Getting the right dose of medicine for a child isn’t just about following a prescription-it’s about survival. A child’s body isn’t a small adult. Their organs, metabolism, and fluid balance work differently, and even a tiny mistake in dosing can lead to serious harm. That’s why weight-based dosing isn’t just best practice-it’s the only safe way to give most medications to kids. But even the best formula won’t save a child if the calculation is wrong or skipped. That’s where the double-check comes in.
Why Weight Matters More Than Age
For decades, doctors guessed pediatric doses based on age. "Give half a teaspoon for a 4-year-old." It was easy. But it was also dangerous. A 4-year-old who’s underweight might get too much. One who’s overweight might get too little. Research shows age-based dosing leads to errors in nearly 3 out of 10 cases, especially in kids at the extremes of growth. Today, every major pediatric hospital and health system uses weight-based dosing. The formula is simple: milligrams per kilogram (mg/kg). You take the child’s weight in kilograms, multiply it by the prescribed dose per kg, and you get the total daily dose. Then you divide that by how many times a day the medicine is given. For example: A 10 kg child prescribed 40 mg/kg/day of amoxicillin. That’s 10 × 40 = 400 mg total per day. If it’s given twice a day, each dose is 200 mg. Easy. But only if the weight is correct.The Math Behind the Safety
Getting the weight right starts with the scale. In the U.S., many scales still show pounds. But every pediatric dosing protocol requires kilograms. That’s where mistakes creep in. The Institute for Safe Medication Practices found that 32% of all pediatric dosing errors come from mixing up pounds and kilograms. The conversion is exact: 1 kg = 2.2 lb. No rounding. Not even a little. If a child weighs 22.4 pounds, you divide by 2.2 to get 10.1818... kg. You don’t round to 10.2 yet. You keep all the decimals until the final calculation. Round too early, and you start piling up tiny errors that add up to dangerous doses. Some drugs need even more precision. Chemotherapy, for example, often uses body surface area (BSA) instead of weight. The Mosteller formula-√(weight in kg × height in cm ÷ 3600)-gives better results for these drugs. But it takes longer. One study showed BSA calculations added 47 seconds per dose. In a busy ER, that’s time you don’t always have.When Weight Isn’t Enough
Weight-based dosing works for most kids. But not all. For babies under 6 months, especially preemies, their kidneys and liver aren’t fully developed. A 3 kg newborn might need a dose that’s 40-60% lower than what the weight formula suggests for an older infant. Giving the full dose could cause toxic buildup. For obese children, the problem flips. If a child has a BMI over the 95th percentile, their body fat changes how drugs are absorbed. Water-soluble drugs (like antibiotics) spread through body water, so using total weight might over-dose them. Fat-soluble drugs (like some seizure meds) stick to fat, so under-dosing becomes the risk. That’s why many hospitals use adjusted body weight (ABW): Ideal body weight + 0.4 × (actual weight − ideal weight). This method is used in 78% of children’s hospitals for certain drugs. It’s not perfect-but it’s safer than using raw weight.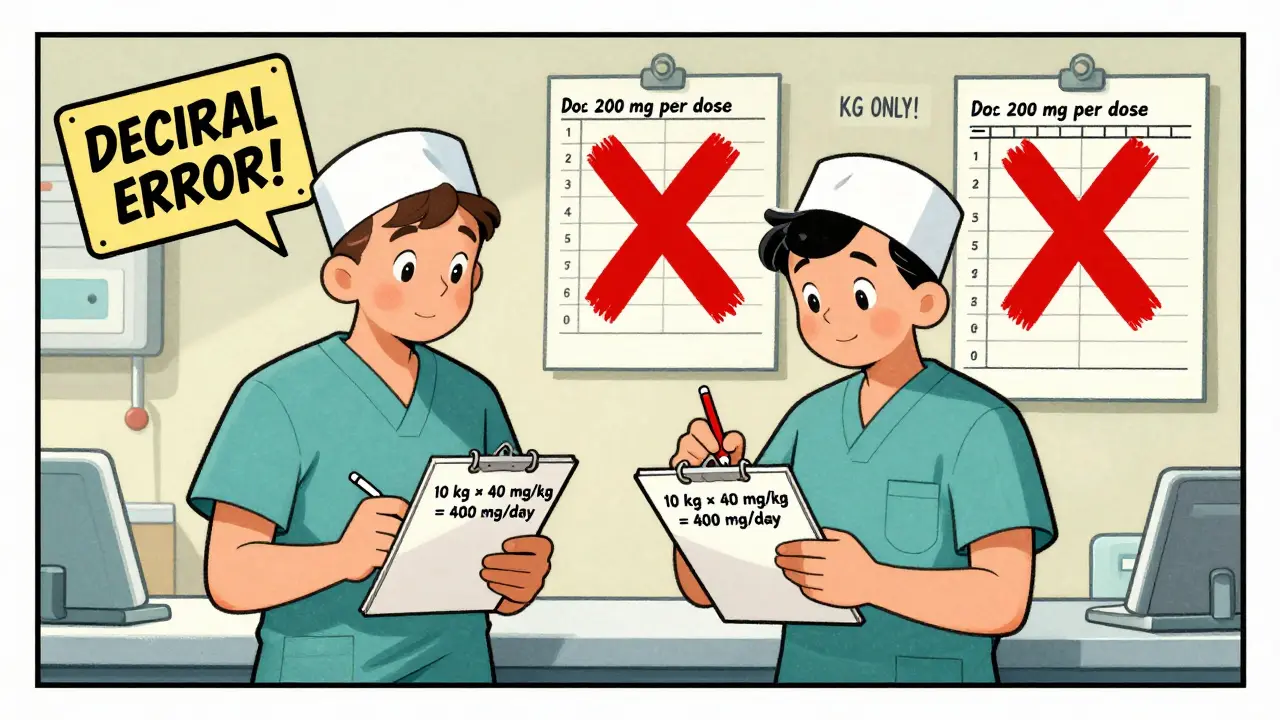
The Double-Check That Saves Lives
Here’s the hard truth: even the best calculator can’t prevent human error. A tired nurse. A rushed resident. A misread decimal. That’s why every major safety organization-The Joint Commission, the American Academy of Pediatrics, the Institute for Safe Medication Practices-requires a double-check for high-alert medications. A double-check isn’t just asking a coworker, "Does this look right?" It’s two independent people doing the full calculation from scratch. One calculates. The other recalculates. They compare. They verify the weight. They check the drug’s maximum safe dose. They look at the child’s history-any kidney or liver issues? Any recent changes? One nurse on AllNurses shared how her team caught a 10-fold error: a resident ordered 200 mg for a 10 kg child. The safe max for amoxicillin is 40 mg/kg/day, so 400 mg total. The dose was 200 mg per dose-twice the safe amount. The double-check caught it. The child was fine. The resident learned. That’s the power of the system.Where Things Go Wrong
Despite protocols, errors still happen. The ISMP’s 2022 report tracked 1,247 pediatric dosing errors. The top three causes?- Incorrect unit conversion (38%) - pounds instead of kilograms, or vice versa.
- Decimal point errors (27%) - writing 20.0 mg instead of 2.0 mg, or missing a zero entirely.
- Failing to adjust for organ function (19%) - giving the same dose to a child with kidney impairment as one who’s healthy.

What’s Changing Now
The future of pediatric dosing isn’t just about better math-it’s about smarter systems. In June 2023, Epic Systems rolled out new pediatric dosing modules in their EHR. These tools auto-calculate weight-based doses, flag unsafe ranges, and even cross-check with the child’s lab results. They’re now in 78% of children’s hospitals. The NIH’s Pediatric Trials Network has enrolled over 15,000 kids to build better dosing data for common drugs. And in April 2023, the WHO updated its list of essential medicines for children, adding specific weight-band dosing for 127 drugs. That means even in low-resource settings, there’s now a clear guide. Soon, genetics may play a role. Testing for CYP2D6 and CYP2C19 genes can tell if a child metabolizes opioids quickly or slowly. That could cut adverse events by nearly 40%. But that’s still years away. Right now, weight and double-checks are what keep kids safe.What You Need to Remember
If you’re a parent, know your child’s weight in kilograms. Ask the nurse or doctor to show you the calculation. Don’t assume it’s right. If you see a dose that seems too high or too low, speak up. If you’re a provider: never skip the double-check. Never round until the final step. Never rely on age. Always check renal and hepatic function. Use the system. The tools are there. Weight-based dosing isn’t magic. It’s math. And double-checks aren’t bureaucracy-they’re a lifeline. Every year, 1 in 5 children in hospitals gets a medication error. Most of them are preventable. The fix isn’t expensive. It’s simple. And it’s already proven to work.Why can’t we just use age to dose children’s medications?
Age-based dosing is outdated and unsafe. Children of the same age can vary wildly in weight, body composition, and organ function. A 4-year-old who’s underweight may get too much medicine, while one who’s overweight may get too little. Studies show age-based dosing leads to errors in 29% of cases. Weight-based dosing cuts that risk by more than half.
How do I convert pounds to kilograms correctly for pediatric dosing?
Use the exact conversion: 1 kg = 2.2 lb. Divide the weight in pounds by 2.2. Keep all decimal places until your final dose calculation. Never round the weight early. For example, a child weighing 22.4 lb is 10.1818 kg. Only round that number to 10.18 kg after you’ve multiplied it by the prescribed mg/kg dose. Rounding too soon causes cumulative errors that can be dangerous.
What’s a double-check, and why is it required?
A double-check is when two independent healthcare providers calculate the dose separately and compare results. It’s not just asking someone if it looks right-it’s two full calculations, with verification of weight, drug, and patient history. For high-alert drugs like chemotherapy, insulin, or opioids, this step is mandatory. Studies show it reduces serious errors by 68%.
Are there cases where weight-based dosing isn’t enough?
Yes. For newborns and infants under 6 months, organ maturity matters more than weight. Their kidneys and liver can’t clear drugs like adults, so doses often need to be reduced by 40-60%. For obese children, using total body weight can lead to overdosing with water-soluble drugs. In those cases, adjusted body weight (ABW) or body surface area (BSA) may be used instead.
What are the most common dosing errors in pediatrics?
The top three are: (1) mixing up pounds and kilograms (38% of errors), (2) decimal point mistakes like writing 20.0 mg instead of 2.0 mg (27%), and (3) not adjusting for kidney or liver problems (19%). These errors are preventable with proper training, clear protocols, and double-checks.








The entire premise of weight-based dosing is a statistical illusion masked as science. You're assuming all children of the same weight have identical pharmacokinetics, which is absurd. Metabolism varies by genetics, microbiome, even sleep patterns. The 40 mg/kg rule? A crude average that ignores heterogeneity. We're treating kids like lab rats with standardized inputs. And don't get me started on BSA-it's just a mathematical fiction derived from 1950s cadaver data. The real solution isn't better math, it's pharmacogenomic individualization. But that requires funding, and funding requires political will, which we don't have. So we keep bandaging systemic failures with decimal points and double-checks. Pathetic.
There's a deeper epistemological issue here. We treat dosing as if it's a purely quantitative problem-weight × mg/kg = safety. But medicine isn't math. It's a narrative of vulnerability. The child is not a variable in an equation. They're a being whose body is still becoming. The double-check isn't just a procedural safeguard-it's a ritual of humility. It forces us to pause, to acknowledge our fallibility. The real danger isn't the decimal error. It's the arrogance that believes precision eliminates uncertainty. We calculate to avoid guilt, not to achieve perfection. And that's why systems fail even when the math is flawless.
Parents need to know their child's weight in kg. Always ask to see the calculation. If a dose seems off, speak up. No hesitation. Nurses and doctors are human. Fatigue happens. Double-checks exist for a reason. Don't assume someone else caught it. Your voice can prevent a tragedy. I've seen it happen. A mother asked about a dose that was 10x higher than it should've been. They caught it. The child is fine. You are your child's best advocate. Trust your gut. You don't need to be a doctor. Just be present. Be loud. Be unapologetic. Safety isn't optional. It's non-negotiable.
I work in a pediatric ER and I’ve seen both sides. The system works when people follow it. The problem isn’t the protocol. It’s the burnout. Nurses rushing between rooms. Residents on 24-hour shifts. Scales not calibrated. Units mixed up. We need better staffing, not more rules. The red sticker on the scale? Brilliant. Simple. Effective. But if you’re exhausted, you’ll miss it. We need to fix the environment, not just the math. And yes, double-checks save lives. But they shouldn’t be a Band-Aid for a broken system.
Let’s be real-this isn’t about math. It’s about culture. If your hospital treats dosing like a checklist item, you’re already losing. The best teams I’ve worked with don’t just double-check-they talk. They ask, "Why this dose?" They pause. They look at the kid. They remember this isn’t a number on a screen. It’s a child who just got off the bus from school, scared, holding their mom’s hand. That’s when the math becomes sacred. I’ve seen residents cry after a near-miss. That’s the moment you realize: we’re not just prescribing drugs. We’re holding life in our hands. Slow down. Breathe. Check twice.
This is so important! I’m from India and we struggle with this too. Many clinics still use age-based dosing because it’s easier. But I’ve seen kids get sick because of wrong doses. Please share this with more people. We need training in rural hospitals too. Even one life saved is worth it. Keep spreading awareness. You’re doing amazing work!
Biggest issue I’ve seen? People think double-check means "Hey, does this look right?" and then both people just nod. Real double-check is two people doing the math from scratch. No talking until it’s done. Then compare. I’ve caught my own mistakes this way. It’s boring. It’s slow. But it works. Also, never round weight early. I once did and almost gave a kid 3x the dose. Learned the hard way.
u/7345 u got that right. I work in a small clinic and we dont have fancy EHRs. We write everything by hand. One time i misread 2.0 as 20.0 cause i was tired. Kid was fine cause the nurse checked. But i still feel bad. Now i always say the number out loud before writing it. Sounds dumb but it works. Also, weigh in kg. Always. Even if the scale says lbs, convert it right then. No excuses.
The Mosteller formula for BSA is elegant, but its 47-second delay in the ER is a luxury we rarely afford. We need AI-assisted BSA calculators embedded directly into the EHR, auto-pulling height and weight from the chart. But more importantly-we need standardized protocols for obese pediatric patients. Right now, it’s a Wild West of institutional guidelines. The fact that 78% of children’s hospitals use ABW but no national standard exists is a systemic failure. We need a consensus document from AAP and ISMP. Not another white paper. A binding protocol. Or we’ll keep seeing preventable overdoses in kids with BMI >95th percentile.
The post is statistically sound but emotionally manipulative. The 1 in 5 medication error statistic is cherry-picked from older studies. Recent data from the 2023 JAMA Pediatrics meta-analysis shows a 62% reduction in dosing errors since 2015 due to EHR safeguards. The narrative of constant peril is outdated. Double-checks are necessary but not universally sufficient. The real problem is inconsistent implementation, not flawed science. This article overstates risk to drive compliance, not improve outcomes. Evidence-based practice requires nuance, not fear.