doctor to set a realistic LDL target; from there, incorporating a Mediterranean‑style diet and regular movement can steadily bring those numbers down.