SNRI Side Effect Calculator
How this tool works
This calculator estimates the likelihood of common SNRI side effects based on the medication you're taking, your age, gender, and current symptoms. Remember, these are general estimates - your experience may vary. Always consult your doctor for medical advice.
Tell us about your situation
When it comes to treating depression, especially when it comes with chronic pain or fatigue, SNRI medications are often one of the first options doctors consider. Unlike older antidepressants that only target serotonin, SNRIs-Serotonin-Norepinephrine Reuptake Inhibitors-work on two key brain chemicals at once. This dual action makes them uniquely useful for people who struggle with both low mood and physical symptoms like body aches, nerve pain, or low energy. But knowing how they work isn’t enough. You need to understand what to expect when taking them, especially the side effects that can make or break your experience.
What Are SNRIs and How Do They Work?
SNRIs are a class of antidepressants that stop the brain from reabsorbing serotonin and norepinephrine. These are neurotransmitters that help regulate mood, focus, and even pain signals. By keeping more of these chemicals active in the spaces between nerve cells, SNRIs help improve communication in brain circuits linked to emotion and physical sensation.
The first SNRI approved was venlafaxine (Effexor) in 1993. Since then, others like duloxetine (Cymbalta), desvenlafaxine (Pristiq), levomilnacipran (Fetzima), and milnacipran (Savella) have joined the list. Each one has slightly different strengths. For example, duloxetine and desvenlafaxine lean more heavily on serotonin, while levomilnacipran and milnacipran have a stronger effect on norepinephrine. This matters because norepinephrine plays a bigger role in energy and pain control. That’s why duloxetine is approved not just for depression, but also for diabetic nerve pain, fibromyalgia, and chronic back pain. Venlafaxine, on the other hand, is often used for depression and anxiety disorders like social anxiety or panic attacks.
What sets SNRIs apart from SSRIs (like sertraline or fluoxetine) is this dual mechanism. SSRIs only boost serotonin, which helps with mood and anxiety but doesn’t always touch physical pain. SNRIs do. That’s why they’re often chosen when someone has both depression and long-term pain-something that’s surprisingly common. Studies show up to 40% of people with major depression also report chronic pain symptoms.
Common Side Effects: What Most People Experience
Like all medications, SNRIs come with side effects. Not everyone gets them, and many fade after a few weeks. But knowing what to expect can help you decide whether to stick with the treatment or talk to your doctor about alternatives.
- Nausea: This is the most common side effect, especially with duloxetine. Around 25-30% of users feel queasy in the first week. Taking the pill with food helps a lot.
- Sexual side effects: About 20-40% of people report lower libido, trouble getting aroused, or delayed orgasm. It’s one of the most frustrating side effects, and it doesn’t always improve over time.
- Dizziness and lightheadedness: Especially in the first few days. Standing up slowly can help prevent this.
- Sweating: More common with duloxetine-about 20% of users notice increased sweating, even when it’s not hot.
- Dry mouth: Reported in about 30% of venlafaxine users. Chewing sugar-free gum or sipping water helps.
- Constipation: Affects about 15% of users across all SNRIs. Increasing fiber and water intake can ease this.
Many people start with mild nausea and dizziness, but these usually get better after 2-4 weeks. If they don’t, it’s worth discussing a dose adjustment or switching meds. A 2023 review of patient forums found that 45% of duloxetine users said nausea disappeared completely after a month.
More Serious Side Effects: What You Need to Watch For
While most side effects are manageable, some require immediate attention.
Serotonin syndrome is rare but dangerous. It happens when too much serotonin builds up in the brain-usually from combining SNRIs with other serotonergic drugs like tramadol, certain migraine meds, or even St. John’s Wort. Symptoms include confusion, rapid heartbeat, high fever, muscle stiffness, and seizures. If you notice any of these, get medical help right away. The risk is low-about 0.5 to 1 case per 1,000 people per year-but it’s serious.
Bleeding risk is another concern. SNRIs affect serotonin in platelets, which can make it harder for blood to clot. This increases the chance of bruising easily, nosebleeds, or bleeding during surgery. If you’re on blood thinners like warfarin or aspirin, your doctor should monitor this closely.
Blood pressure spikes are most common with venlafaxine, especially at doses over 150mg per day. About 12-15% of users at these higher doses develop high blood pressure. That’s why doctors usually check your BP before starting and again after a few weeks. If your systolic pressure goes above 140 or diastolic above 90, they may lower your dose or switch you.
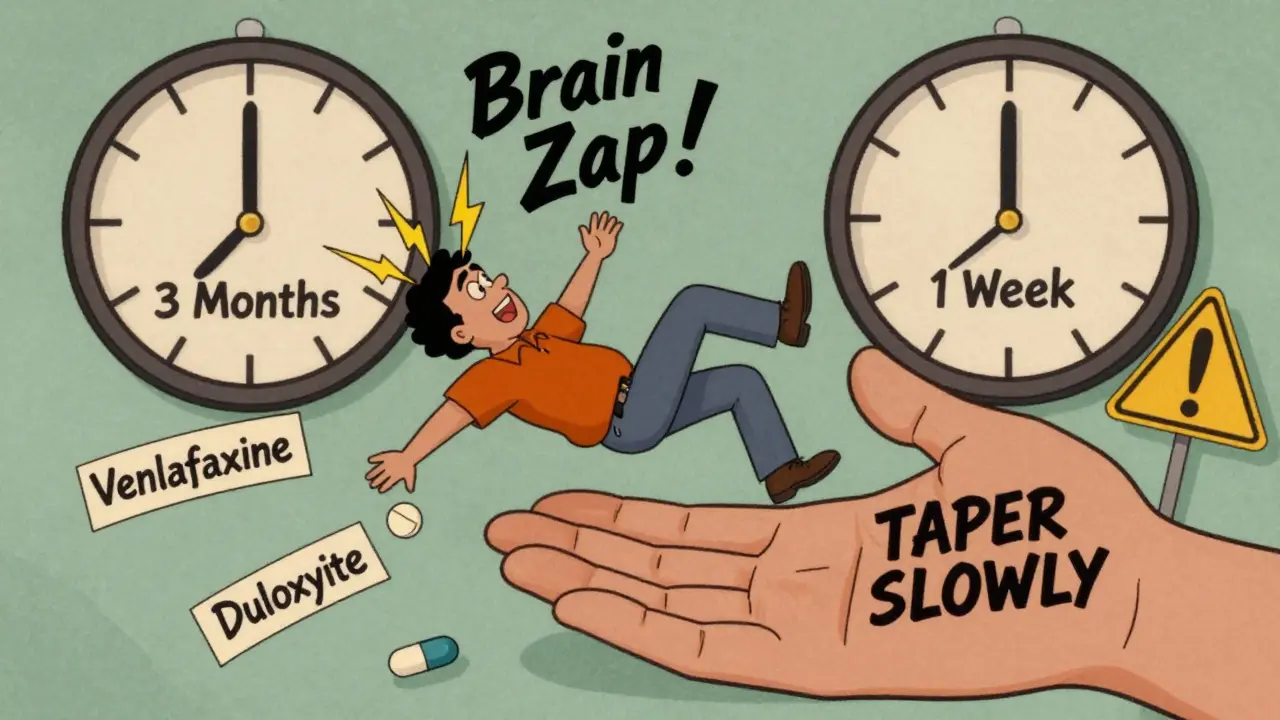
Discontinuation syndrome is one of the biggest challenges with SNRIs. If you stop suddenly-miss a dose, run out of pills, or quit cold turkey-you could get brain zaps, dizziness, nausea, insomnia, or even flu-like symptoms. Up to 50% of people who quit without tapering experience this. Venlafaxine users are especially prone to this, with 54% reporting what they call the “venlafaxine cliff”-a sudden, intense drop in mood and physical well-being after missing just one dose. The fix? Never stop abruptly. Always taper down slowly over 2-4 weeks under medical supervision.

How SNRIs Compare: Venlafaxine vs. Duloxetine vs. Others
Not all SNRIs are the same. Here’s how the most common ones stack up:
| Medication | Primary Use | Typical Starting Dose | Max Dose | Key Side Effects | Special Notes |
|---|---|---|---|---|---|
| Venlafaxine | Depression, anxiety disorders | 37.5 mg/day | 225 mg/day | High BP, sweating, discontinuation symptoms | Higher risk of hypertension above 150 mg/day; metabolite helps prolong effect |
| Duloxetine | Depression, fibromyalgia, nerve pain | 30 mg/day | 120 mg/day | Nausea, dry mouth, weight changes | First SNRI approved for multiple pain conditions; 37% of users report initial weight loss |
| Desvenlafaxine | Depression | 50 mg/day | 100 mg/day | Nausea, dizziness, insomnia | Active metabolite of venlafaxine; less variation in blood levels |
| Levomilnacipran | Depression | 20 mg/day | 120 mg/day | Increased heart rate, high BP | Most norepinephrine-focused; may help with fatigue more than other SNRIs |
| Milnacipran | Fibromyalgia | 12.5 mg/day | 100 mg/day | Nausea, high BP, headache | Only approved for fibromyalgia in the U.S.; not used for depression |
Choosing between them depends on your symptoms. If you have depression plus nerve pain, duloxetine is often the go-to. If anxiety and low energy are your main issues, venlafaxine might be better. Levomilnacipran is newer and often chosen for people who feel drained or sluggish-its stronger norepinephrine boost can help with motivation. Milnacipran is rarely used unless fibromyalgia is the primary concern.
Real-World Experiences: What Patients Say
Online forums and patient reviews paint a mixed picture. On Reddit and Drugs.com, users describe venlafaxine as a “life-saver” for mood and energy-but also a “nightmare” to quit. One user wrote: “It lifted my depression faster than anything else. But when I missed a dose, I felt like I was dying. Took me three months to taper off.”
Duloxetine users often praise its pain relief. “I had back pain for years. No NSAIDs worked. Duloxetine cut it in half,” said one patient. But many also mention the nausea. “First week, I couldn’t eat. Second week, it got better. Worth it,” said another.
Sexual side effects are the most consistent complaint across all SNRIs. About 65% of users report reduced libido or difficulty reaching orgasm. Some say it’s worse than the depression itself. A few report improvement after switching to bupropion (Wellbutrin), which doesn’t affect sexual function.
Weight changes are unpredictable. Some lose 5-7 pounds in the first few months, then gain it back. Others gain weight slowly over time. There’s no clear pattern, but it’s something to monitor.
What to Expect When Starting an SNRI
If your doctor prescribes an SNRI, here’s what usually happens:
- You start low: Usually 30-37.5 mg per day to minimize side effects.
- You wait 2-4 weeks: It takes time for the brain to adjust. Don’t expect immediate results.
- You monitor side effects: Keep a simple log-nausea, sleep, mood, energy.
- You increase slowly: Doses go up every 1-2 weeks until you hit the right level.
- You get checked: Blood pressure, liver function, and mental state are monitored.
- You don’t quit suddenly: Even if you feel better, tapering is non-negotiable.
Most people see mood improvements after 4-6 weeks. Pain relief can take longer-up to 8-12 weeks. Patience is key. If side effects are unbearable after 4 weeks, talk to your doctor. There’s no shame in switching. What works for one person might not work for another.
Who Should Avoid SNRIs?
SNRIs aren’t right for everyone. Avoid them if you:
- Have uncontrolled high blood pressure
- Are taking MAO inhibitors (like phenelzine) or stopped them in the last 14 days
- Have liver disease or severe kidney problems
- Have a history of seizures or eating disorders
- Are pregnant or breastfeeding-data is limited, and risks aren’t fully understood
Also, if you’ve had a bad reaction to one SNRI, you’re more likely to react badly to others. But it’s not guaranteed-some people tolerate one but not another.
The Bigger Picture: Are SNRIs Worth It?
SNRIs aren’t magic pills. Depression isn’t just a chemical imbalance-it’s complex, involving stress, sleep, inflammation, and life circumstances. But for many, SNRIs offer real relief where other treatments failed.
They’re especially helpful for people with depression and chronic pain, fatigue, or anxiety. Their ability to target both mood and physical symptoms makes them unique. And unlike older antidepressants, they’re generally safer for the heart and less likely to cause drowsiness or dry mouth.
Still, they come with trade-offs. Sexual side effects, discontinuation risks, and blood pressure concerns mean you need to be informed and involved in your care. Don’t just take the pill and hope for the best. Track your symptoms. Talk to your doctor. Ask questions. If one SNRI doesn’t work, another might.
With over 22 million prescriptions for venlafaxine alone in the U.S. each year, these drugs are far from rare. They’re a tool-and like any tool, they work best when used with awareness, not ignorance.
Can SNRIs cause weight gain?
Some people lose weight at first-especially with duloxetine-then gain it back over time. Others gain weight slowly. There’s no clear pattern, but it’s common enough that doctors monitor it. Weight changes are usually mild, but if they’re bothersome, talk to your provider. Switching to bupropion or adjusting your diet and activity level can help.
How long does it take for SNRIs to work?
Mood improvements usually start after 2-4 weeks, but full effects take 6-8 weeks. Pain relief can take even longer-up to 12 weeks. Don’t give up too soon. If side effects are too strong, talk to your doctor about lowering the dose or switching.
Is venlafaxine more addictive than other SNRIs?
SNRIs aren’t addictive in the way opioids or benzodiazepines are. But venlafaxine has a very short half-life, meaning it leaves your system quickly. That’s why people experience severe withdrawal symptoms if they miss a dose or stop suddenly. It’s not addiction-it’s physical dependence. Tapering slowly prevents this.
Can I drink alcohol while on SNRIs?
It’s not recommended. Alcohol can worsen dizziness, drowsiness, and depression symptoms. It also increases the risk of liver problems and can make side effects like nausea worse. Even moderate drinking isn’t safe when you’re on an SNRI. If you drink, talk to your doctor about whether it’s safe for you.
Are SNRIs safe during pregnancy?
Data is limited. Some studies suggest a small increased risk of complications like preterm birth or persistent pulmonary hypertension in newborns. But untreated depression also carries risks. If you’re pregnant or planning to be, talk to your doctor. They’ll weigh the risks of medication versus the risks of not treating your depression.
Do SNRIs work better than SSRIs?
For depression alone, the difference is small. But if you have pain, fatigue, or anxiety alongside depression, SNRIs often work better. That’s why they’re preferred for fibromyalgia, diabetic nerve pain, or chronic back pain. For pure anxiety or mild depression, SSRIs are still first-line because they’re easier to tolerate.
If you’re considering an SNRI, remember: you’re not alone. Millions have walked this path. The key is to stay informed, communicate with your doctor, and give the medication time to work-while watching for red flags. With the right approach, SNRIs can be a turning point.








![Endep (Amitriptyline) Uses, Dosage, Side Effects, and Safety in Australia [2025]](/uploads/2025/08/thumbnail-endep-amitriptyline-uses-dosage-side-effects-and-safety-in-australia.webp)
Okay but like… I took venlafaxine for 8 months and it turned me into a sweating, zapped-out zombie who cried during cereal commercials. 🥲 I didn’t even know I could cry over Frosted Flakes. Tapering was hell. Like, I missed one dose and felt like I’d been hit by a truck made of regret. Worth it? Maybe. Would I do it again? Nah. Send help.
How quaint-another armchair neuropharmacology treatise, complete with bullet points and a table. Did you even read the primary literature? The 2023 meta-analysis by Fava et al. demonstrated that SNRI efficacy over placebo is clinically negligible when corrected for publication bias. And yet, here we are, treating depression like it’s a firmware update. Pathetic. Also, ‘brain zaps’? That’s not a medical term. It’s a TikTok symptom.
For anyone starting an SNRI: be patient. The first two weeks suck. But if you stick with it, your body adjusts. Keep a journal. Talk to your doctor. And if nausea hits hard-take it with food. Seriously. It makes a difference. You got this.
Ohhh so duloxetine helps with pain? Wow. I guess that’s why my spine is now a disco ball of nerve zaps. 🤡 Maybe next they’ll tell me serotonin fixes my existential dread. Oh wait-it’s already trying. And failing. Hard.
hey i just started venlafaxine and i think i might be having serotonin syndrome?? my heart is racing and i feel like my skin is on fire?? idk if this is normal or if i should go to er??
From a clinical perspective, the pharmacokinetic profile of levomilnacipran makes it uniquely suited for patients with anhedonia and psychomotor retardation-particularly those with elevated baseline fatigue scores on the MADRS. Its noradrenergic selectivity (>10:1 vs. serotonergic) enhances cortical arousal without the same degree of autonomic side effects seen with venlafaxine. That said, hepatic metabolism via CYP2D6 means poor metabolizers may need dose titration. Monitor liver enzymes and HR. Also-always taper. Don’t be that person.
My mom took duloxetine for fibromyalgia. Nausea was bad at first, but after a month, her pain dropped by 60%. She still takes it. No side effects now. It’s not perfect, but it helped.
They don’t want you to know this… but SNRIs are part of the pharmaceutical deep state’s plan to keep us docile. 🕵️♂️ The FDA approves them because they want us dependent on chemicals while the real causes-EMFs, fluoride, 5G, and soul-sucking capitalism-are ignored. My cousin quit SNRIs and started doing cold showers and grounding. Now she’s ‘unplugged’ and says her mood is ‘naturally regulated.’ I’m not saying… but have you checked your EMF meter lately?